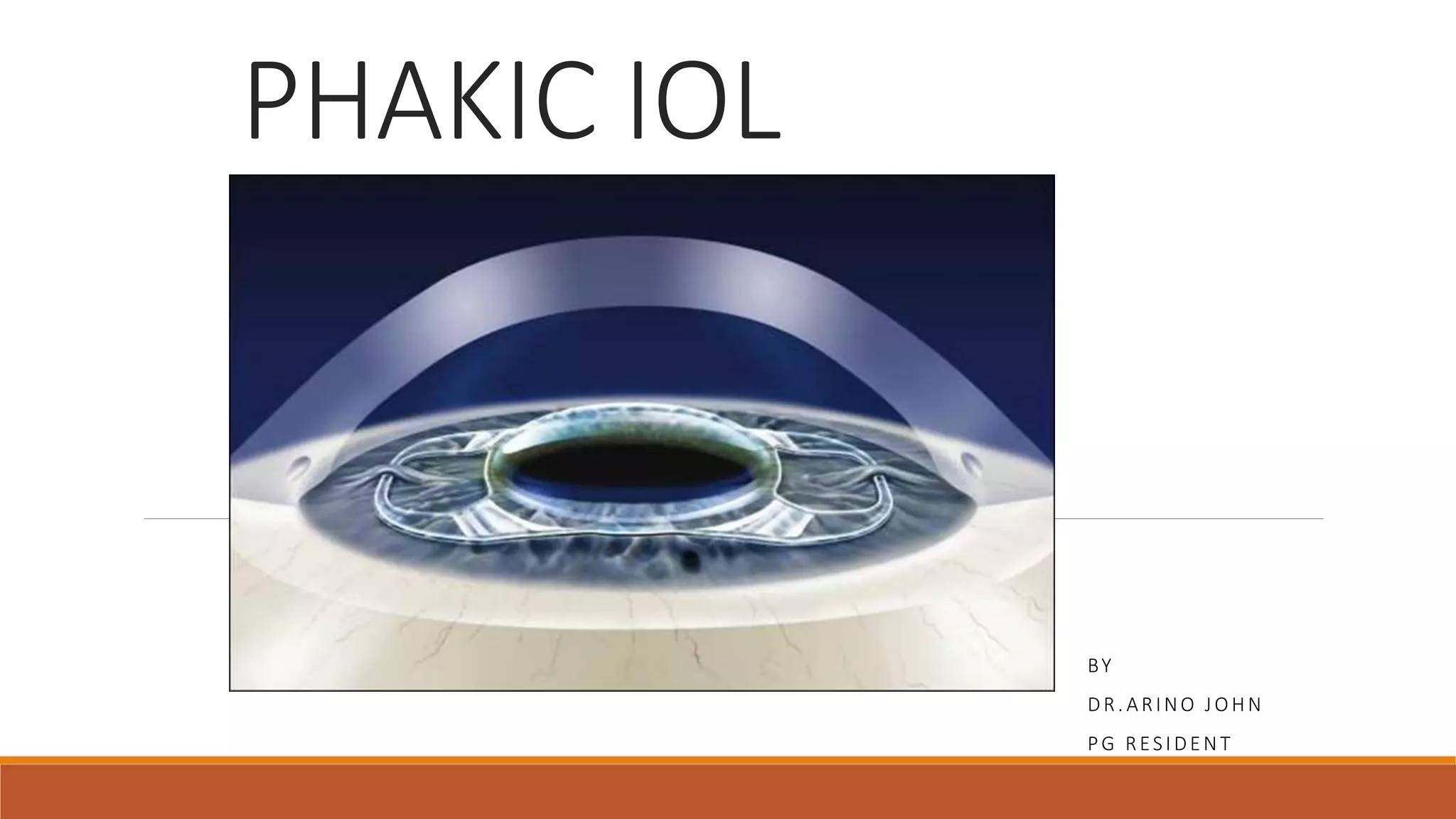
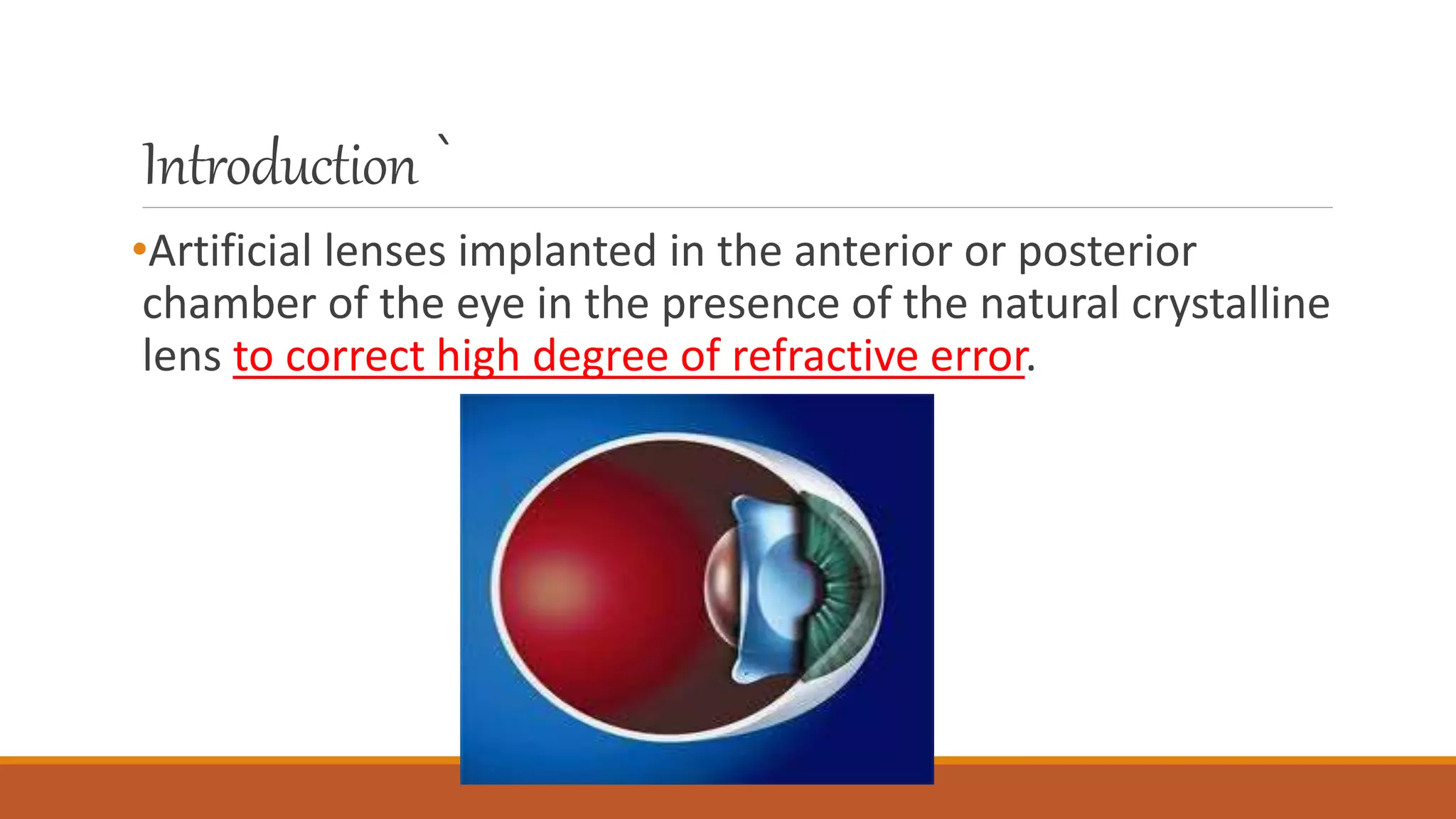
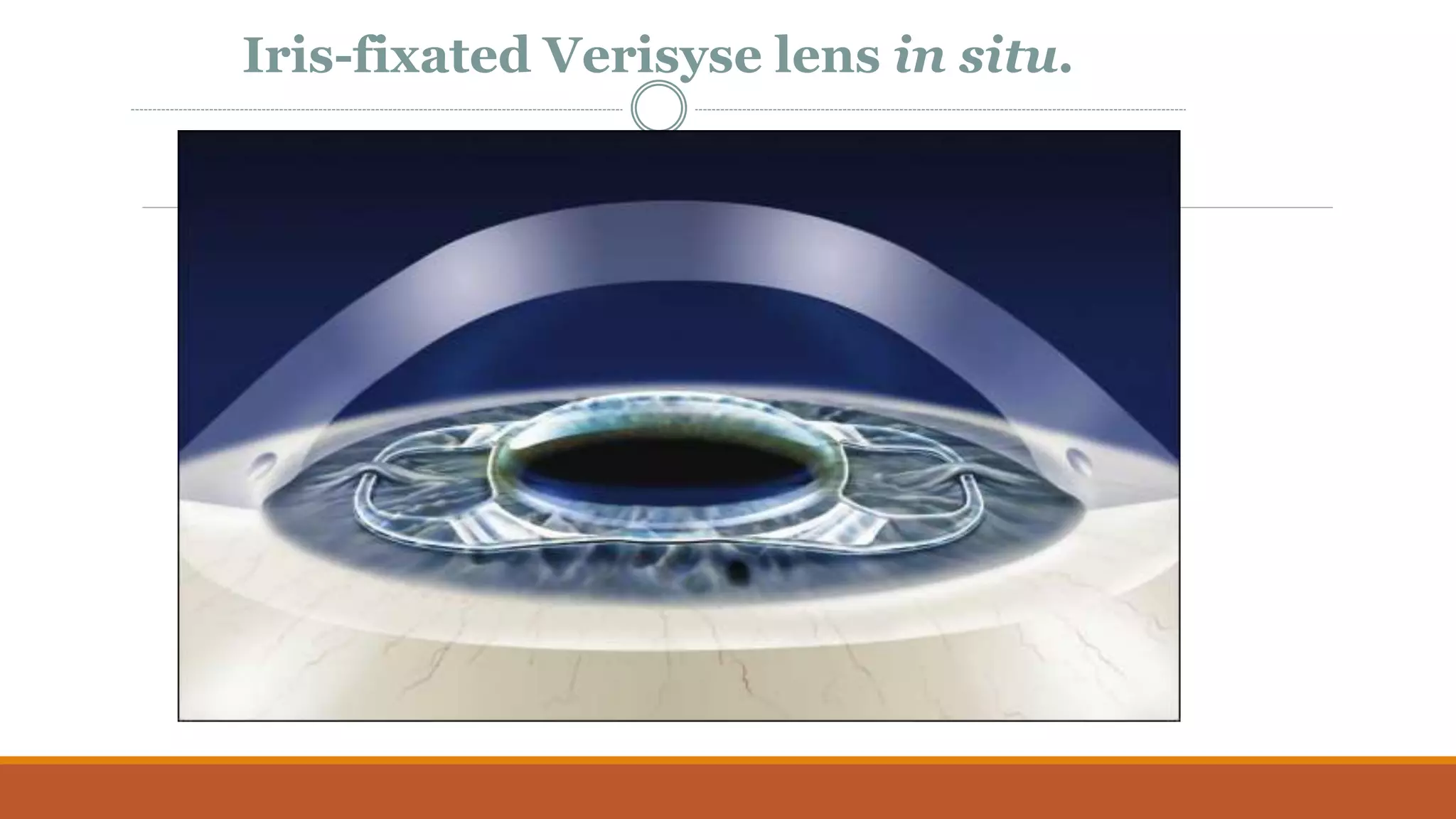
