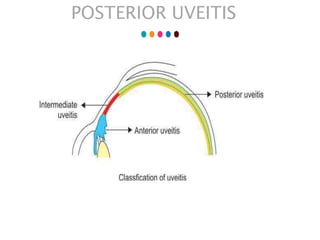
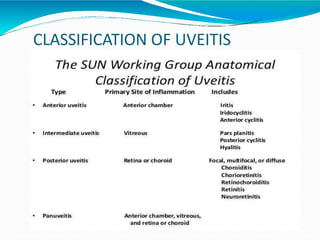
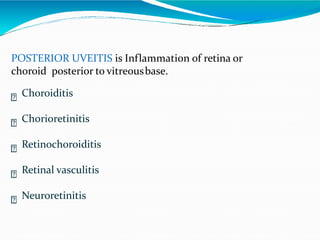
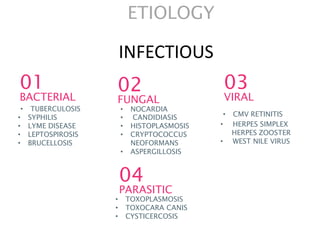
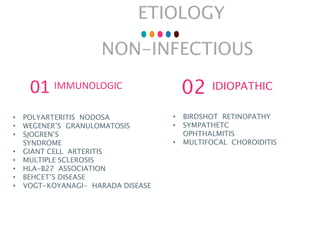
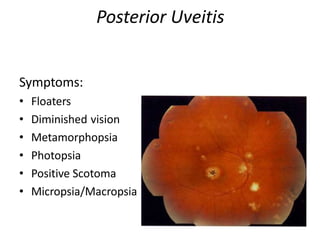
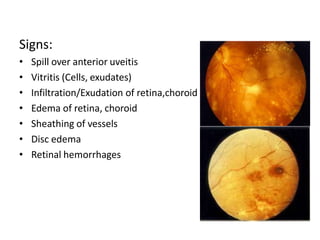
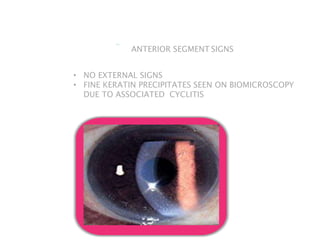
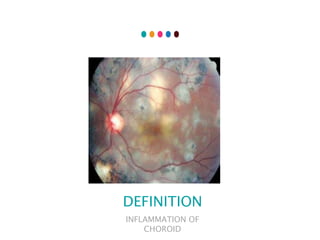
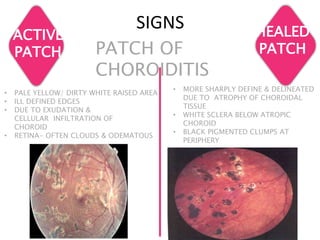
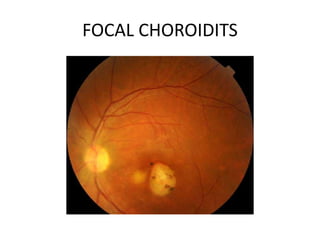
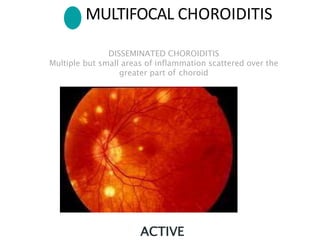
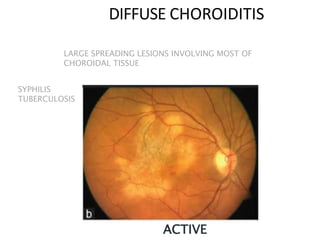
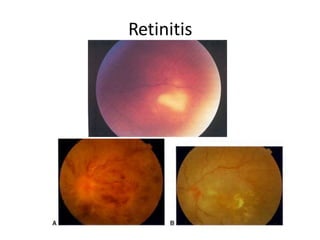
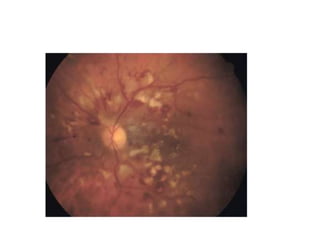
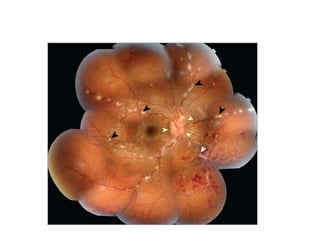
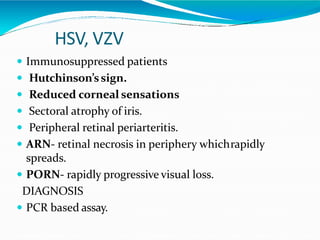
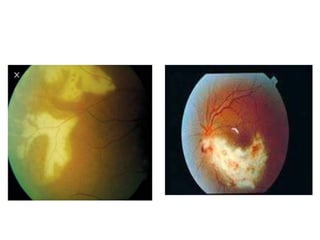
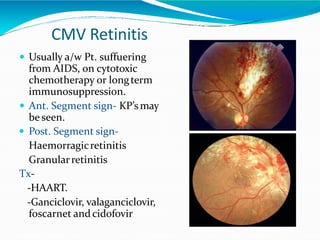
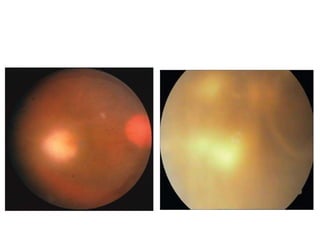
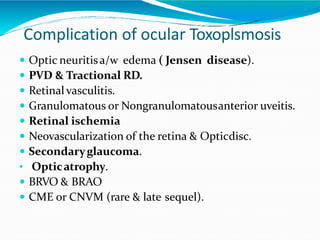
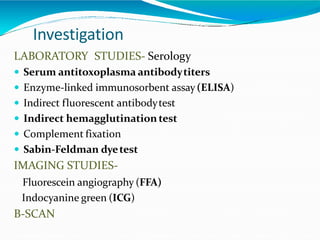
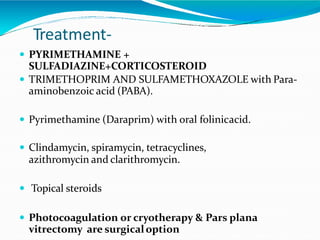
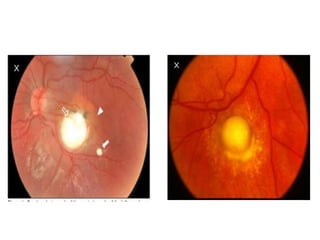
