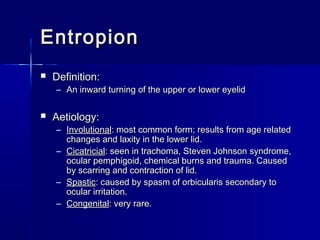
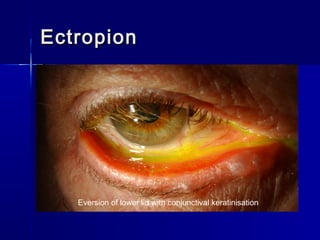
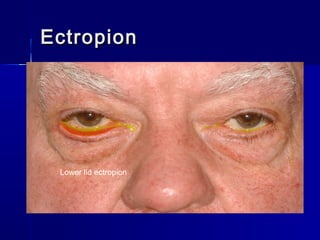
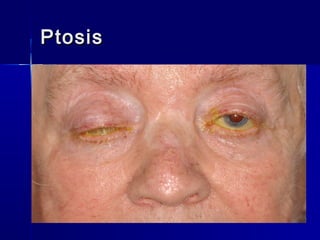
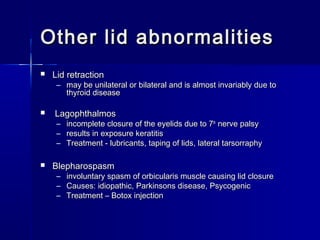
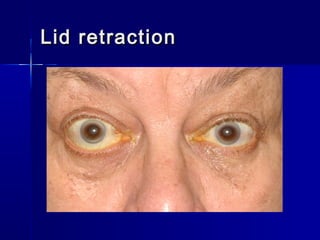
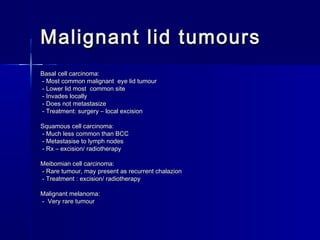
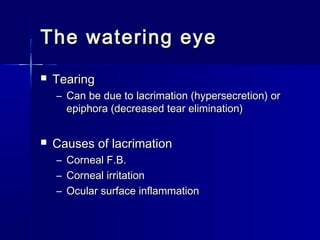
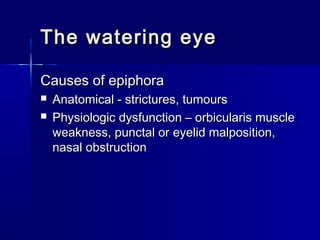
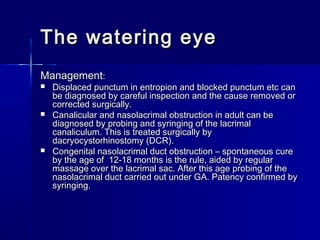
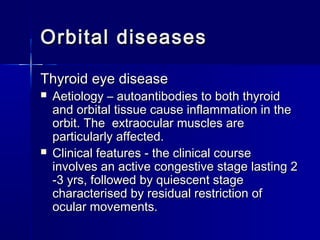
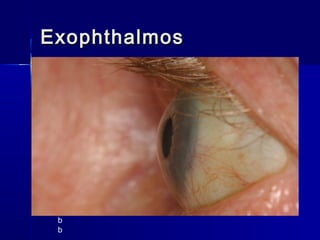
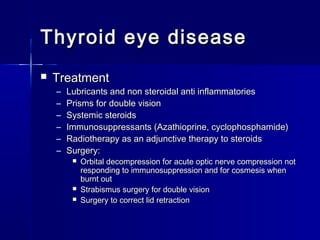
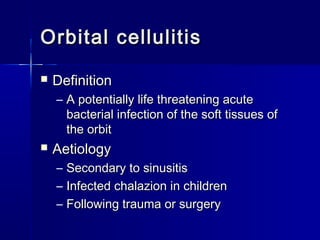
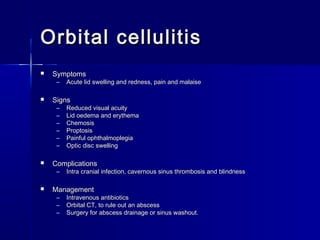
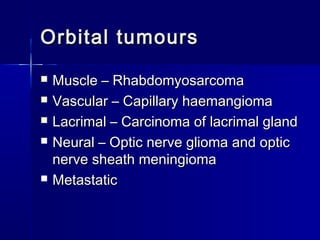
This document discusses various diseases and conditions of the eyelids, lacrimal system, and orbit. It covers eyelid malpositions like entropion, ectropion, ptosis, and lagophthalmos. It also discusses eyelid inflammation conditions like blepharitis. Non-neoplastic lid lesions, benign and malignant lid tumors are described. The lacrimal system anatomy and tear production/drainage is briefly explained. Finally, it discusses orbital diseases like thyroid eye disease which can cause proptosis, double vision, and restricted eye movements.