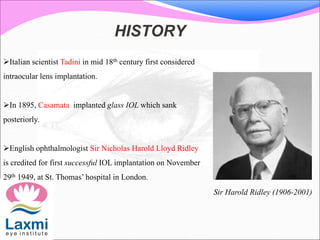
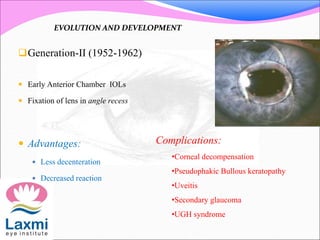
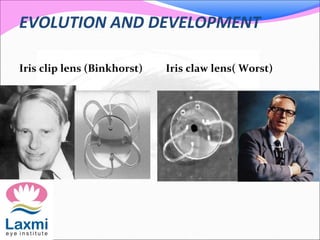
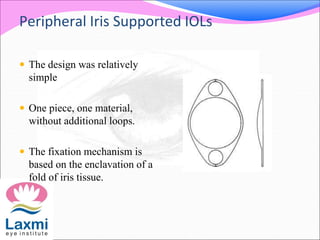
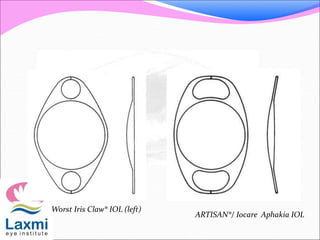
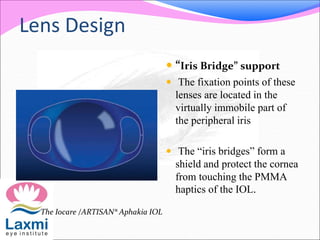
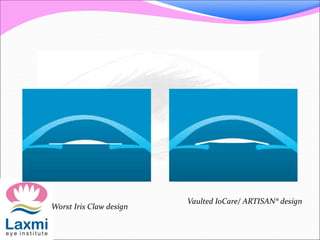
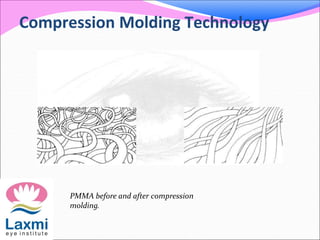
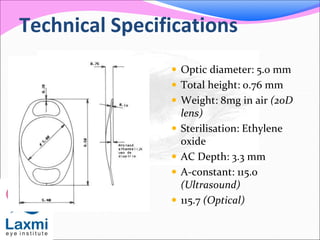
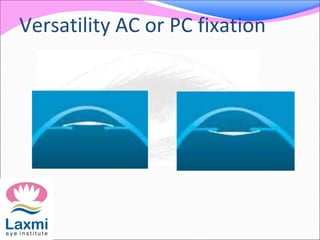
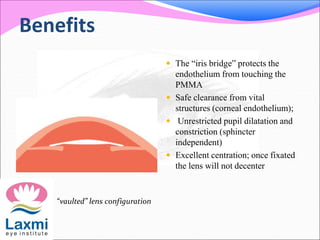
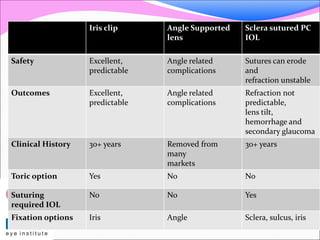
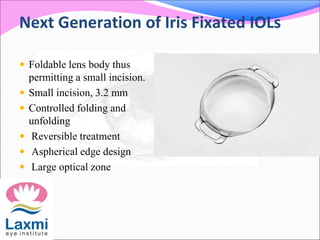
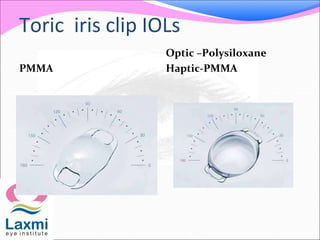
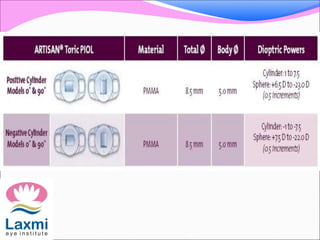
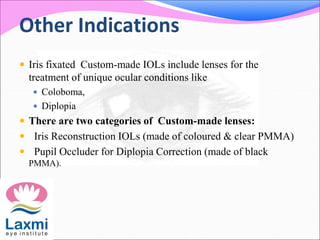
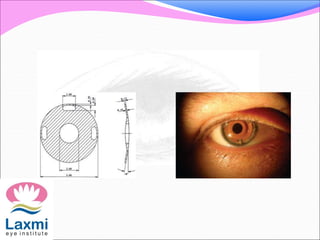
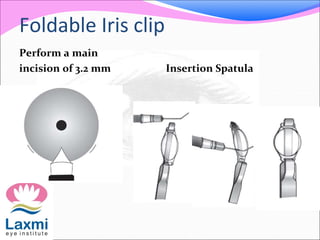
This document discusses the history and evolution of iris clip intraocular lenses (IOLs). It describes generations of IOL designs from 1949 to present day. Key developments include Binkhorst's iris clip lens in 1965 and Worst's iris claw lens in 1978, which pioneered iris fixation without sutures. Modern iris clip IOLs are made of PMMA or foldable materials, have vaulted designs for clearance, and fixate to the iris periphery for unrestricted pupil function. They are indicated for lens implantation in cases of cataract or aphakia.