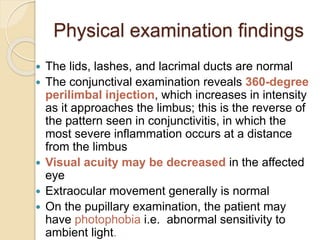
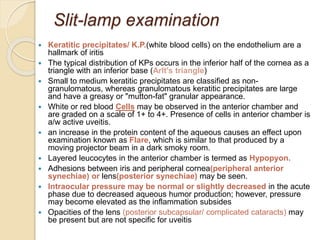
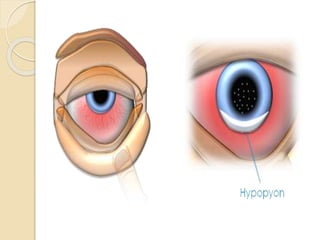
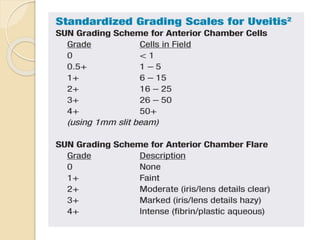
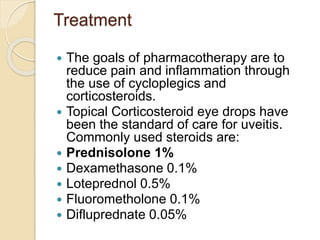
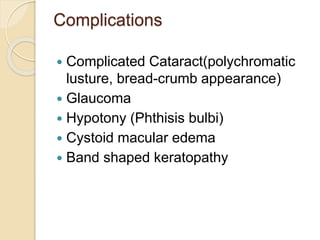
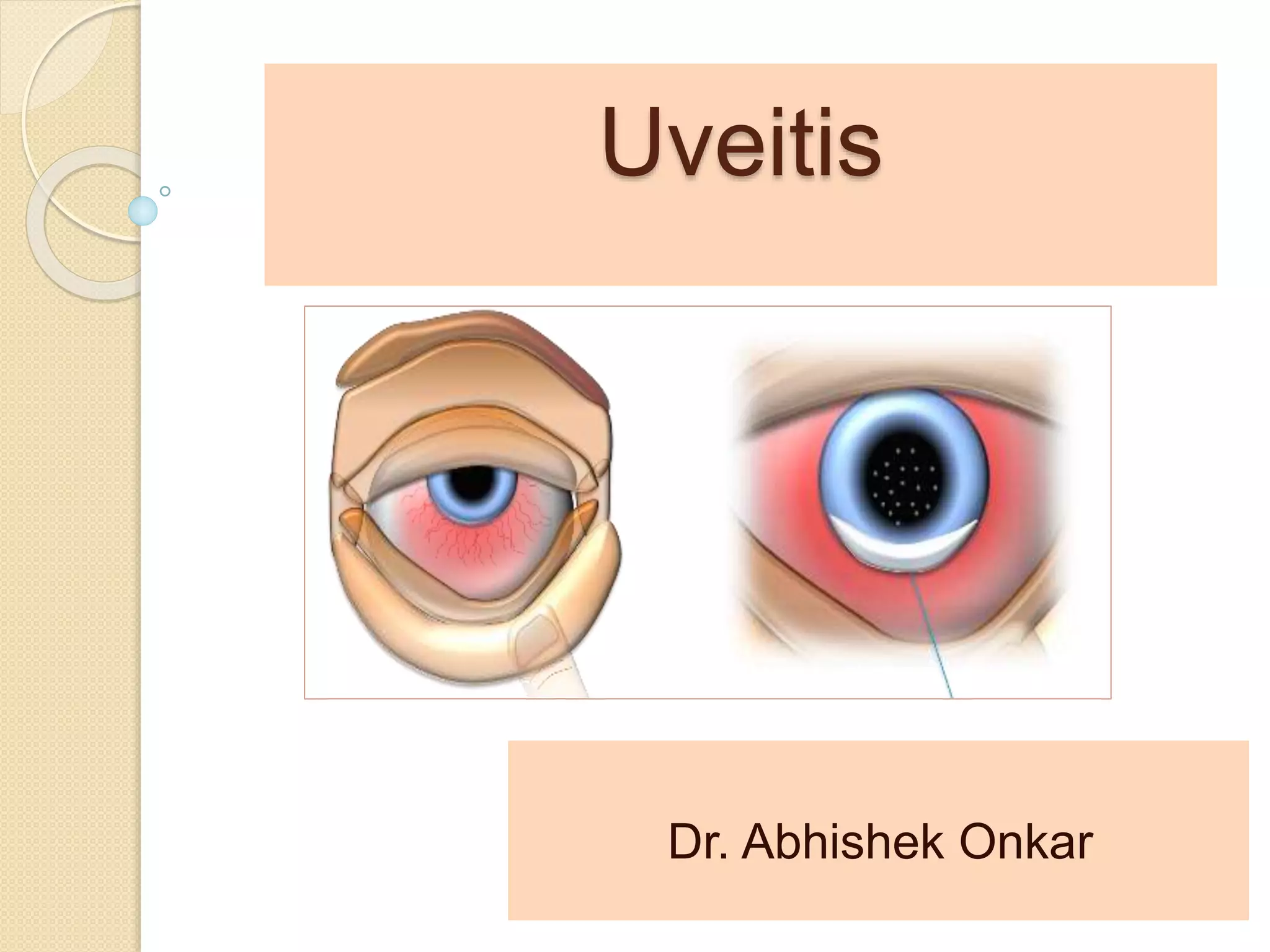
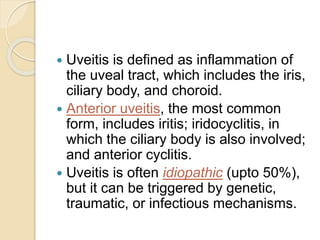
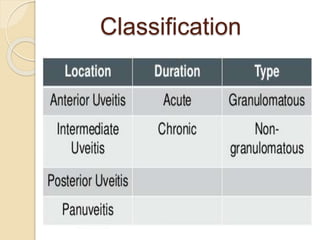
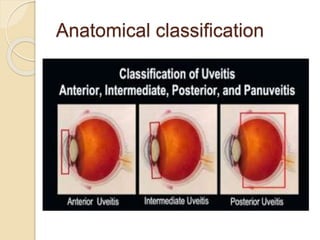
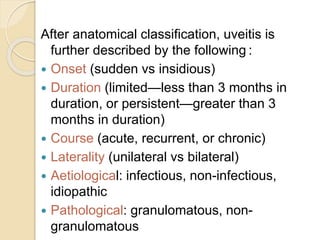
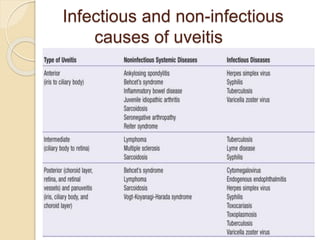
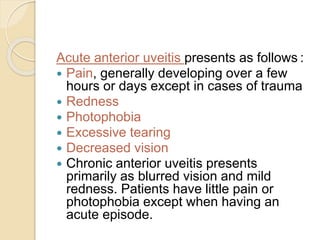
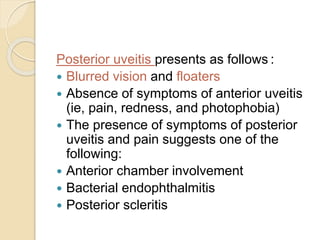
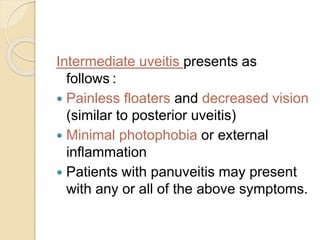
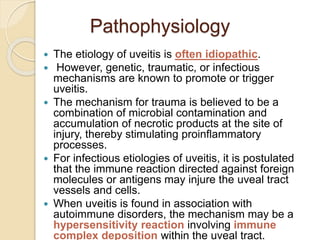
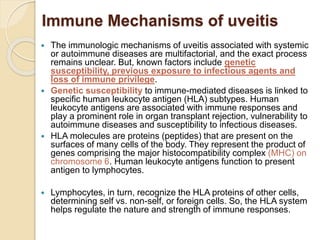
Uveitis is inflammation of the uveal tract of the eye. It can be idiopathic or caused by infection or autoimmune conditions. Anterior uveitis is the most common type, involving the iris and sometimes the ciliary body. Uveitis is classified based on location and course of inflammation. Symptoms vary depending on location but can include eye pain, redness, photophobia, blurred vision, and floaters. Treatment focuses on reducing inflammation with corticosteroid eye drops. Complications can include glaucoma, cataracts, and vision loss if not properly treated.
![Epidemiology
Incidence and prevalence:
The incidence of uveitis varies from 14 to 52.4/100,000 with
the overall prevalence around the world is up to 0.73%
Race
Racial predisposition to uveitis is related to the patient's
underlying systemic disease.[3]
Caucasian: HLA-B27, multiple sclerosis
African American: Sarcoidosis, SLE
Mediterranean/Middle Eastern: Behçet's disease
Asian: Behçet's disease
Sex
In general, uveitis does not have a gender predisposition
except in cases secondary to systemic disease, such as JRA
and SLE.
Age
The majority of patients are aged 20-50 years.](https://image.slidesharecdn.com/uveitisbasicsforundergrads-150322061025-conversion-gate01/85/Uveitis-basics-for-undergrads-15-320.jpg)