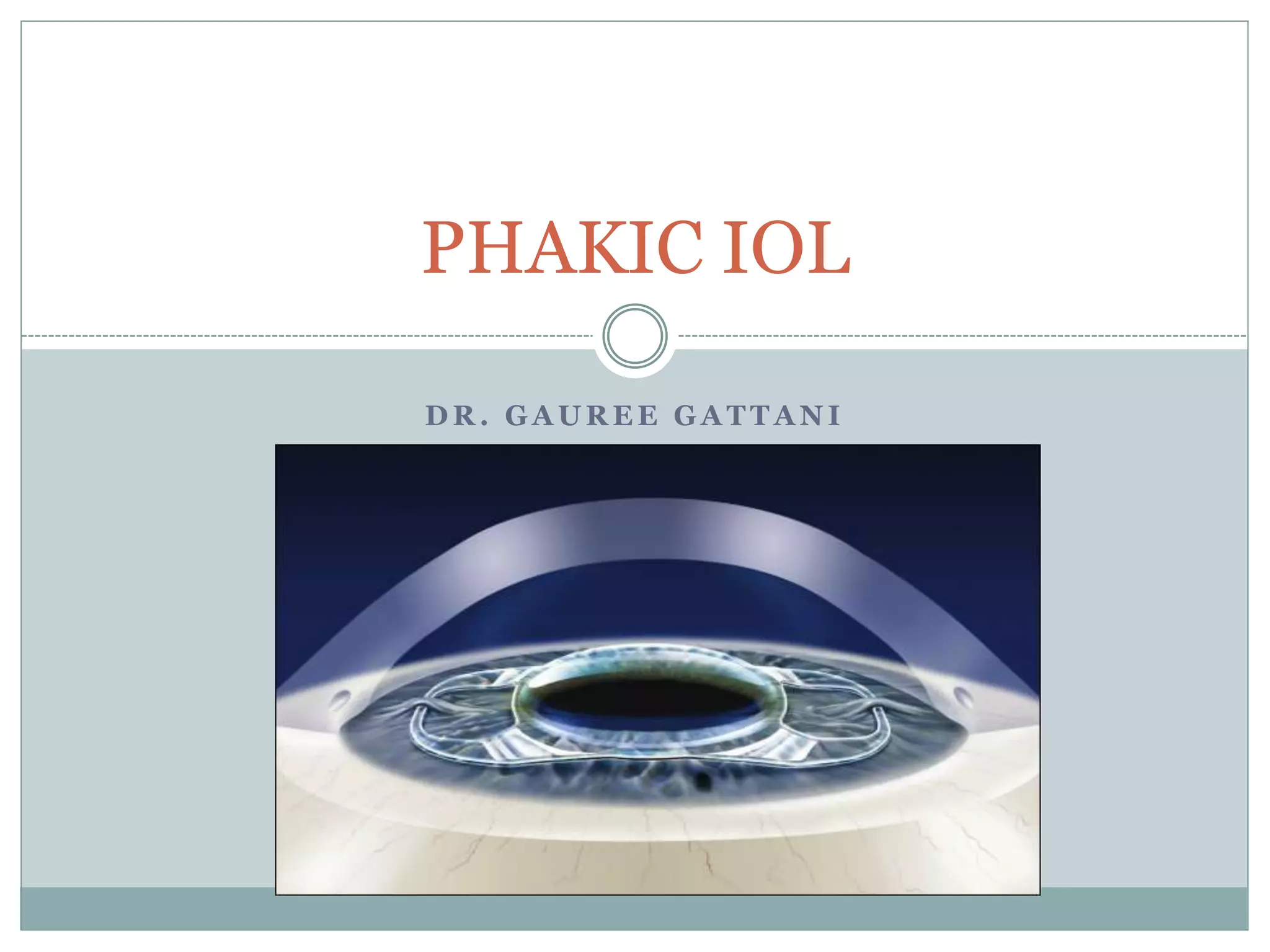
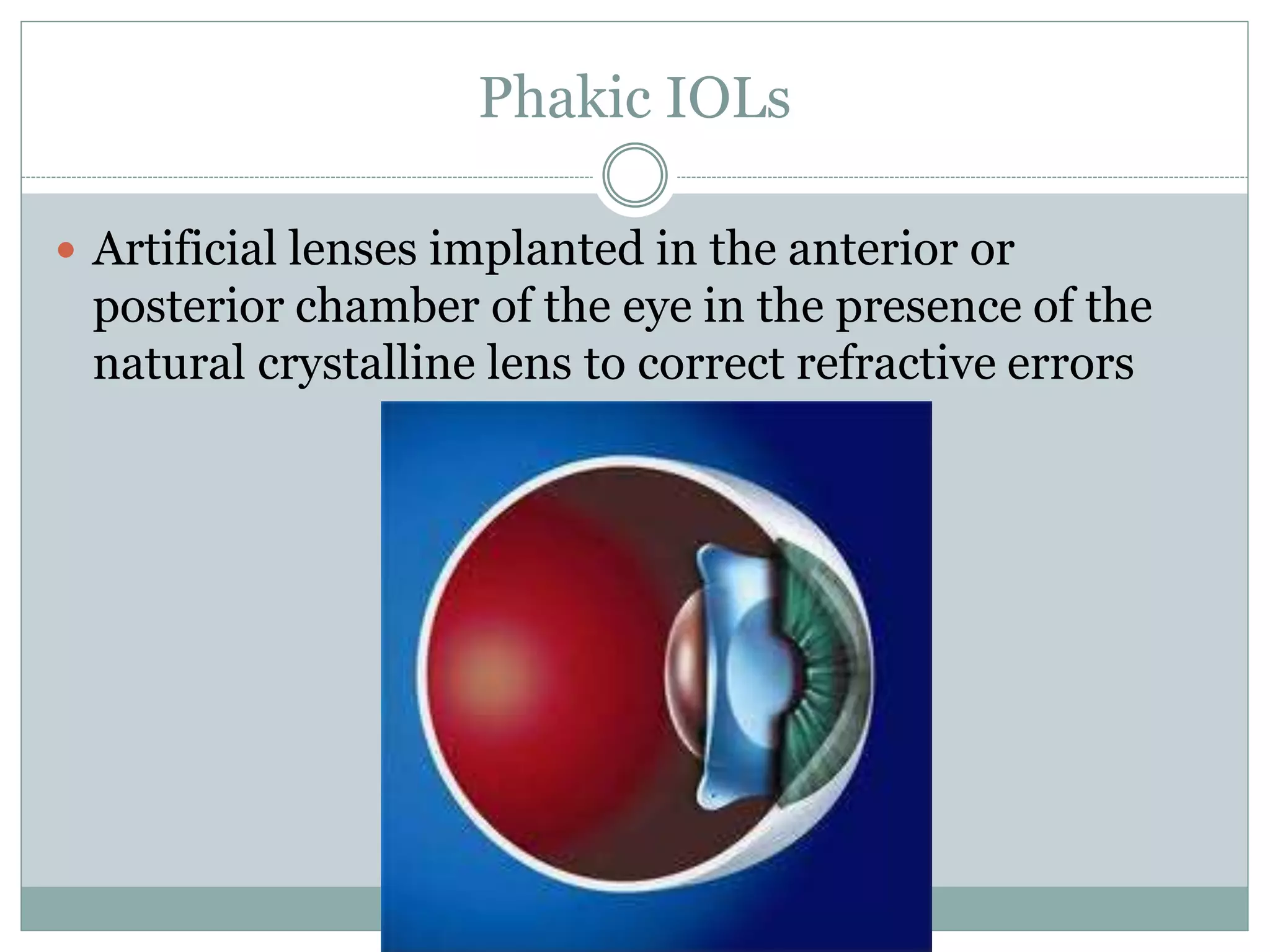
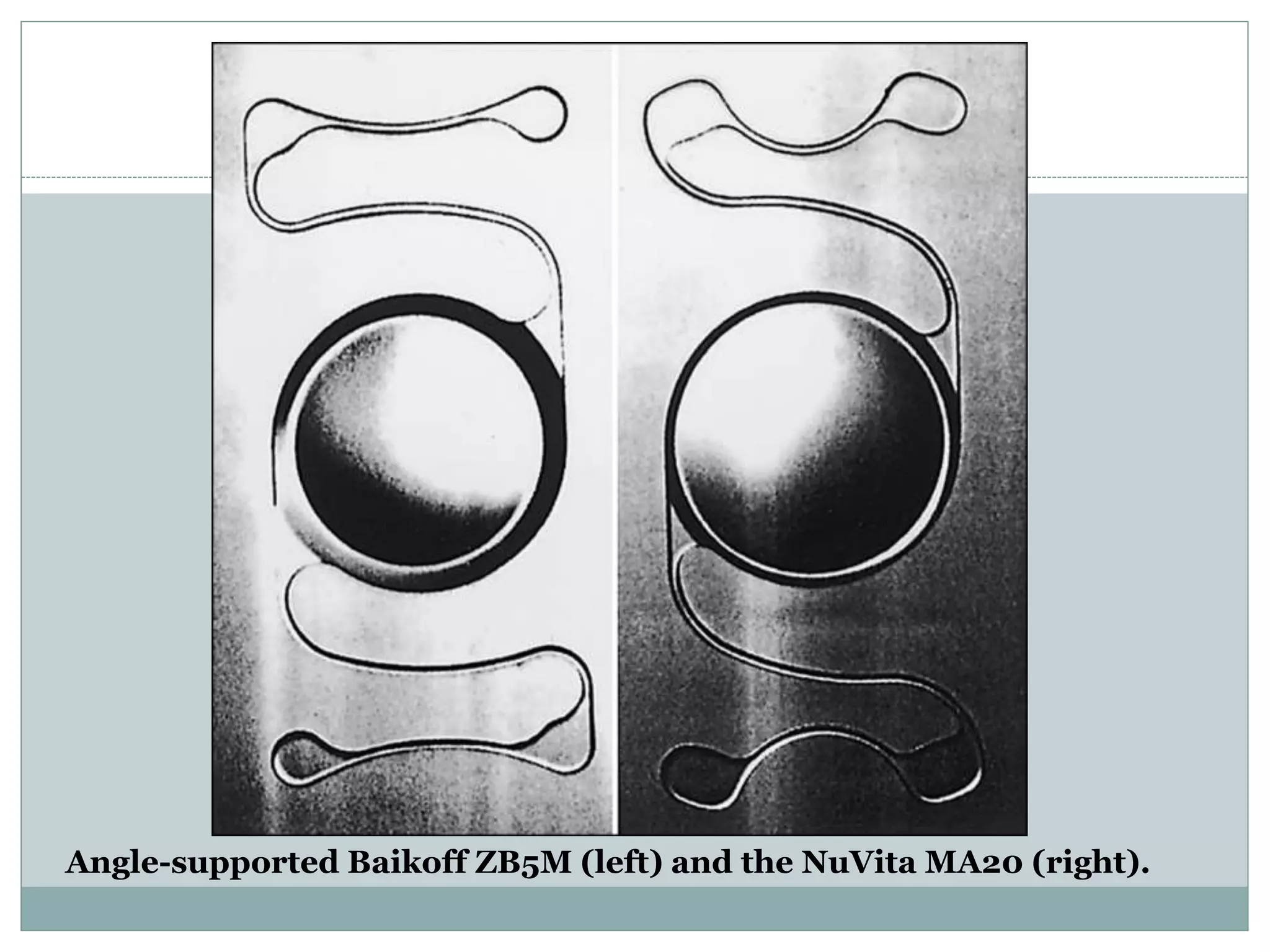