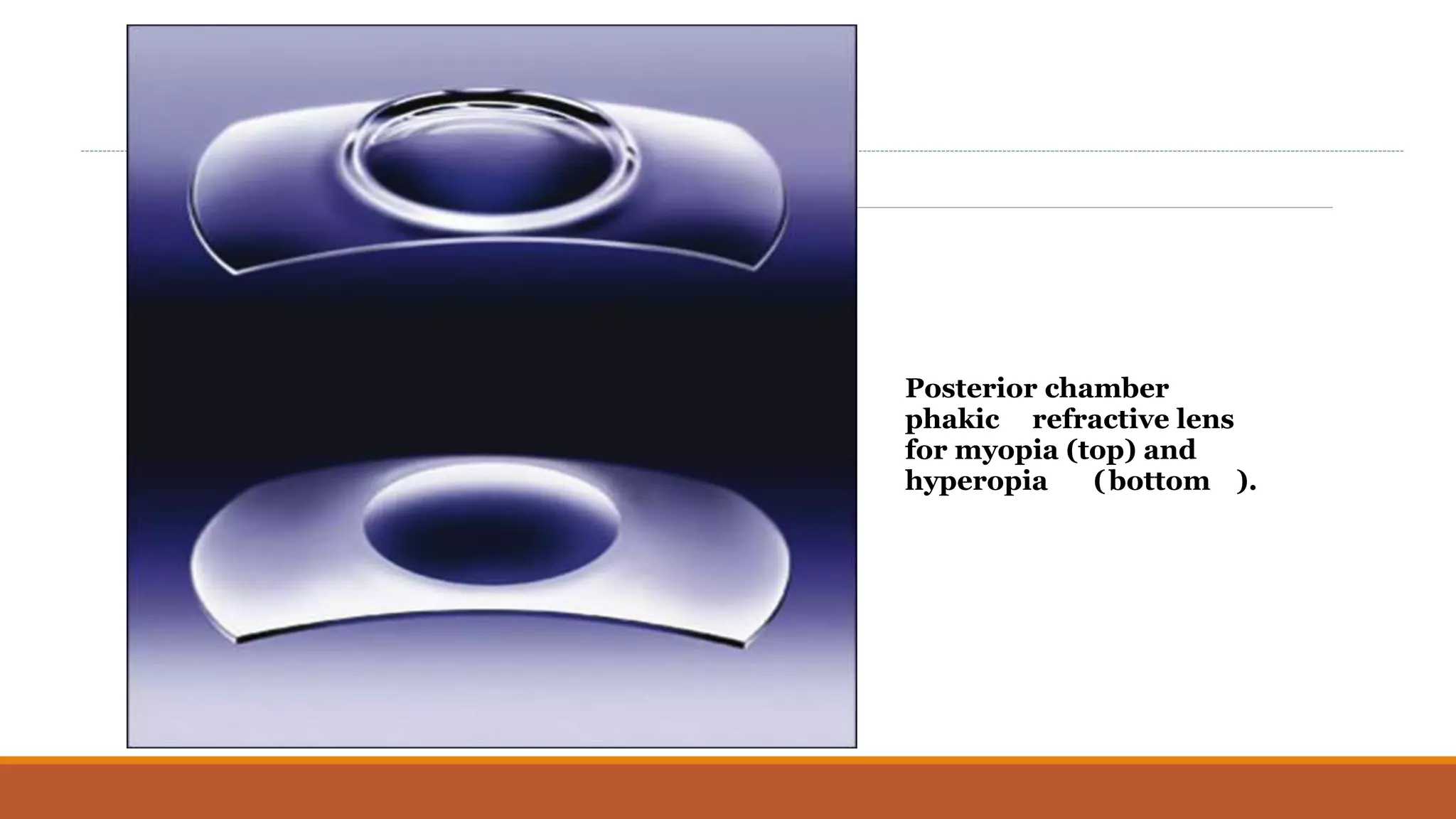
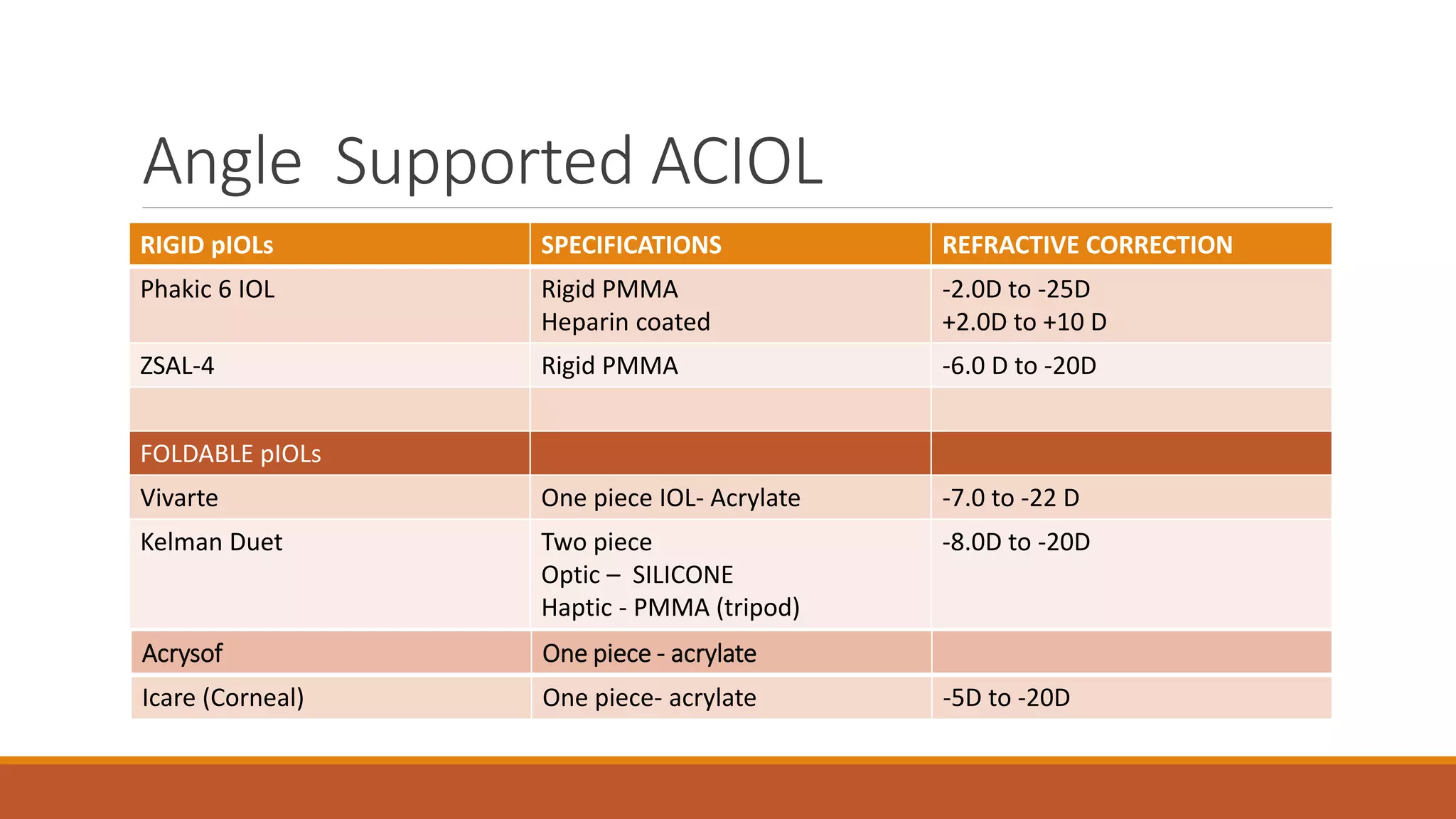
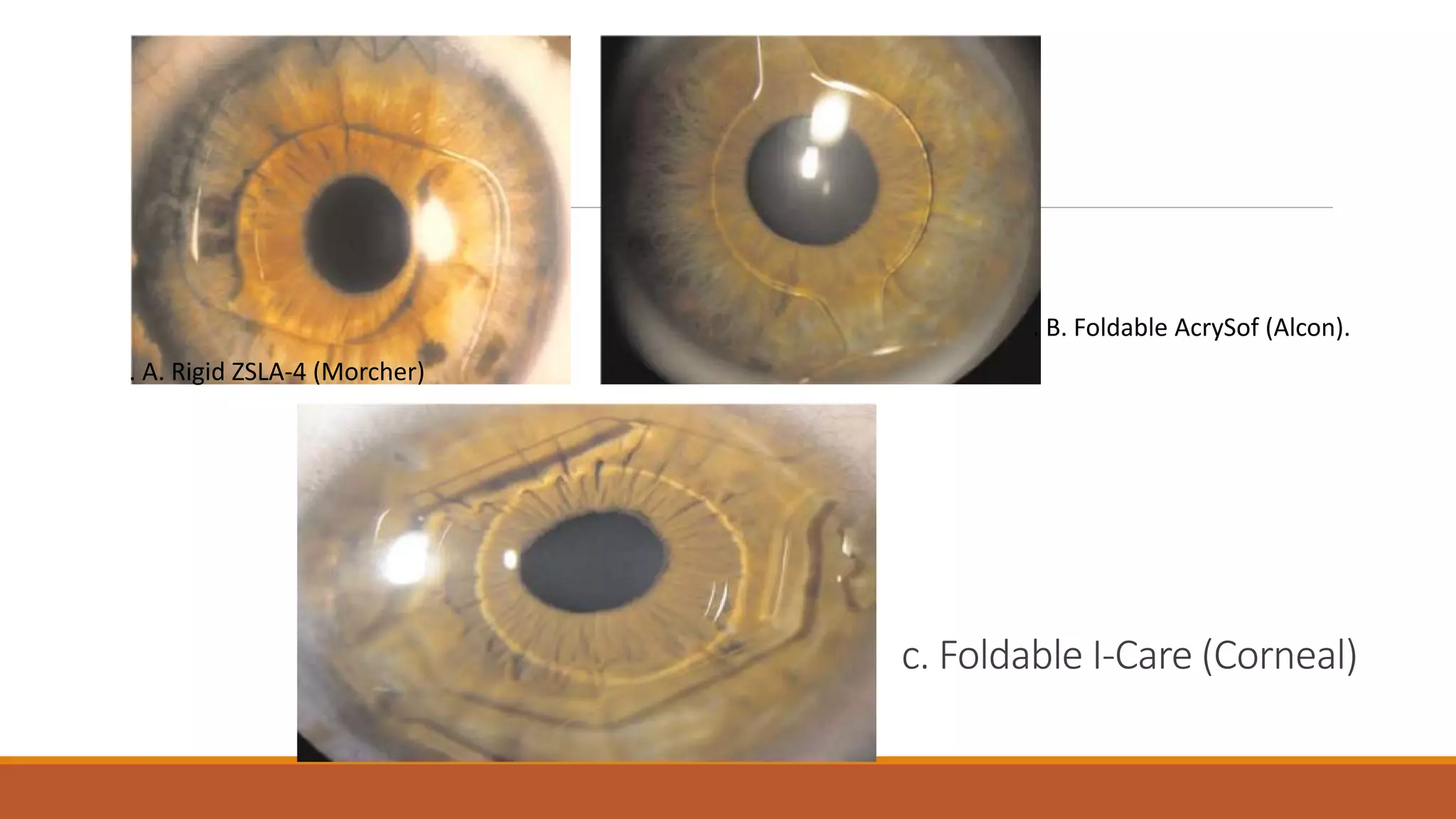