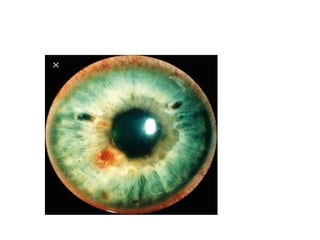
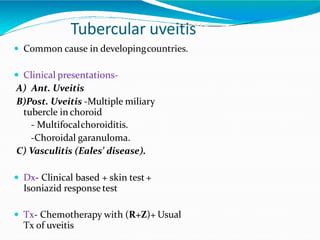
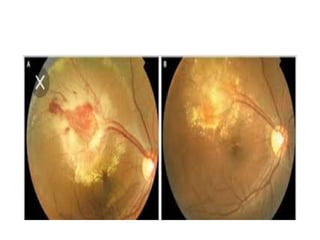
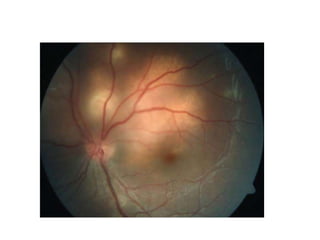
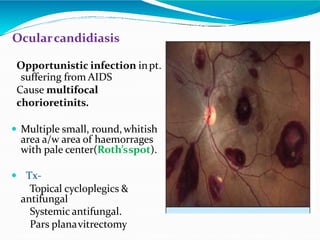
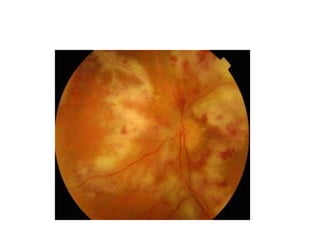
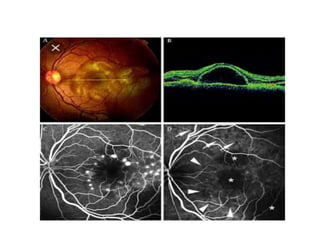
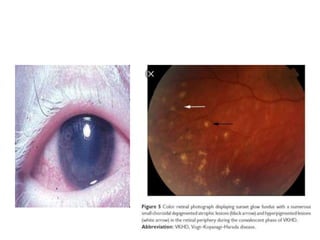
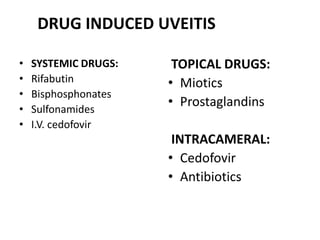
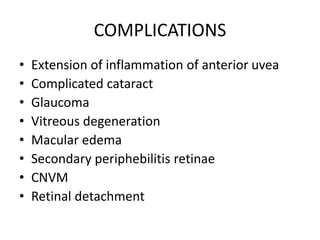
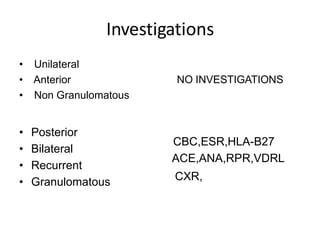
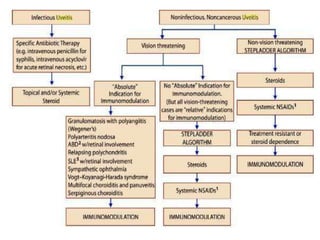
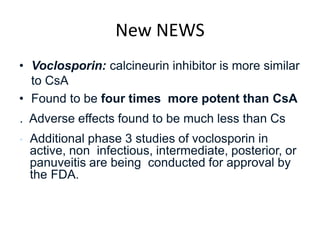
The document provides a comprehensive guide on posterior uveitis, detailing its classification, symptoms, signs, and differential diagnoses, including infectious and non-infectious etiologies. It outlines diagnostic criteria, investigative approaches, and treatment options such as corticosteroids, immunosuppressants, and specific therapies based on underlying causes. Furthermore, it discusses complications and the relevance of laboratory and imaging studies in managing posterior uveitis.