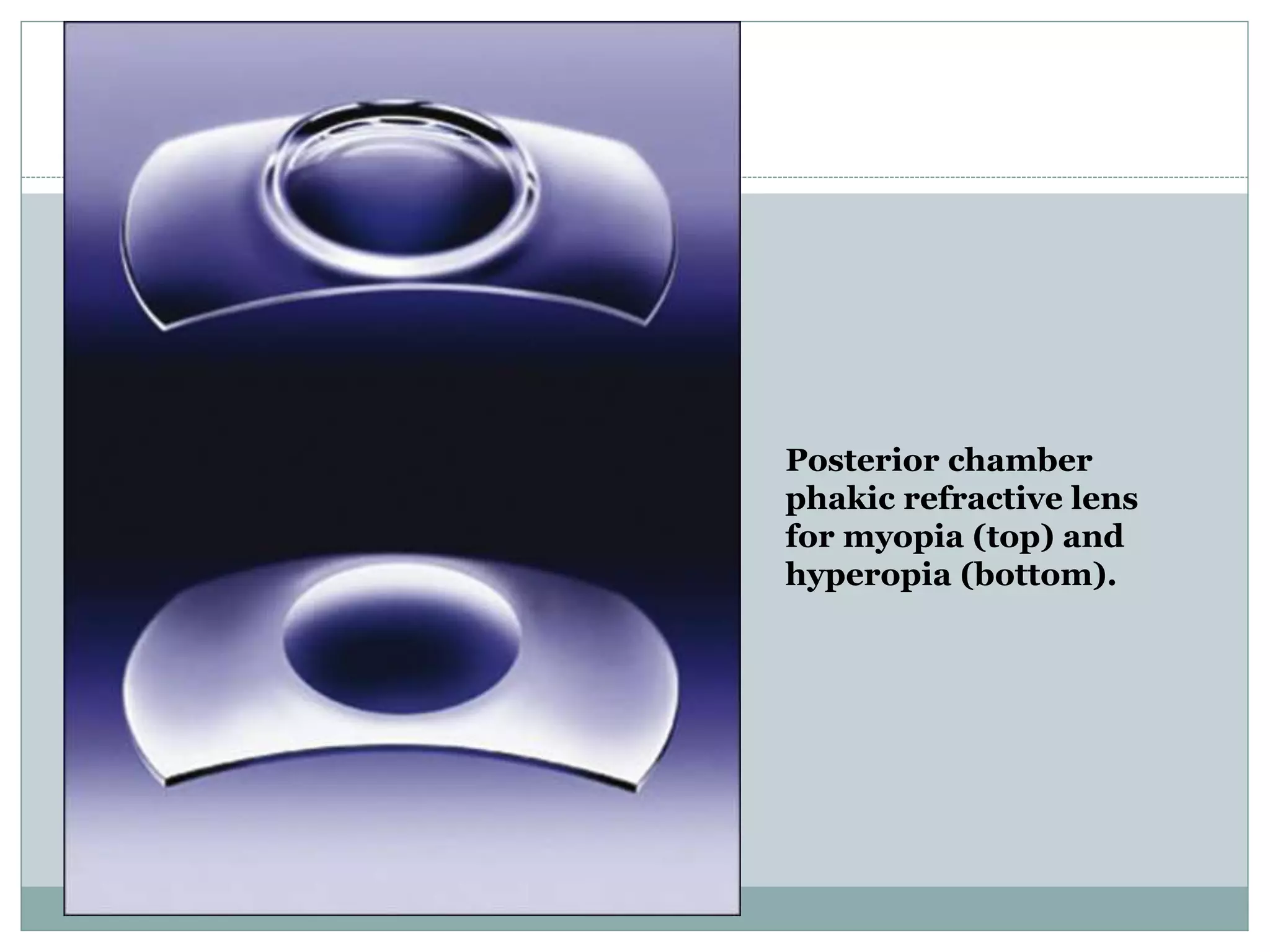
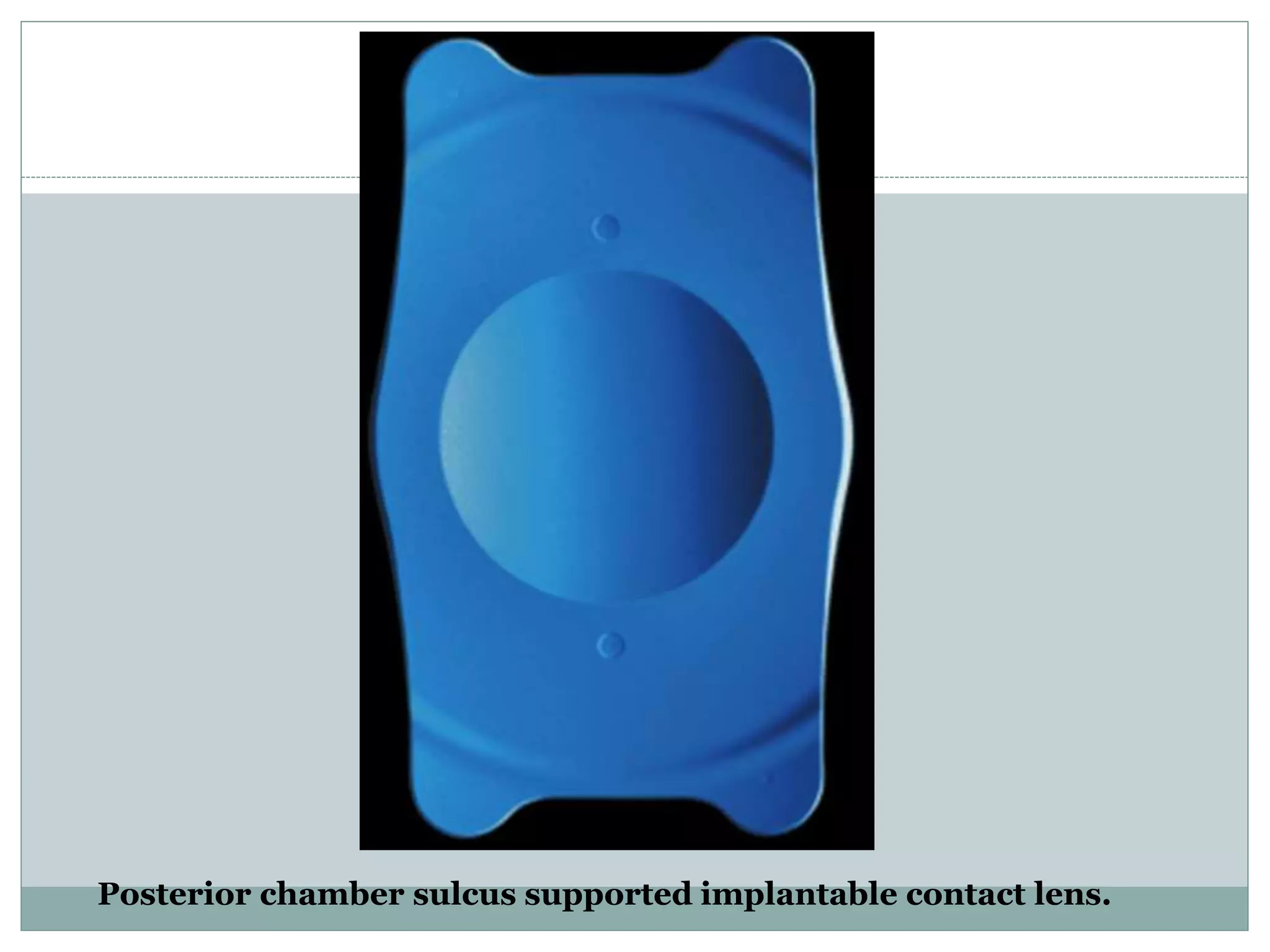
