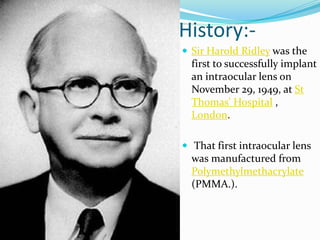
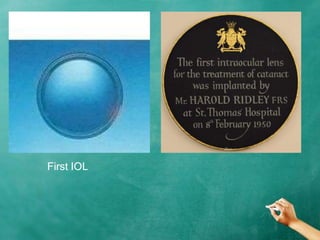
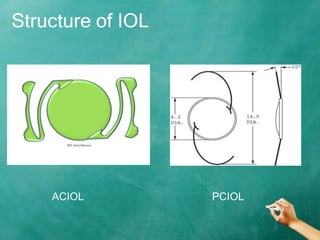
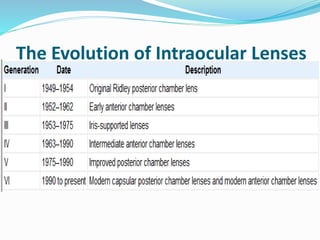
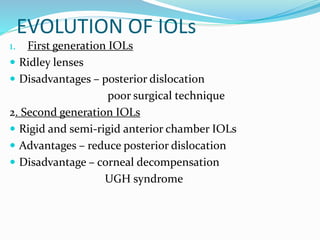
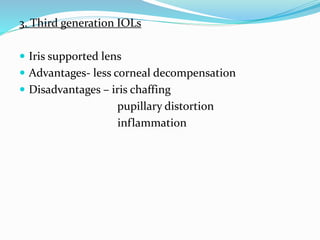
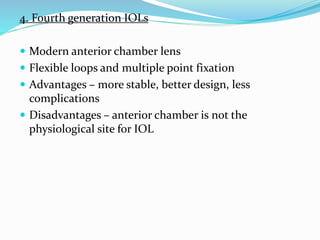
Sir Harold Ridley was the first to successfully implant an intraocular lens in 1949 using polymethylmethacrylate (PMMA). Early intraocular lenses had high complication rates of dislocation and glaucoma. The evolution of intraocular lens design led to foldable lenses made of silicone and acrylic materials that are implanted in the capsular bag for better stability and lower complication rates. Modern multifocal and toric intraocular lenses provide patients with independence from glasses by correcting presbyopia and astigmatism. Precise biometry and surgical technique are important for optimal outcomes with premium intraocular lenses.



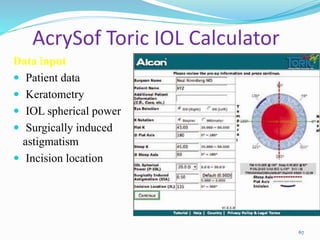
![TORIC IOL POWER CALCULATION
Precise keratometry
Surgically induced astgmatism [SIA].](https://image.slidesharecdn.com/iolneerajag-150916170923-lva1-app6891/85/Intra-Oular-Lenses-62-320.jpg)