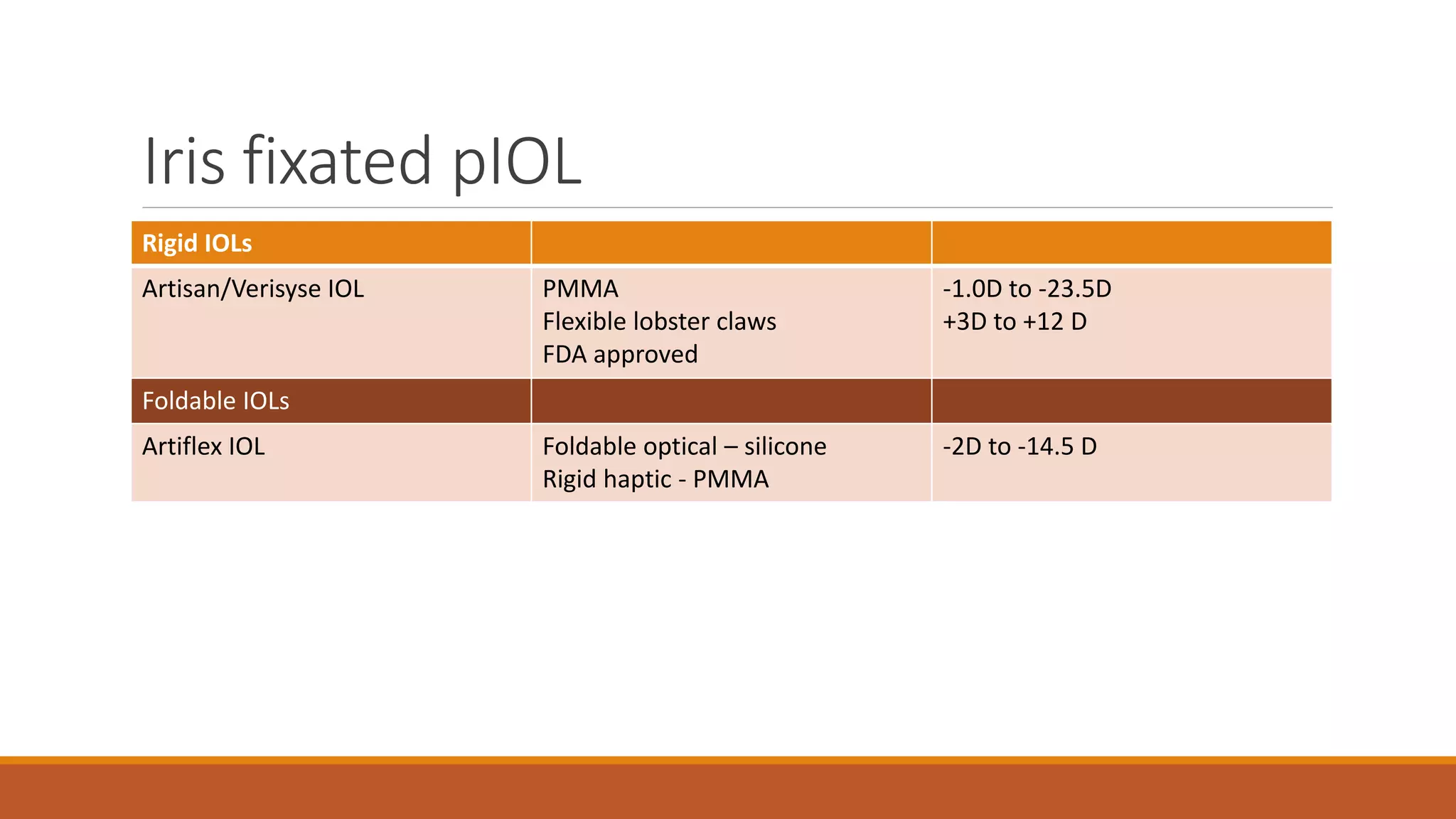
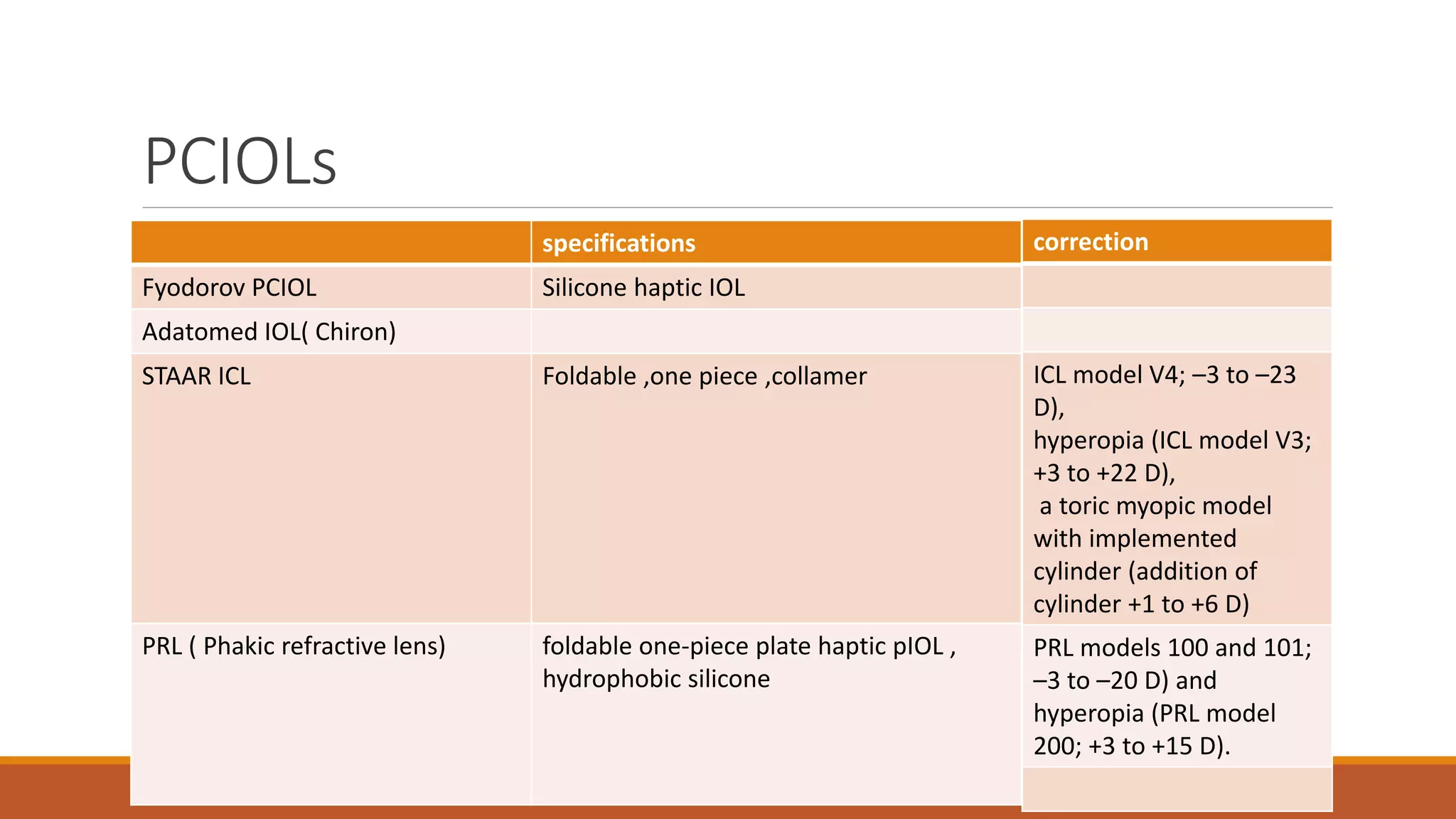