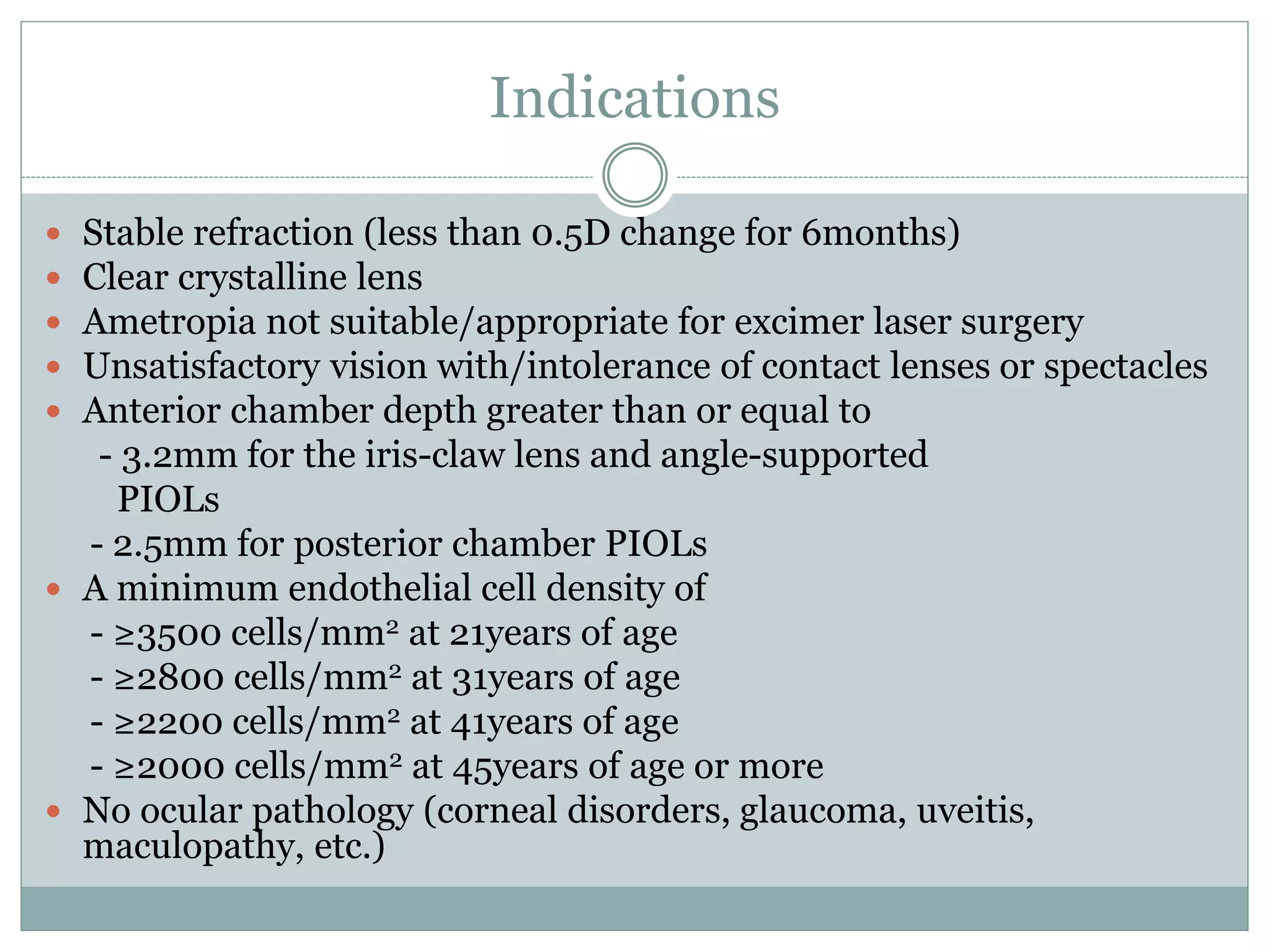
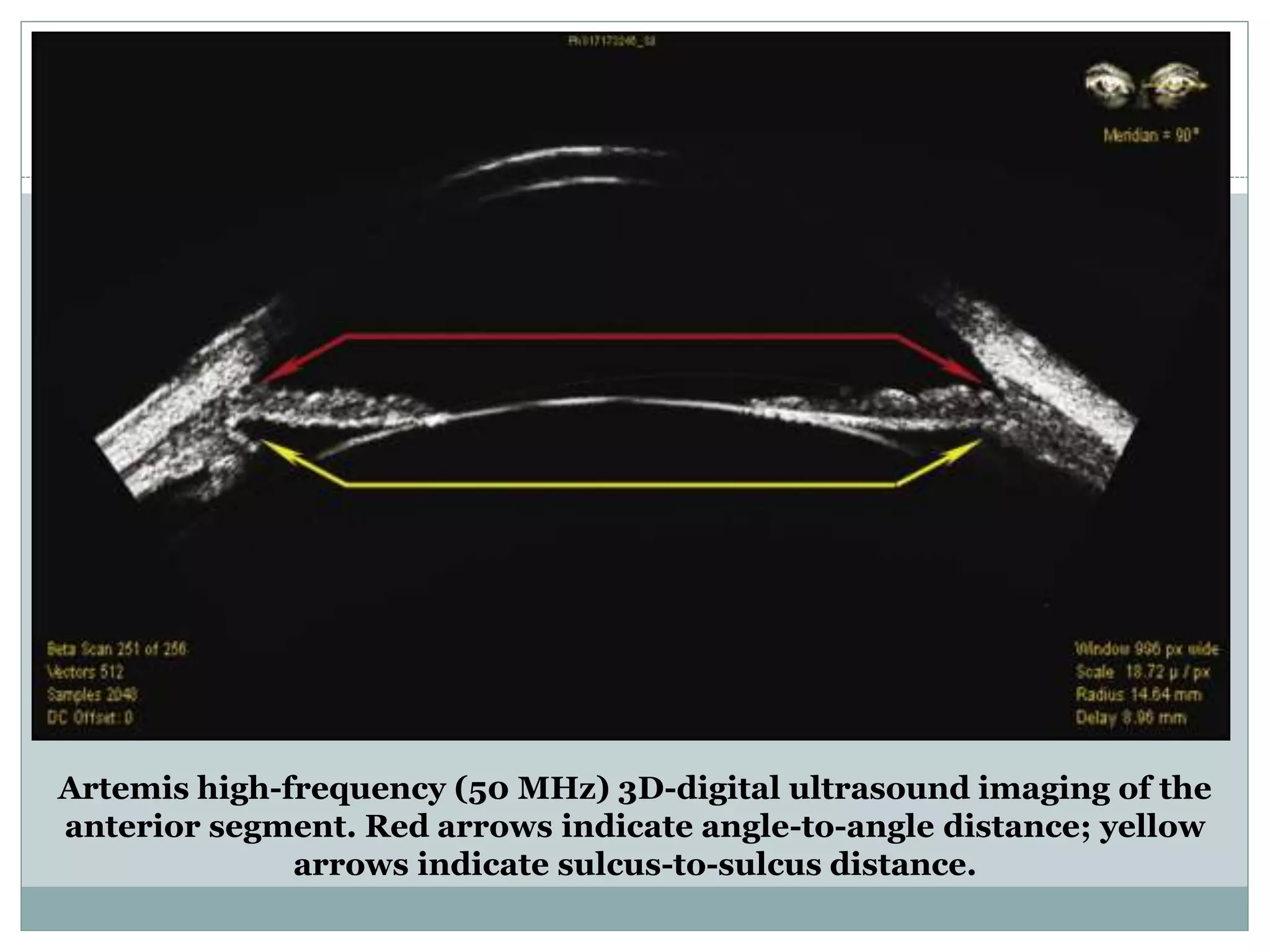
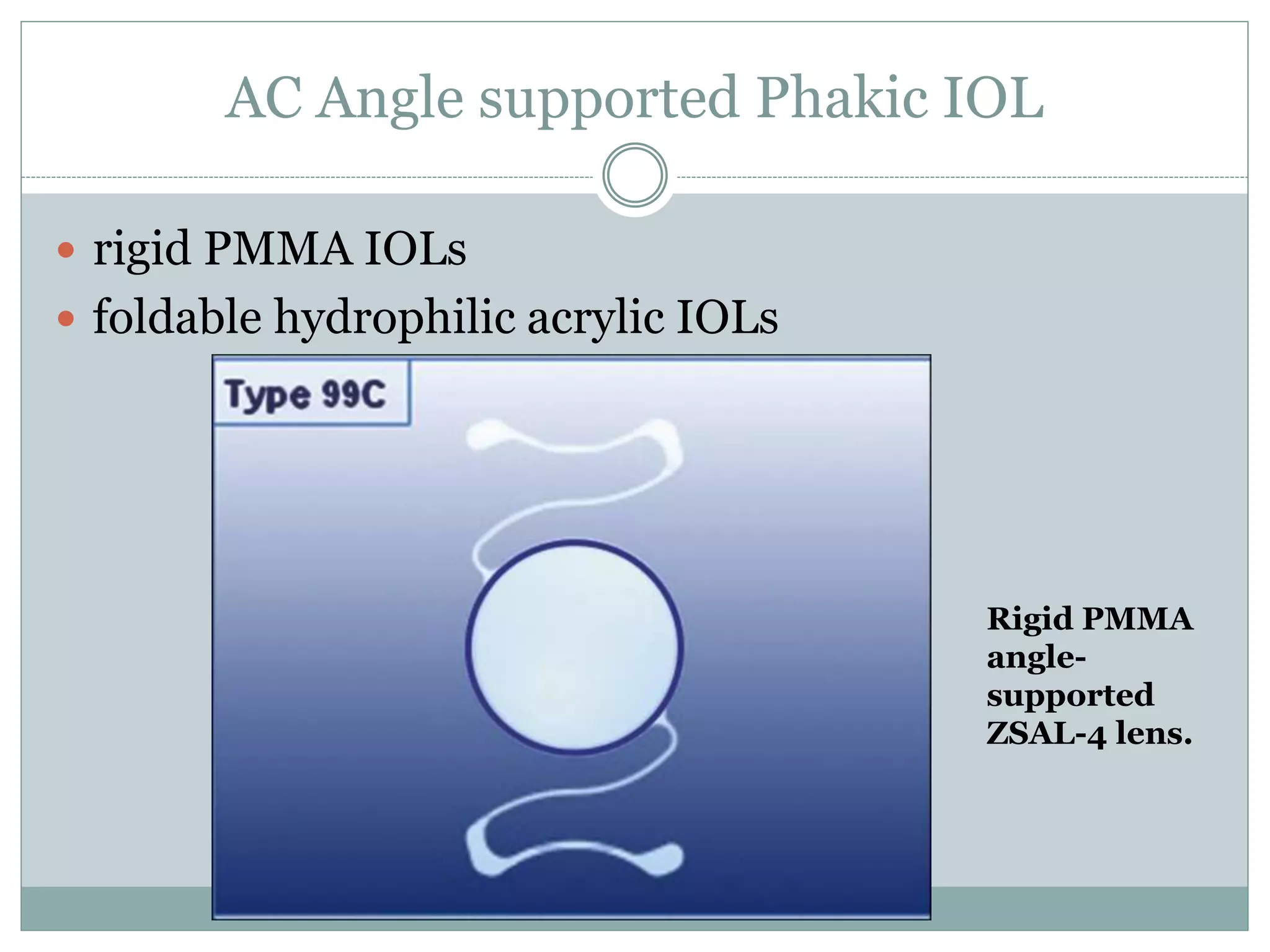
