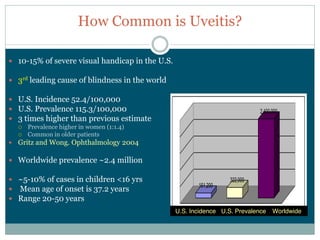
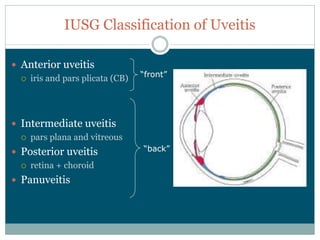
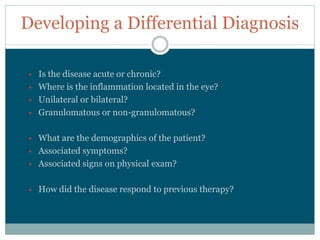
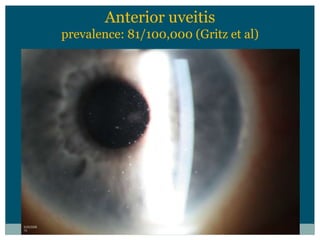
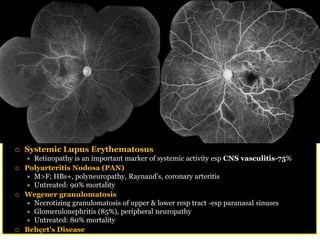
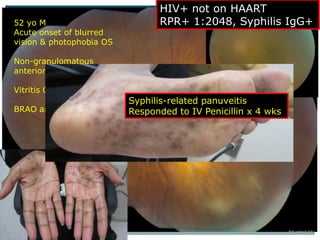
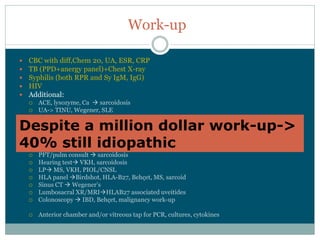
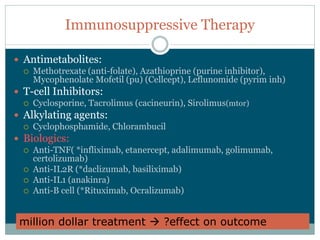
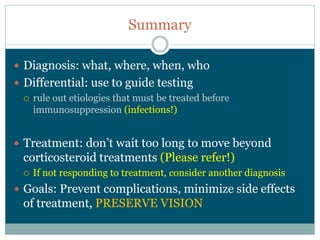
Uveitis is an intraocular inflammation that can lead to vision loss and is a significant cause of blindness worldwide. Various classifications and grading systems are used to diagnose and categorize uveitis, with treatment options including corticosteroids and immunosuppressive therapies. Understanding the underlying causes and identifying the specific type of uveitis is critical for appropriate management and improving patient outcomes.