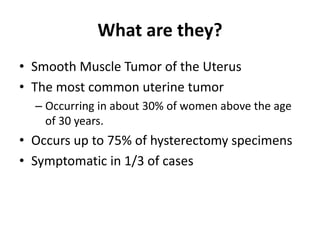
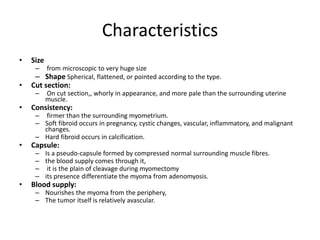
Uterine fibroids are benign smooth muscle tumors of the uterus that are very common. They occur in around 30% of women over 30 years of age. Symptoms include heavy bleeding, pelvic pressure, pain, and infertility. Treatment options depend on symptoms and desire for future fertility, and include medical management, myomectomy (surgical removal of fibroids), hysterectomy (removal of the uterus), uterine artery embolization, and newer minimally invasive procedures such as focused ultrasound and radiofrequency ablation. Complications can arise from degenerative changes, vascular changes, inflammation, or rarely malignant changes within the fibroids.
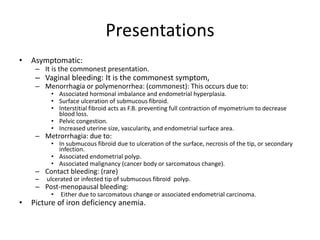
![• Discharge:
– Leucorrhea and mucoid discharge due to pelvic congestion.
– Muco-sanguinous discharge with ulcerated fibroid polyp.
– Muco-purulent discharge due to secondary infection.
• Swelling:
– Either abdominal swelling due to large fibroid or vaginal swelling due to a polyp.
• Infertility [in 5-10% of cases]:
– Most important is the underlying predisposing factor as anovulation and hormonal
disturbance.
– Broad ligamentary fibroid may stretch or distort the tubes.
– Corneal fibroids may obstruct the uterine end of the tube.
– S.M.F. acts as F.B. interfering with implantation.
– Cervical fibroid may obstruct the cervical canal.
– Associated endometriosis or endometrial hyperplasia.
• Pain: uncommon
– Intermittent colicky pain in submucous fibroid (acts as F.B. in the uterine cavity).
– Dull-aching pain and congestive dysmenorrhea due to pelvic congestion.
– Acute abdomen in red degeneration, torsion, ruptured vessel, and inflammation](https://image.slidesharecdn.com/fibroiduterus-151008060106-lva1-app6891/85/Fibroid-uterus-18-320.jpg)
![• Pressure symptoms
– Cervical fibroid:
• Anteriorly on the urethra causing acute retention of urine, or the
bladder causing frequency of micturition.
• Laterally on the ureters causing colic and back pressure on the
kidneys.
• Posteriorly on the rectum causing dyskasia, constipation, and sense
of incomplete defecation.
– Huge fibroid:
• On the pelvic veins causing edema, pain, and varicose veins in the
lower limbs.
• On the GIT causing distension and dyspepsia.
• On the diaphragm causing dyspnea.
• Spontaneous abortion:
– Before myomectomy [ 40%]
– 20% after myomectomy](https://image.slidesharecdn.com/fibroiduterus-151008060106-lva1-app6891/85/Fibroid-uterus-19-320.jpg)