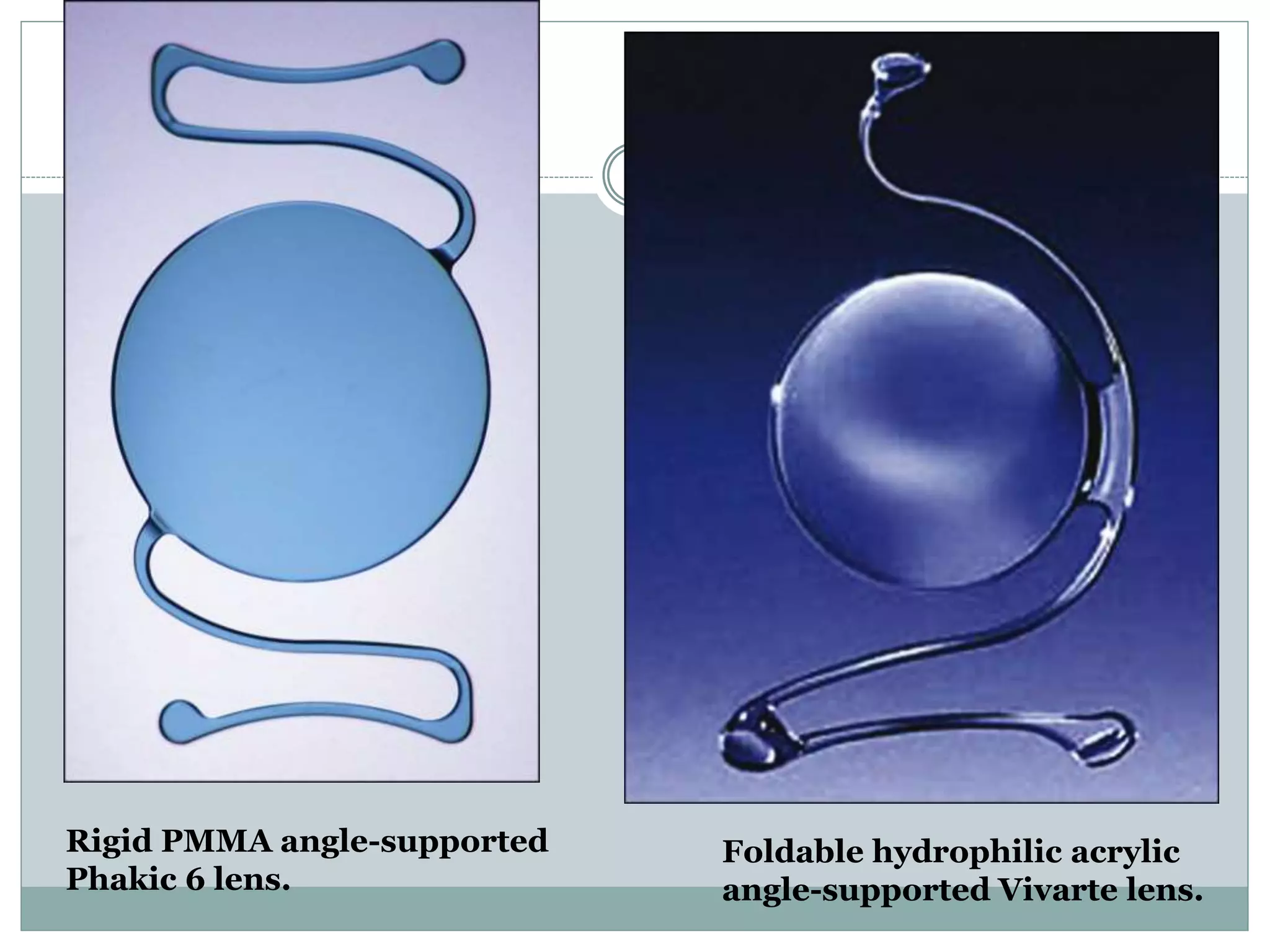
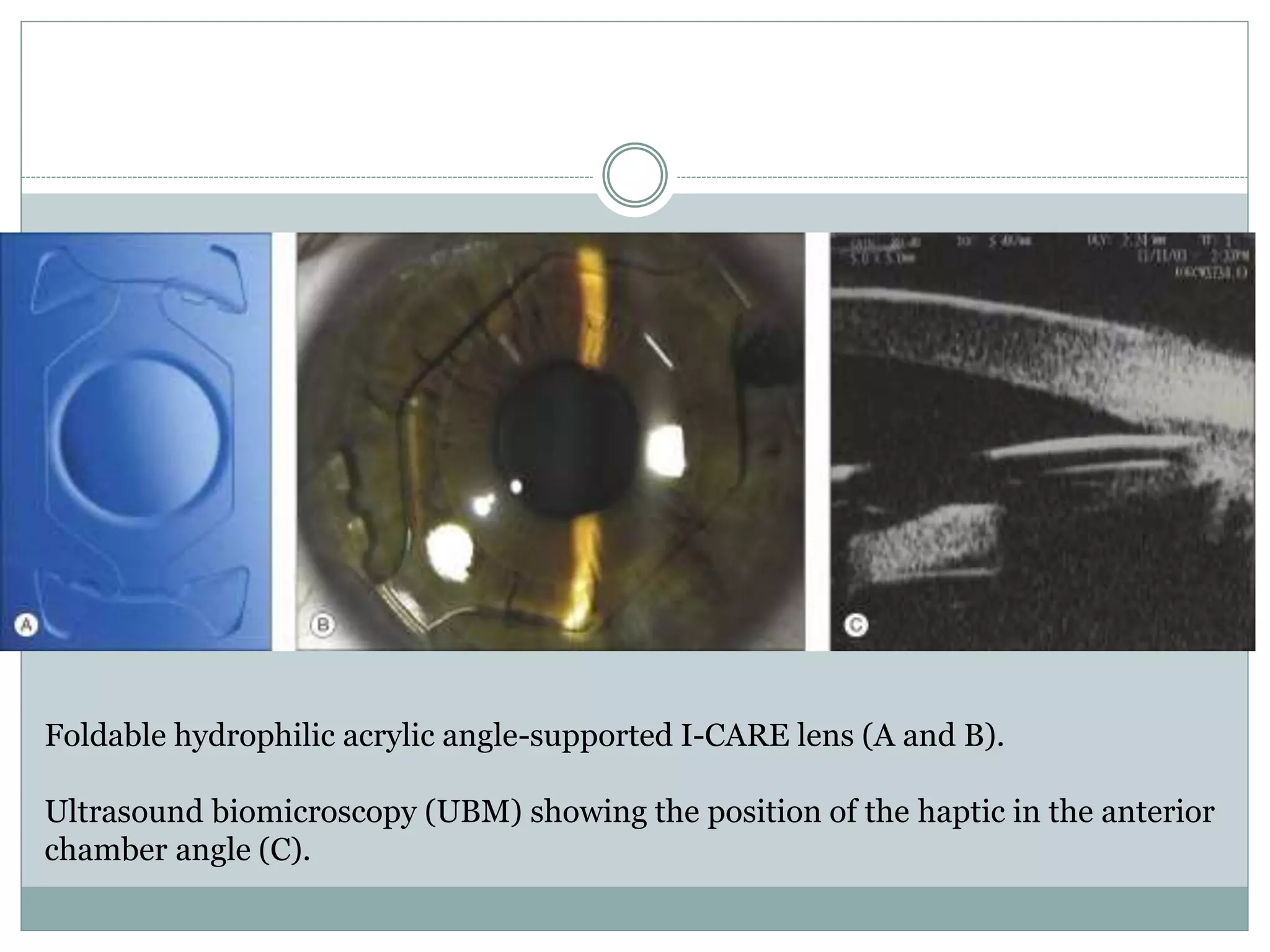