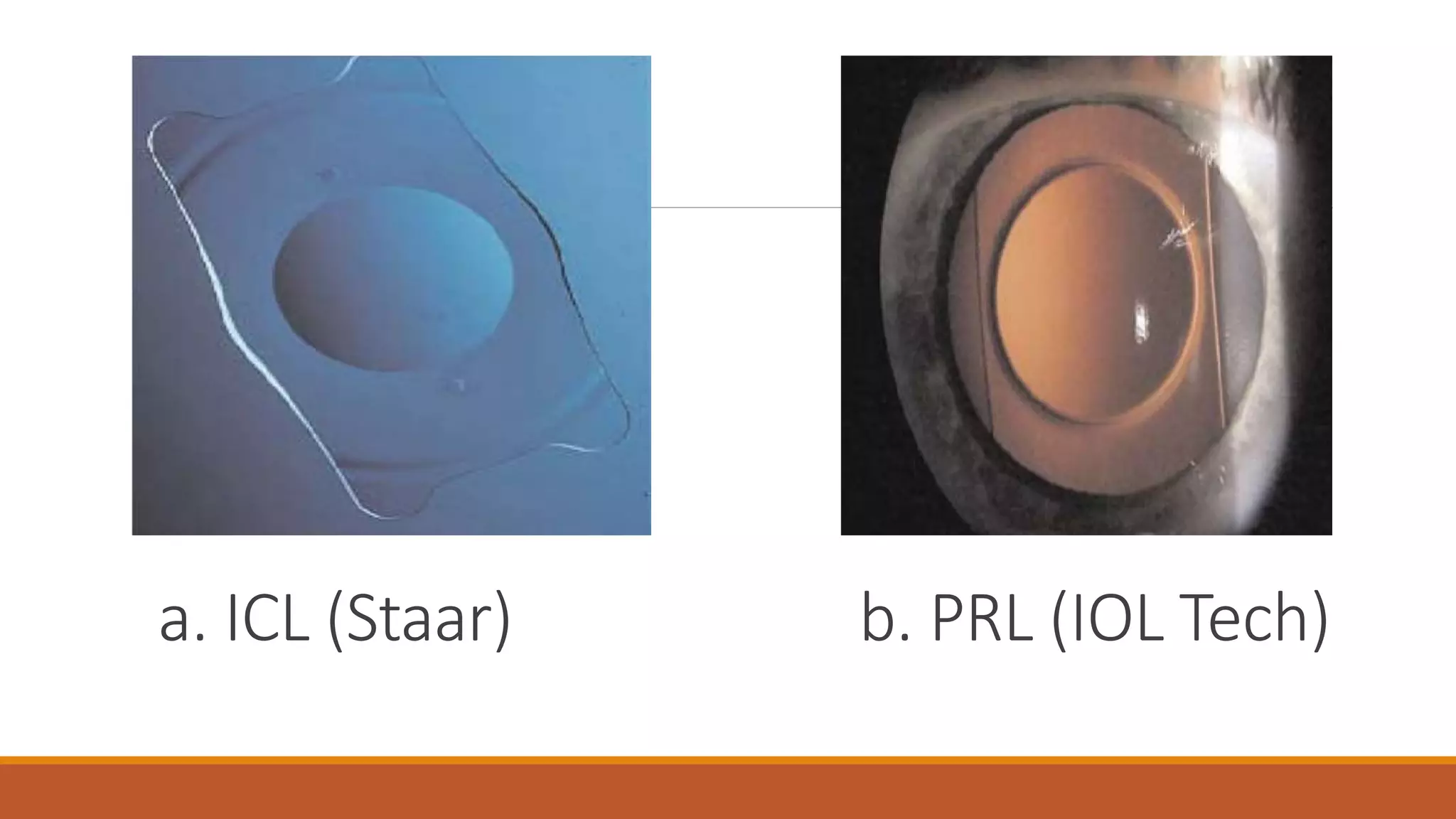
1) Phakic IOLs are artificial lenses implanted in the eye to correct refractive errors while leaving the natural lens intact. They are classified as angle-supported, iris-fixated, or posterior chamber IOLs.