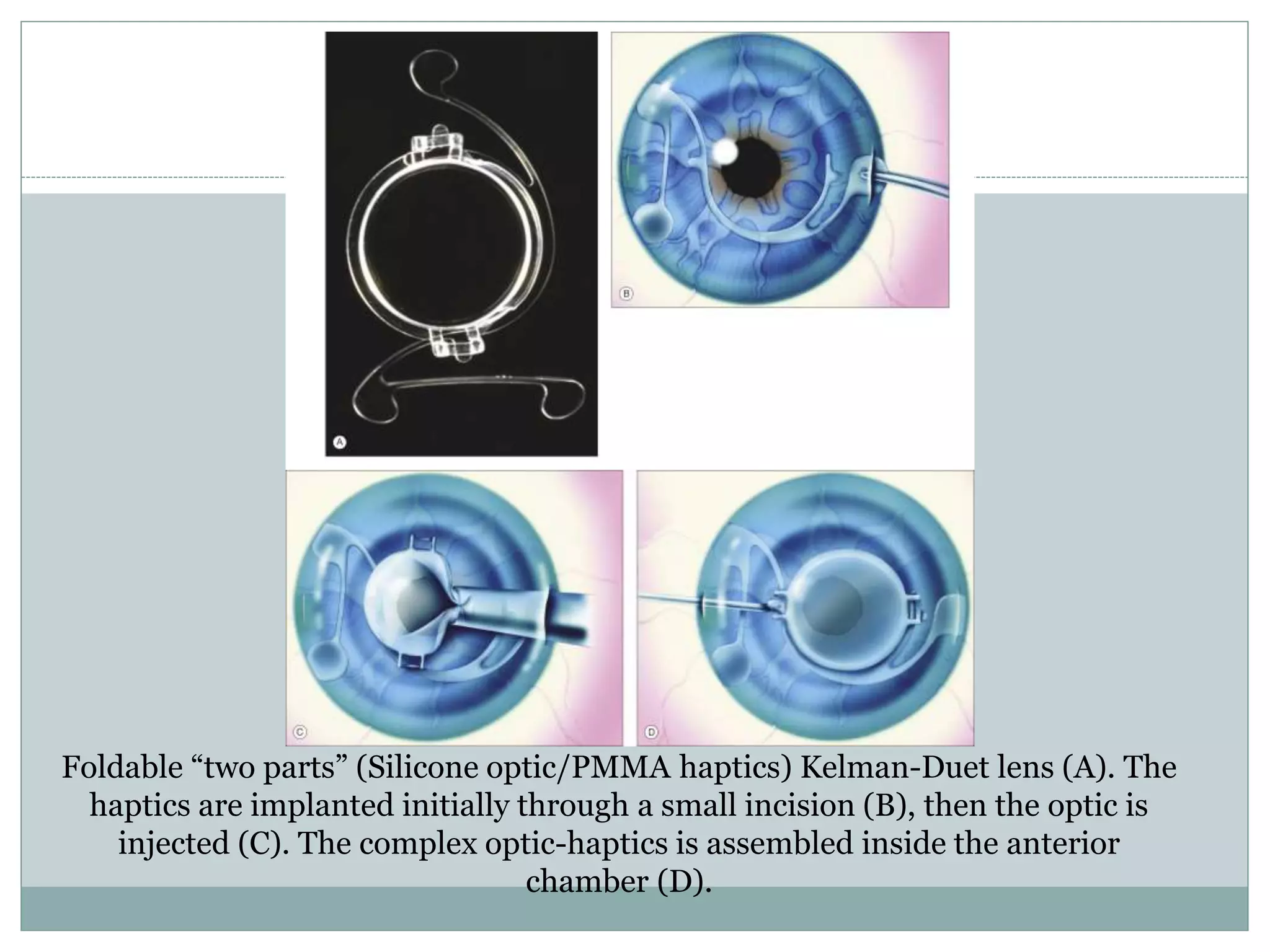
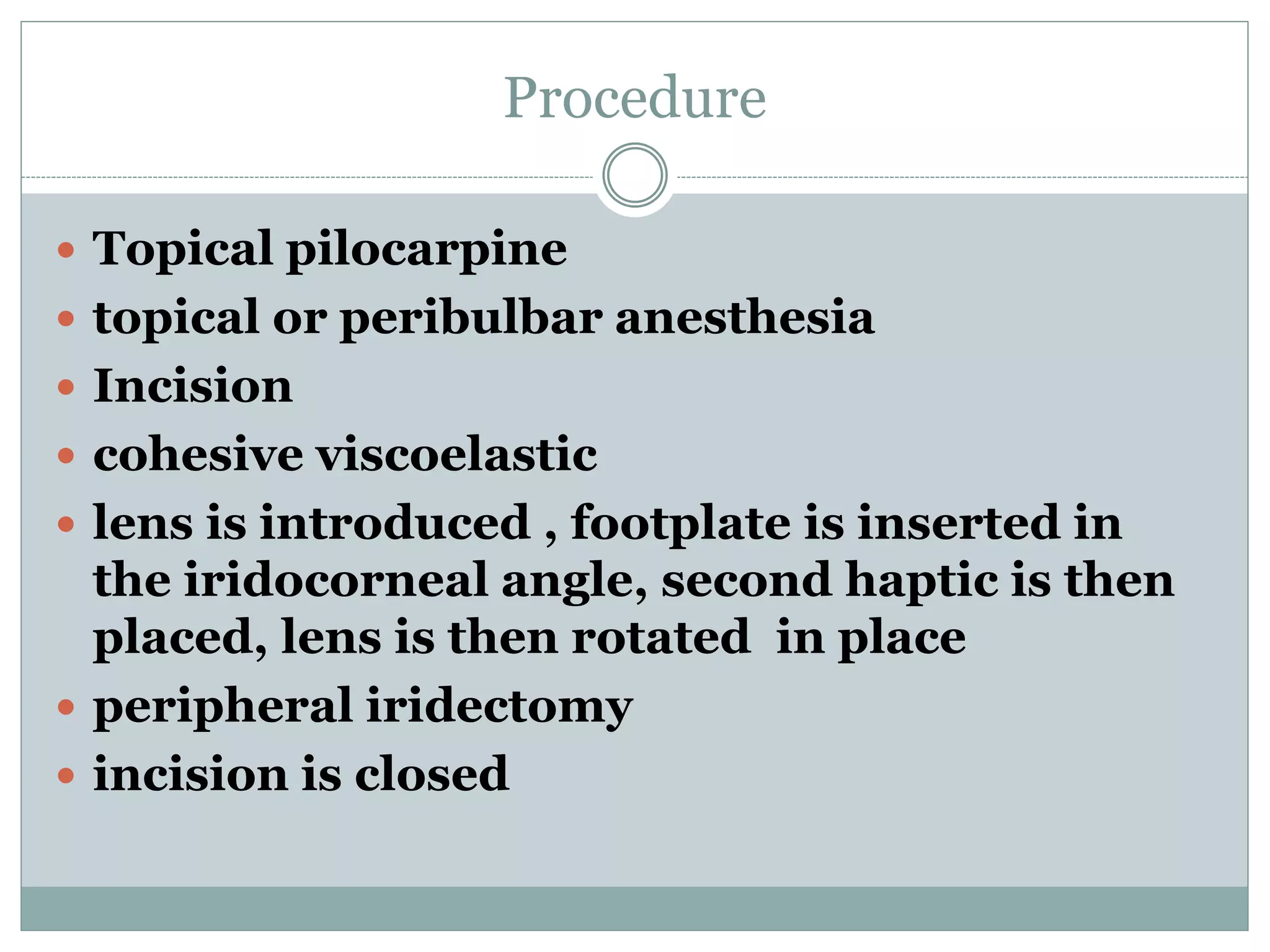
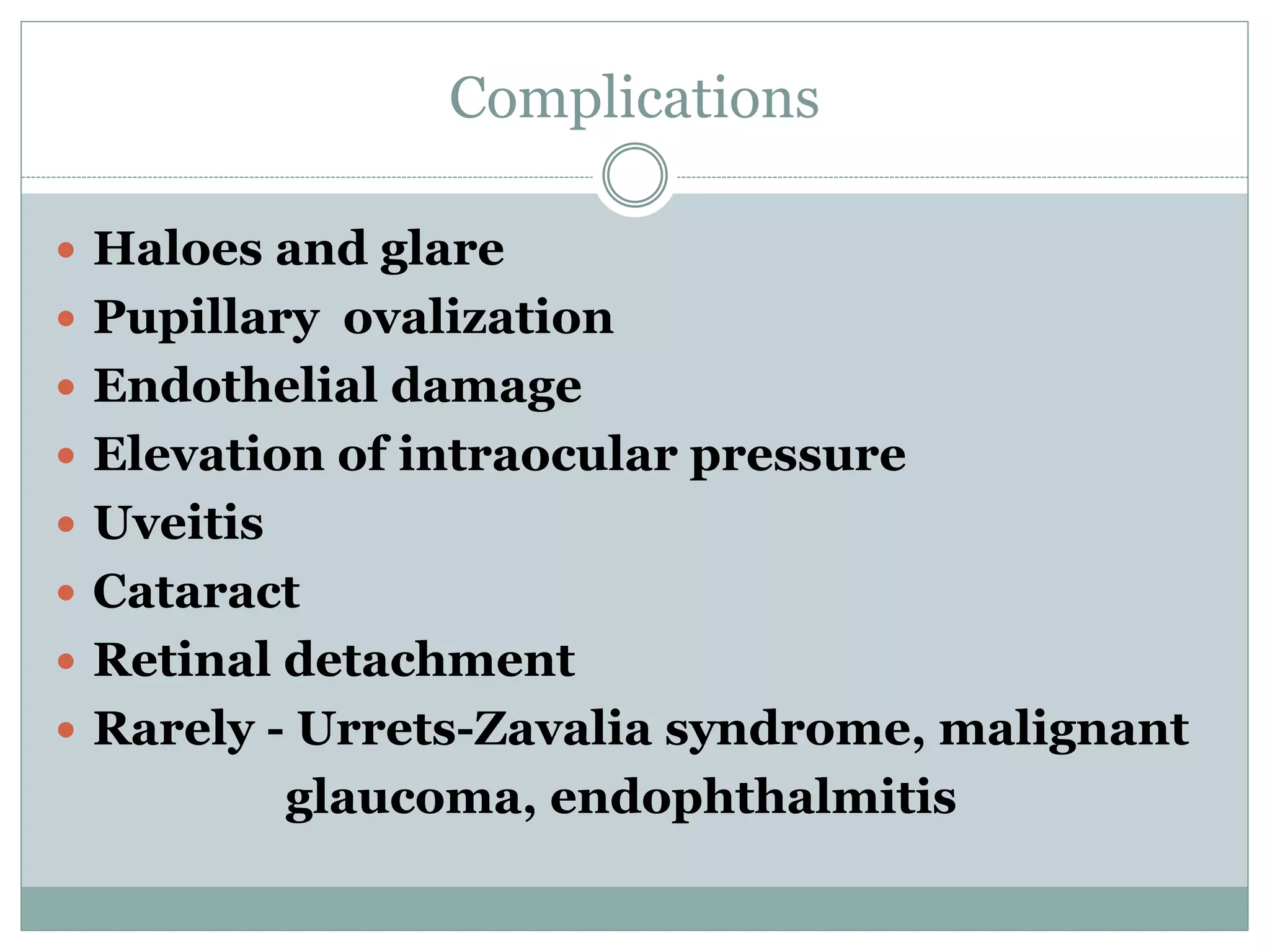