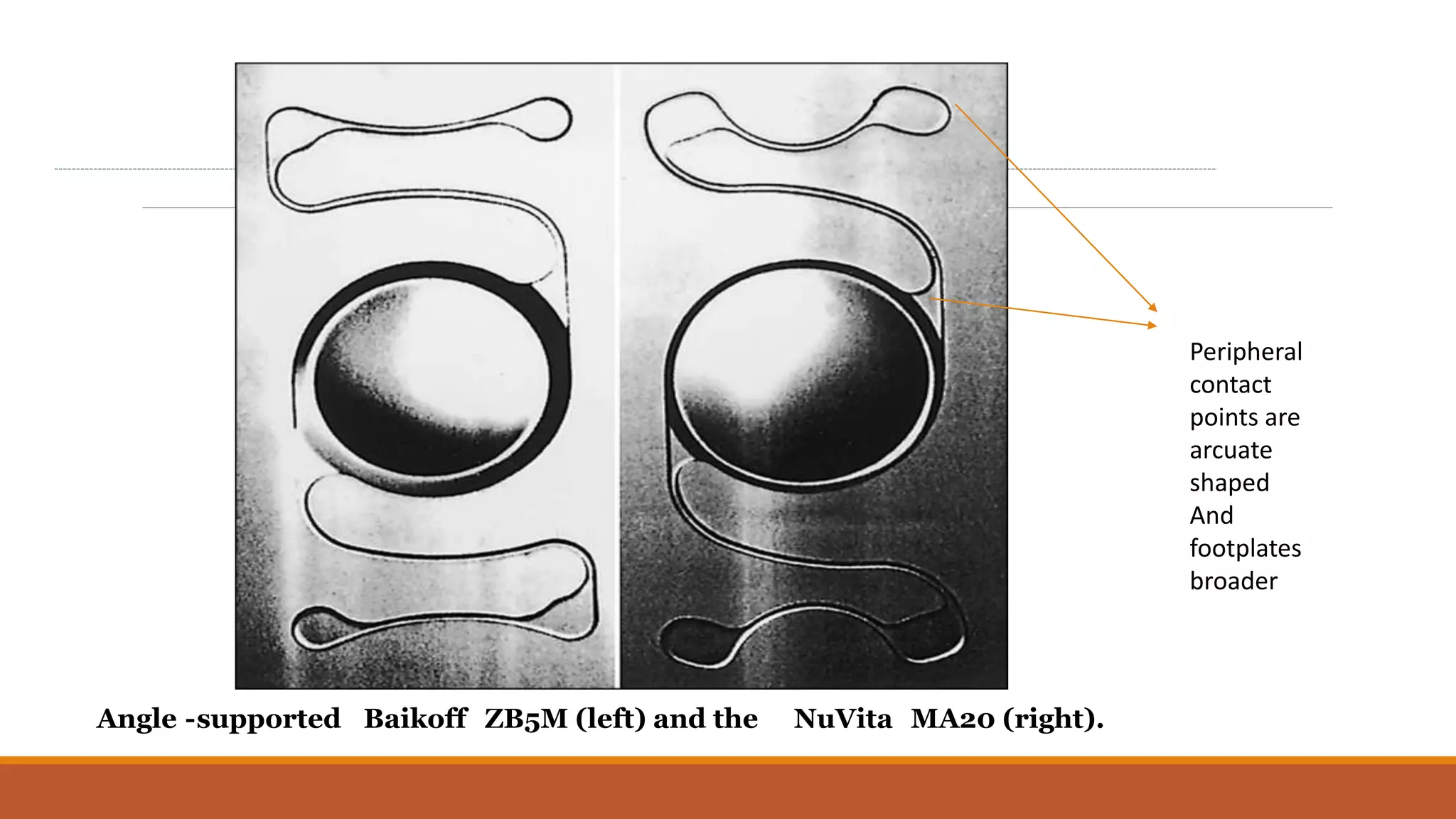
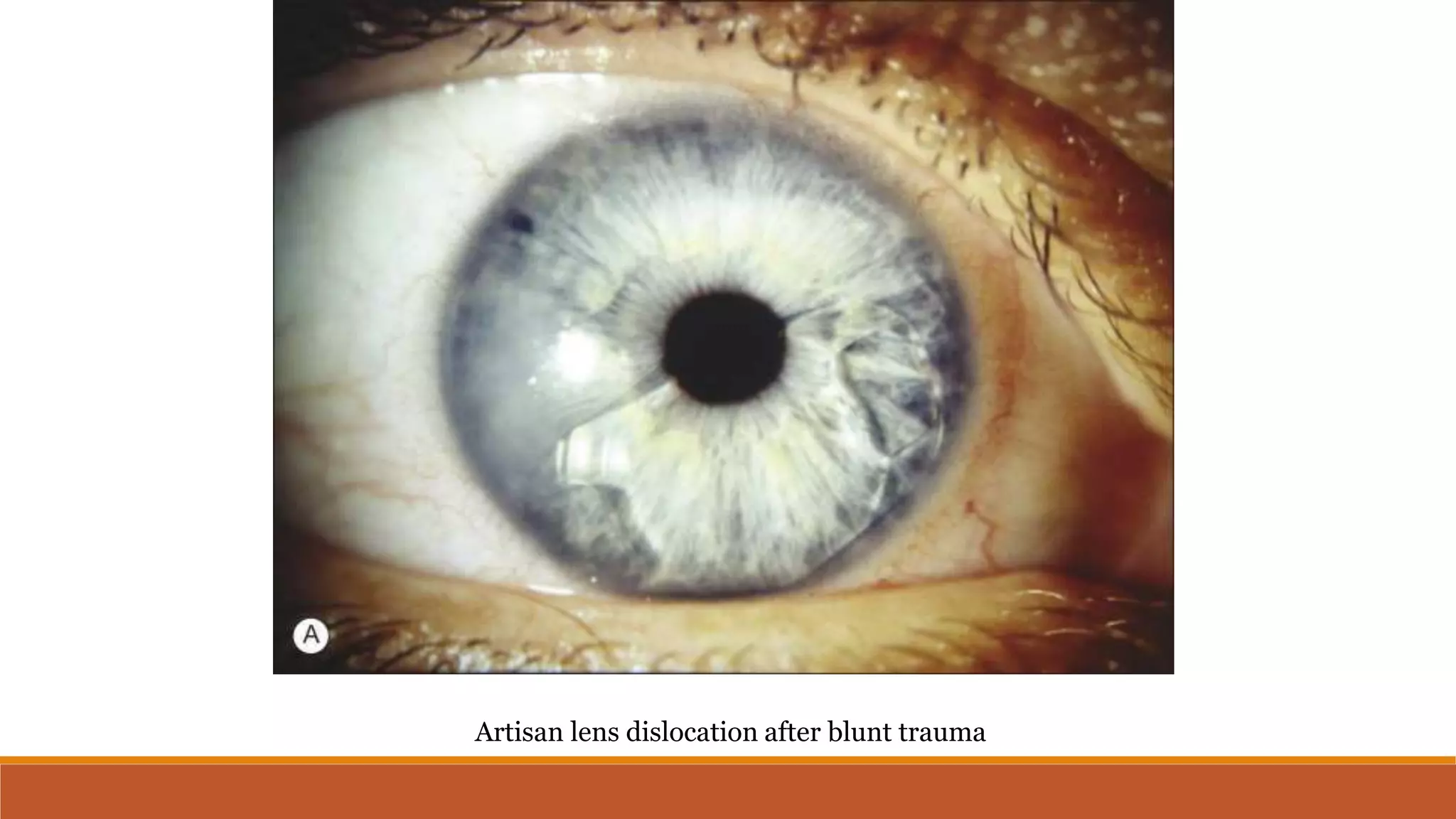
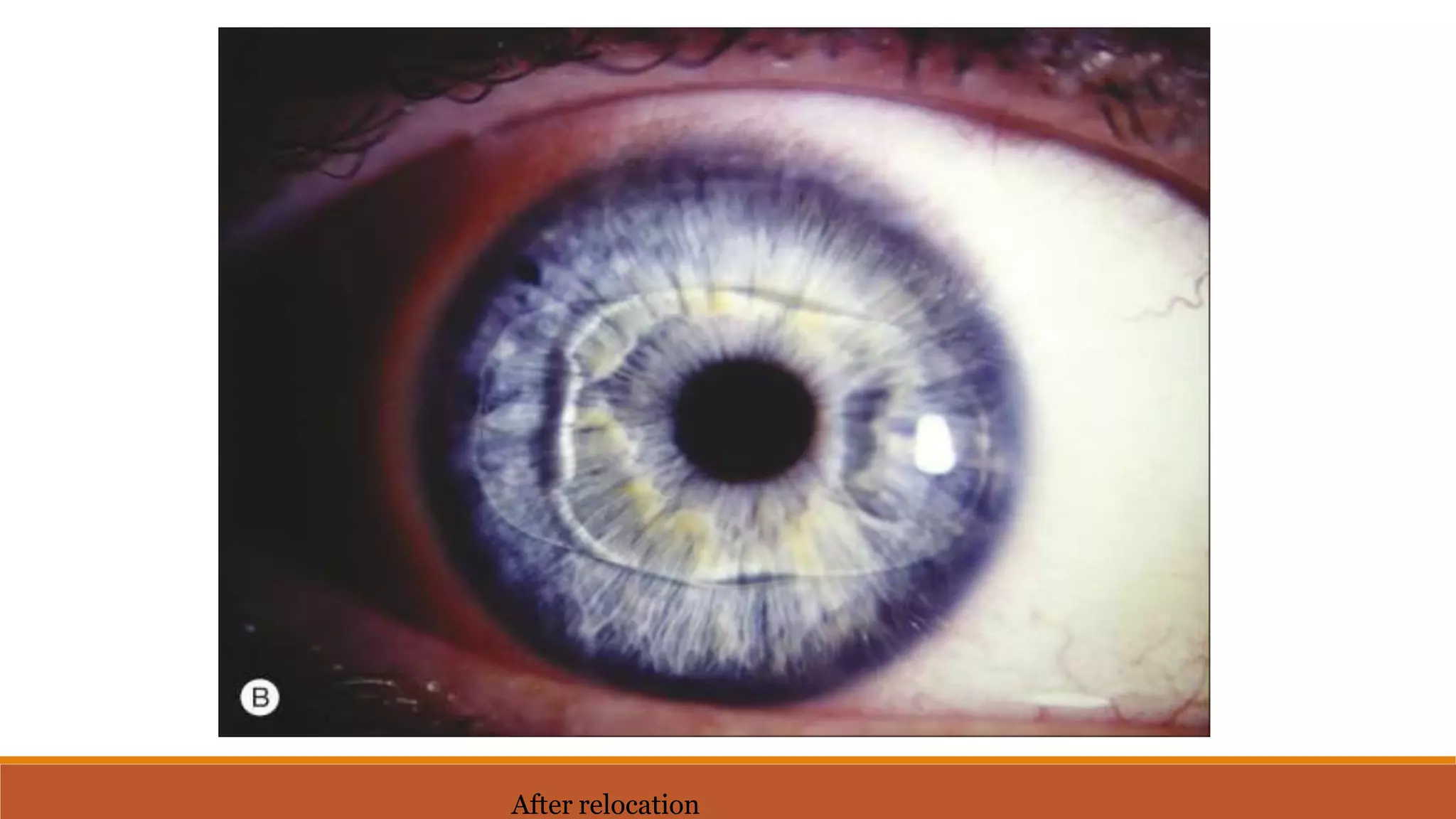
2) The first phakic IOLs date back to the 1950s but modern designs from the 