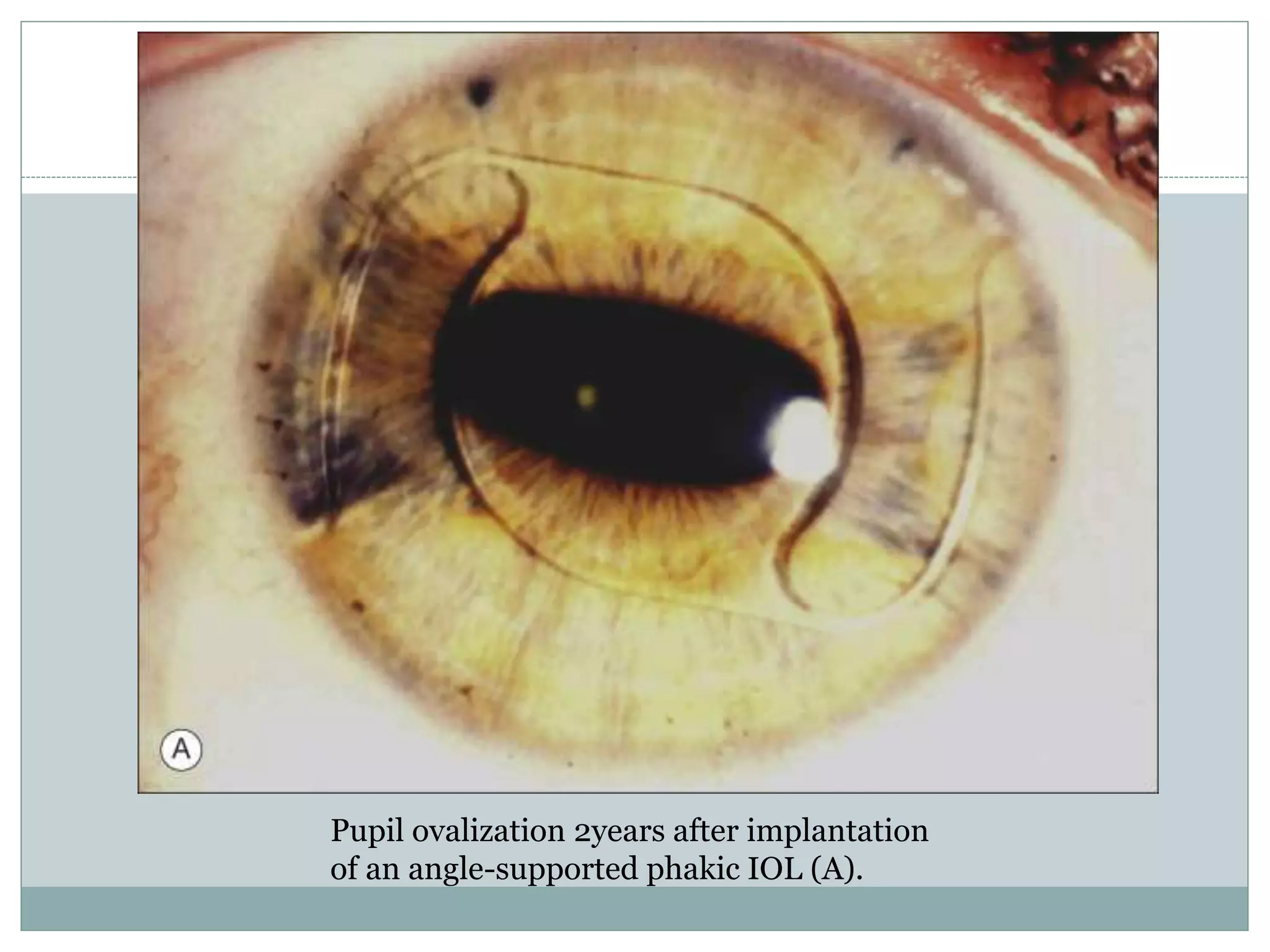
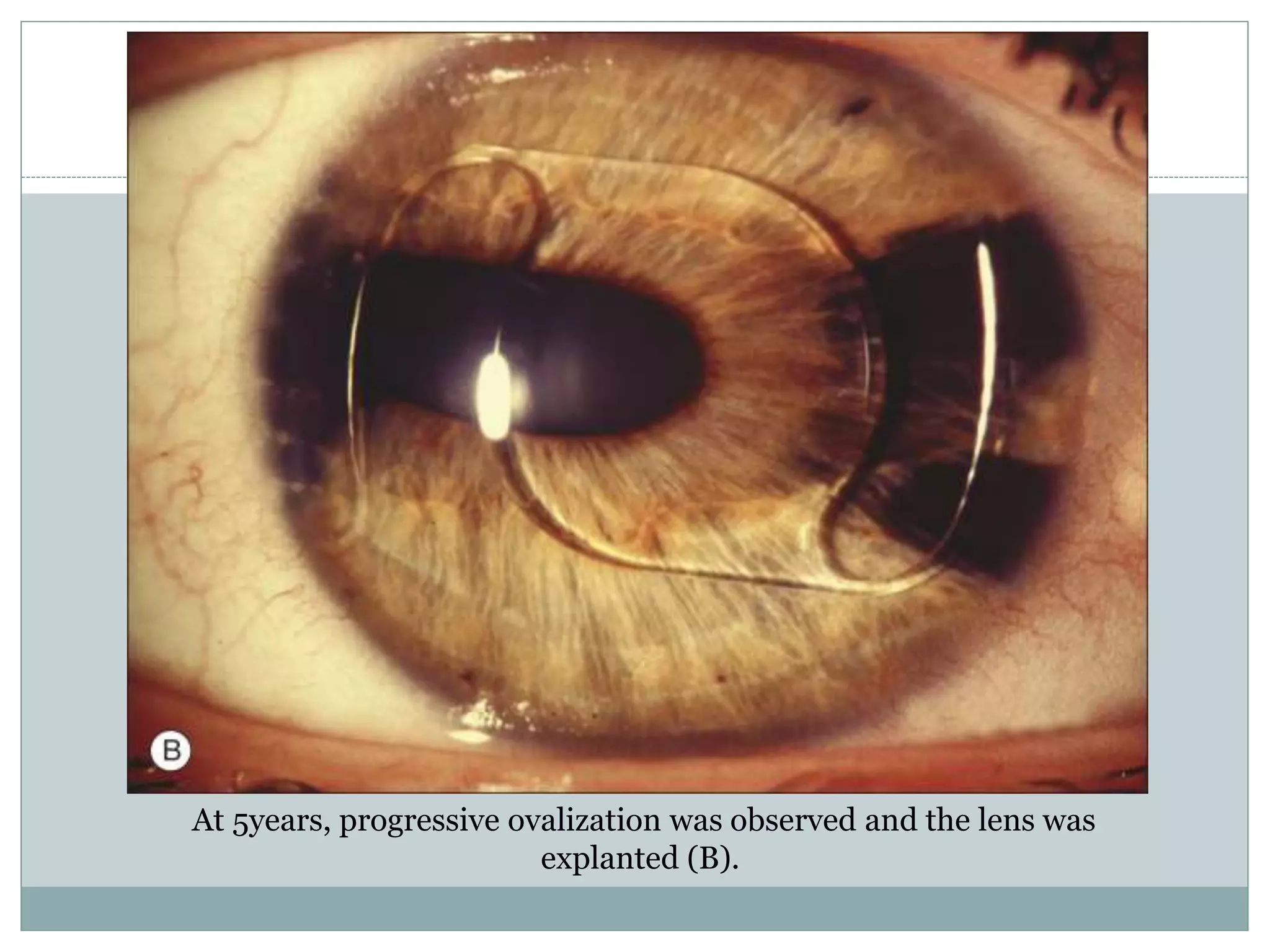
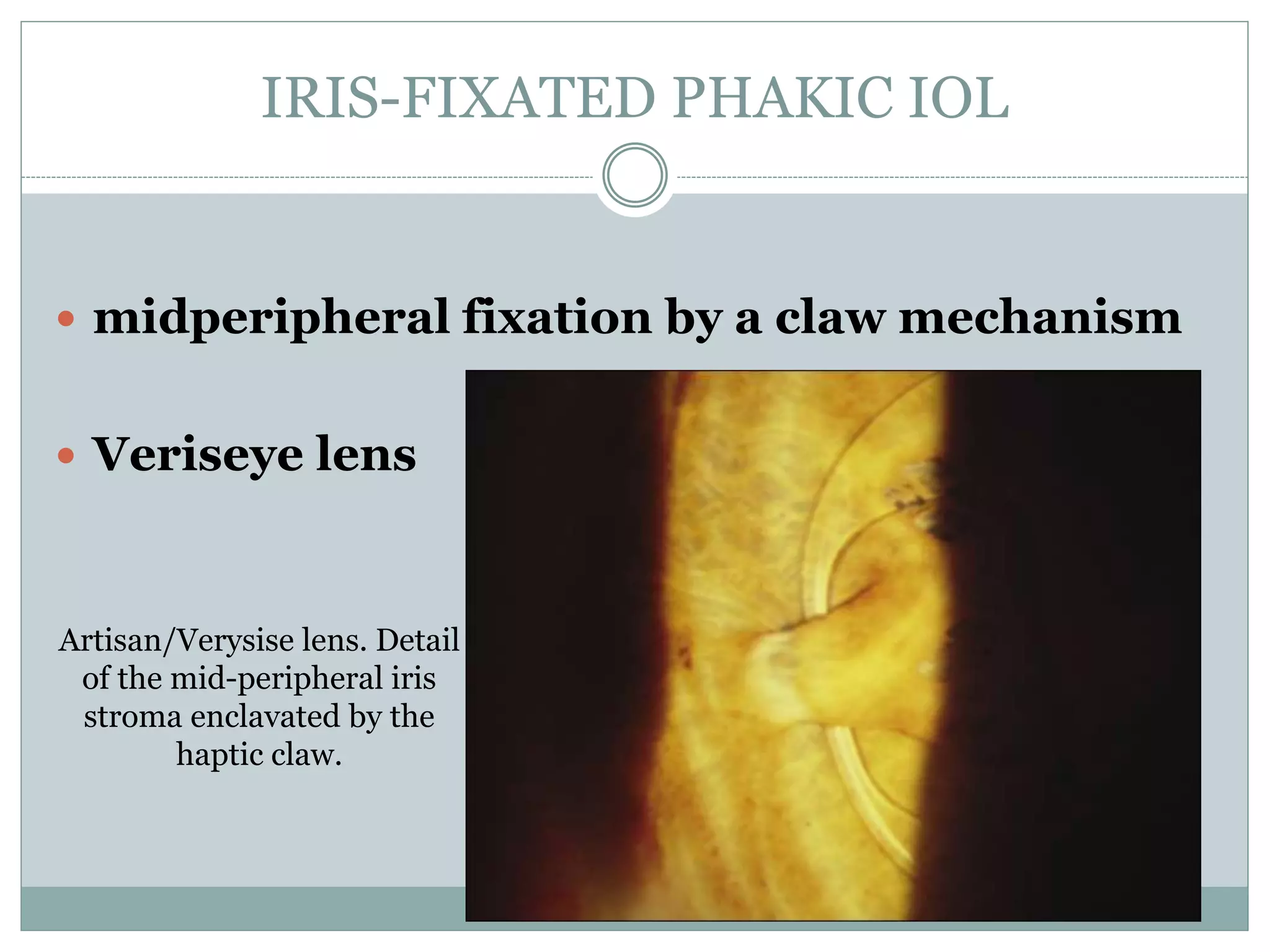
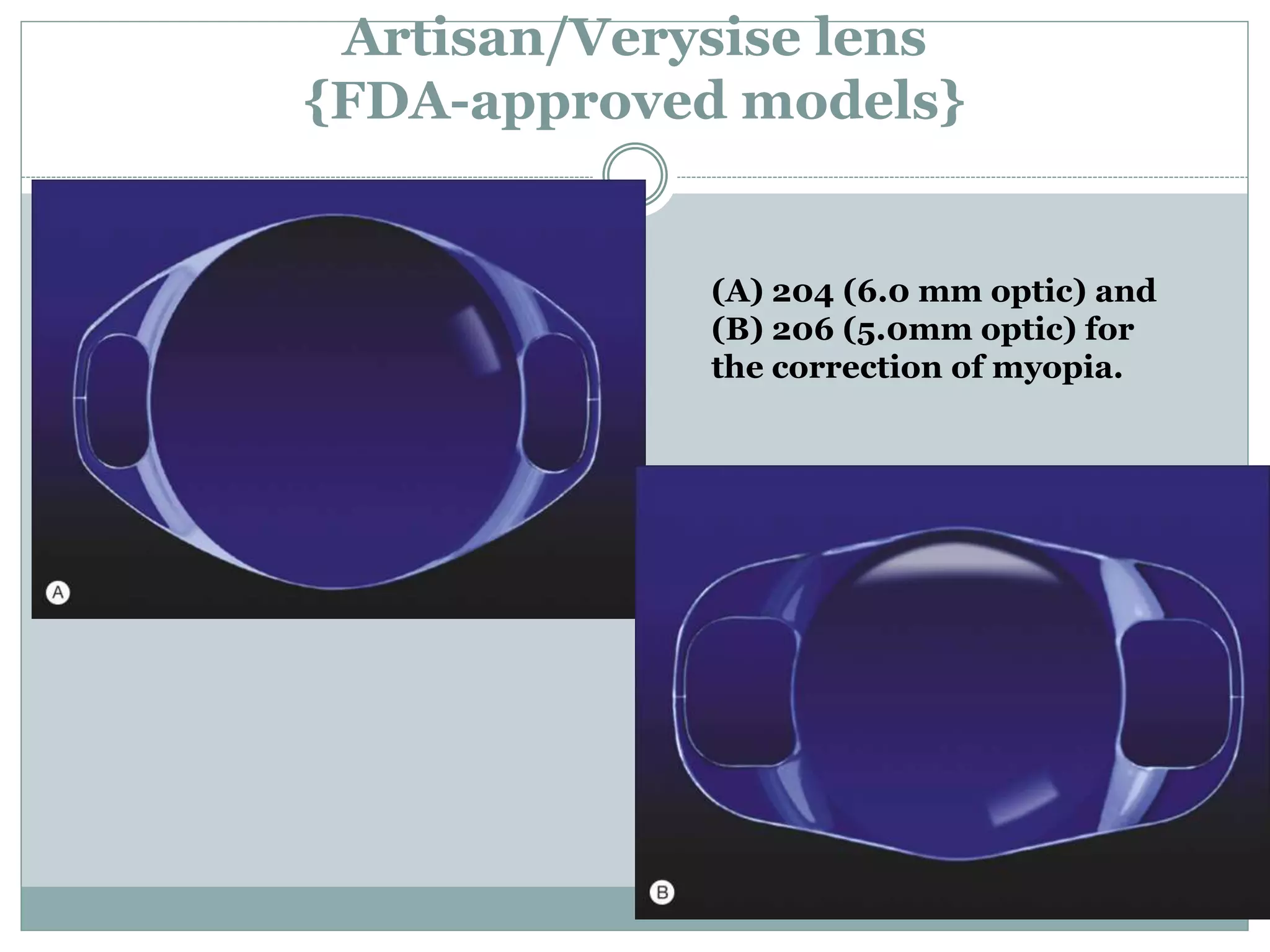
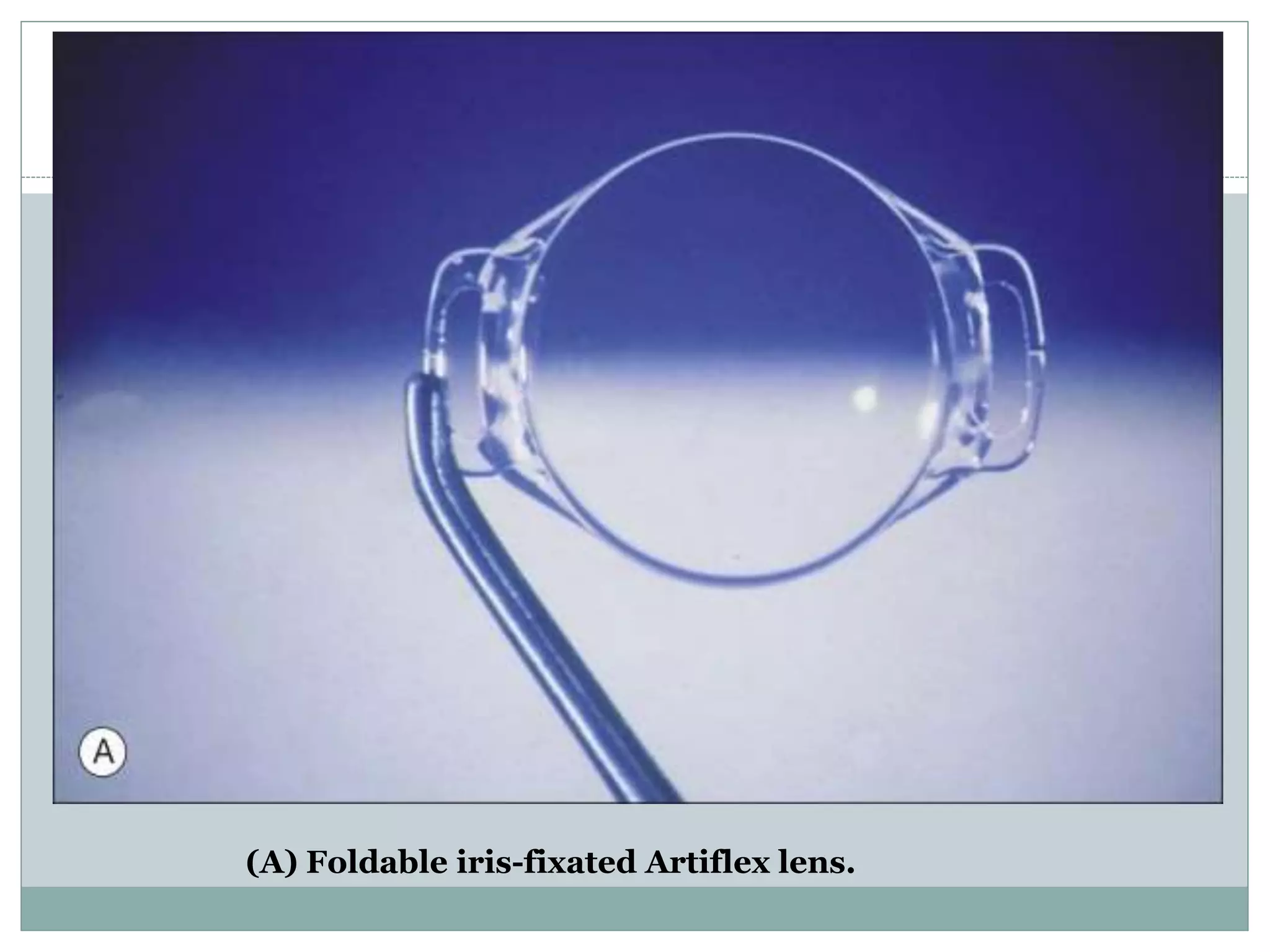