1980s/90s include the Artisan iris-claw lens and posterior chamber lenses like the ICL.
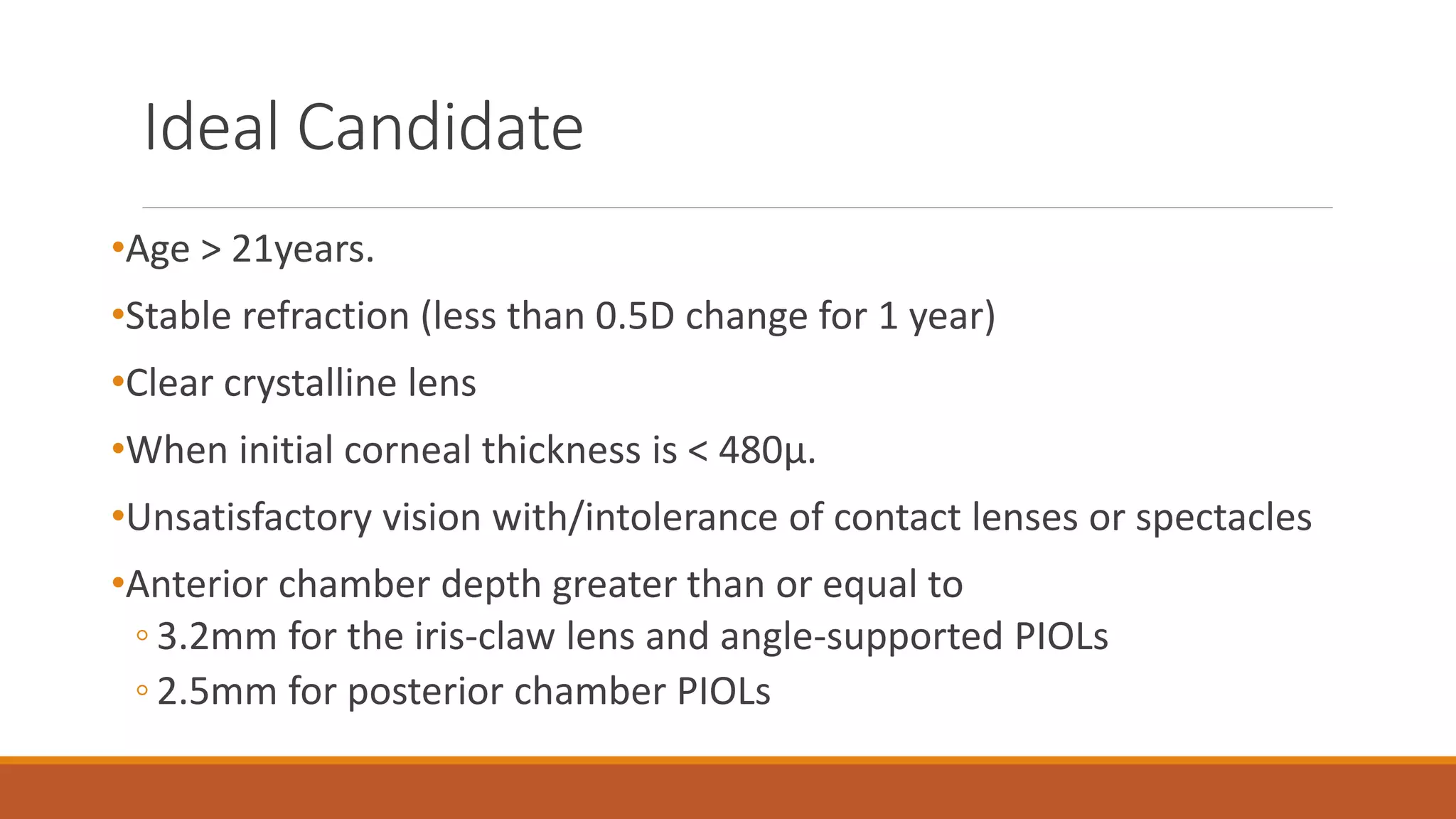
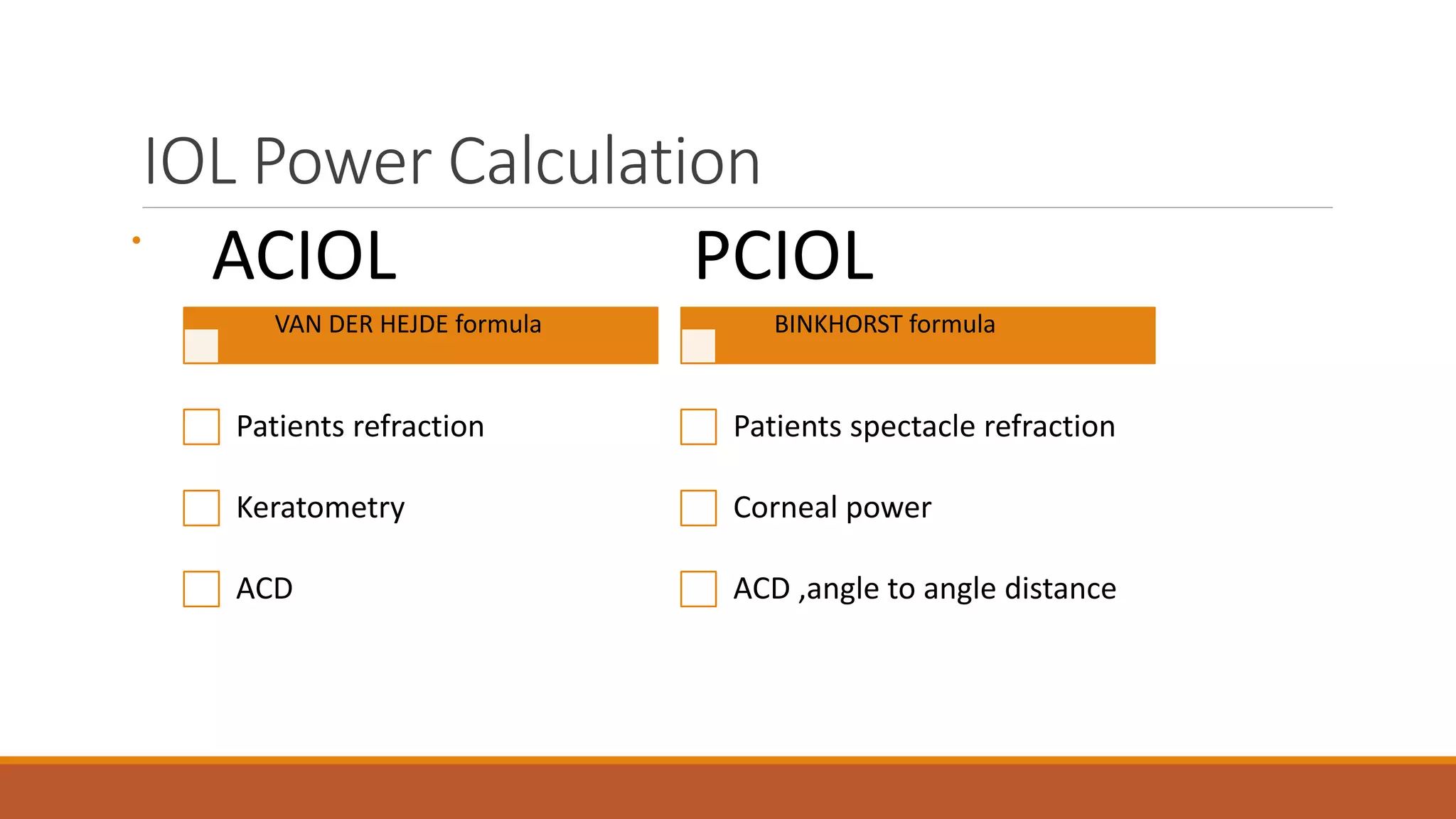
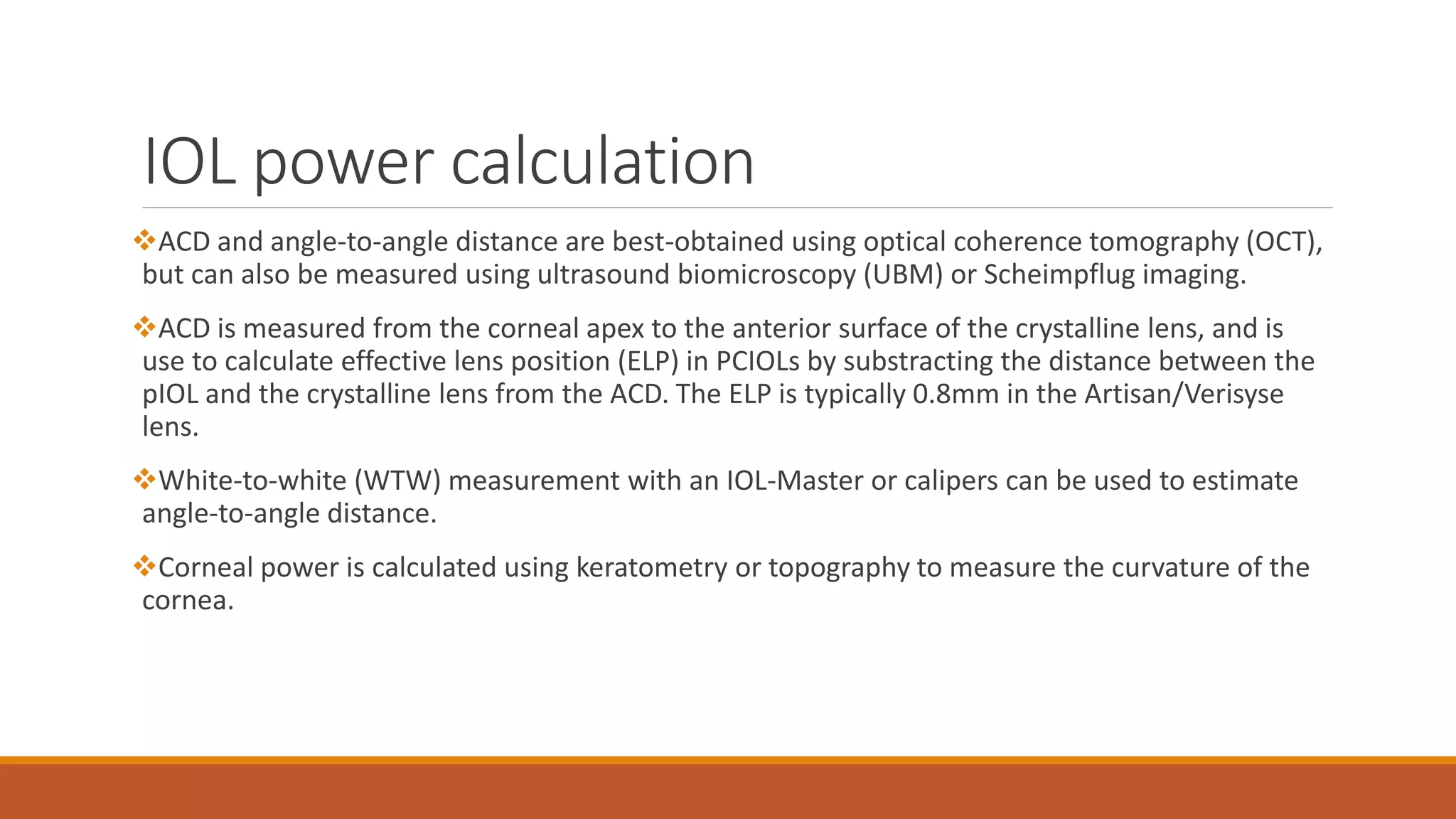
3) Ideal phakic IOL candidates have a stable refraction and meet endothelial cell and anterior chamber depth requirements. Assessments include VA, biometry, and endothelial cell counts.