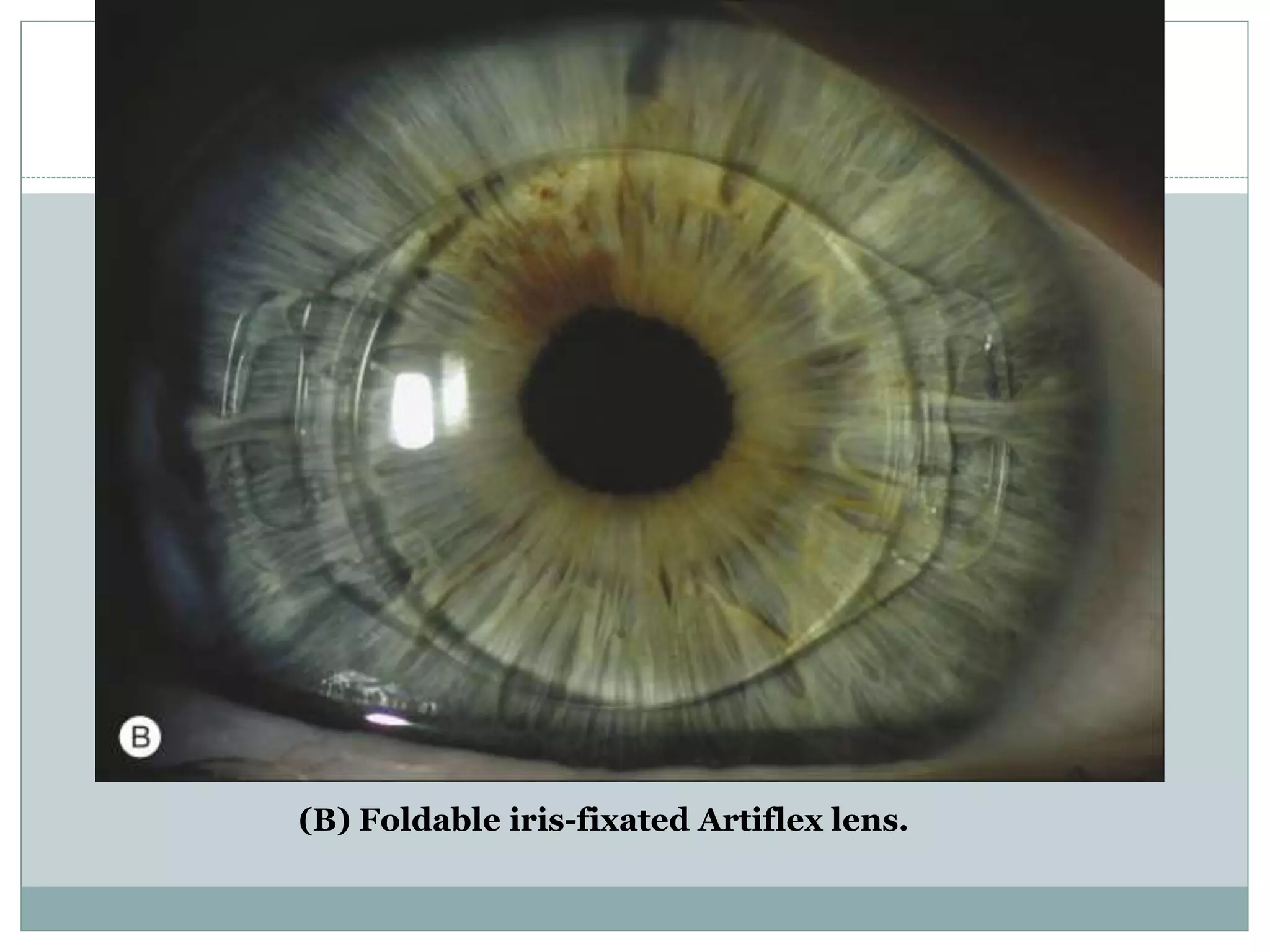
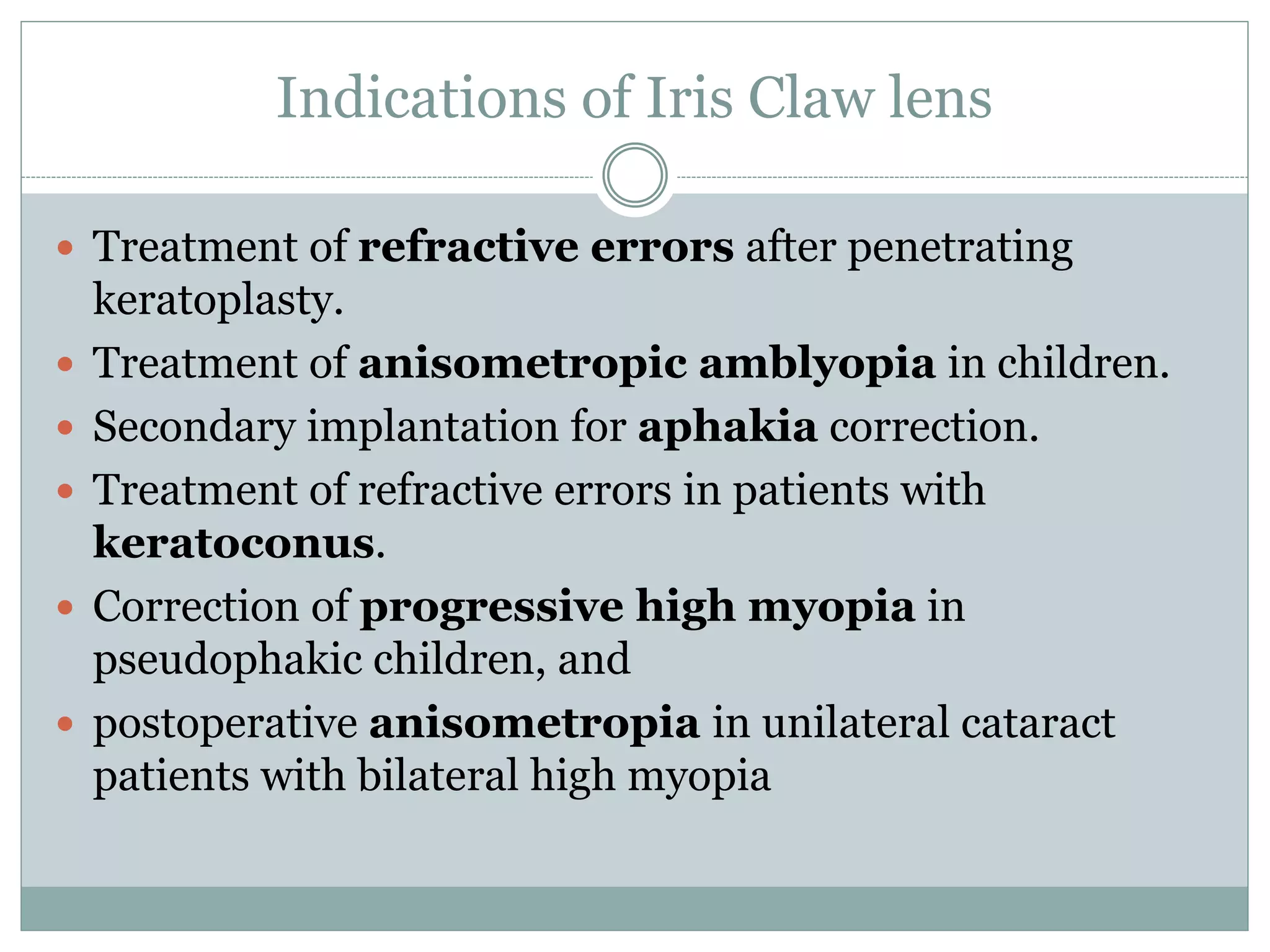
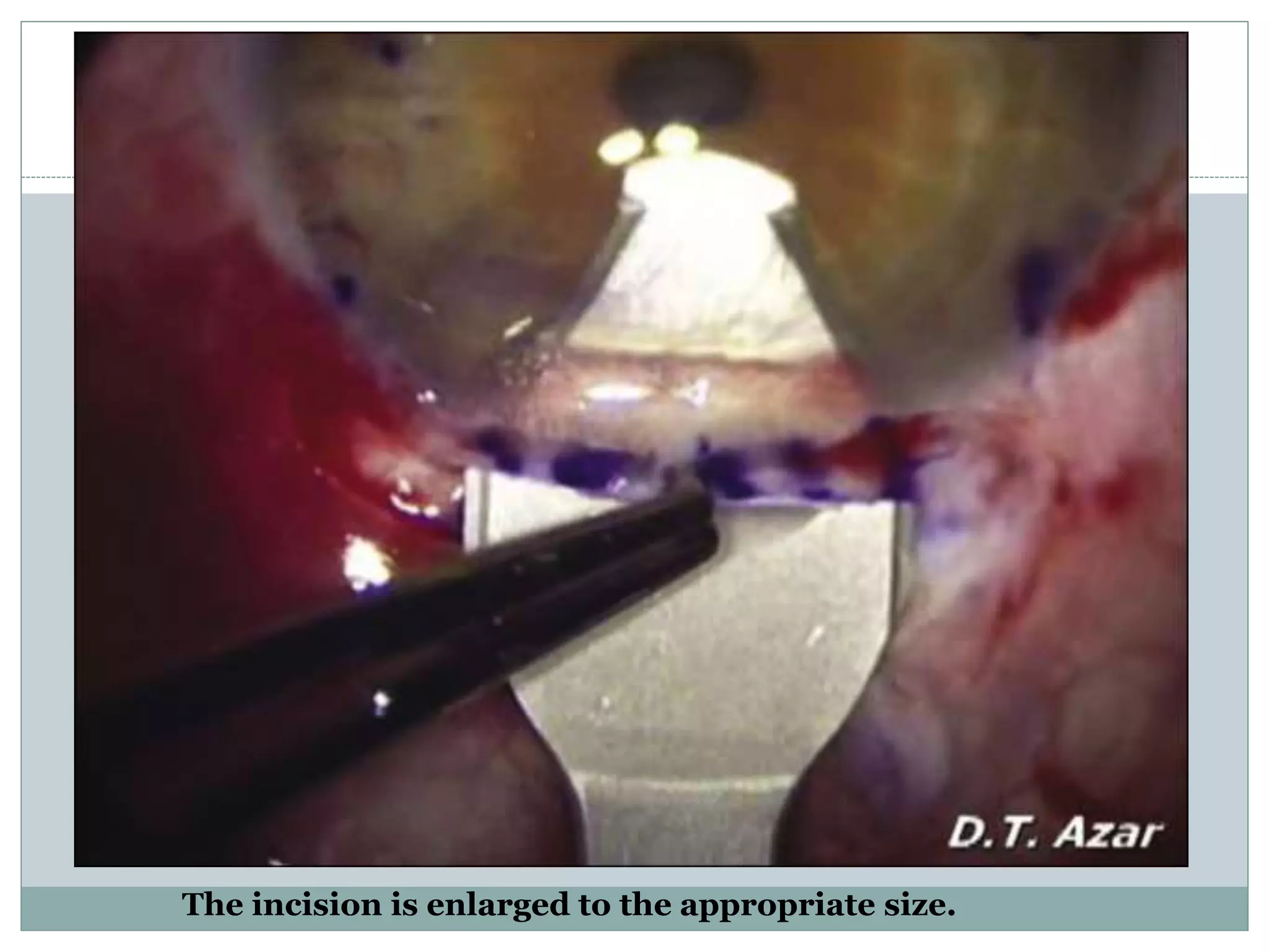
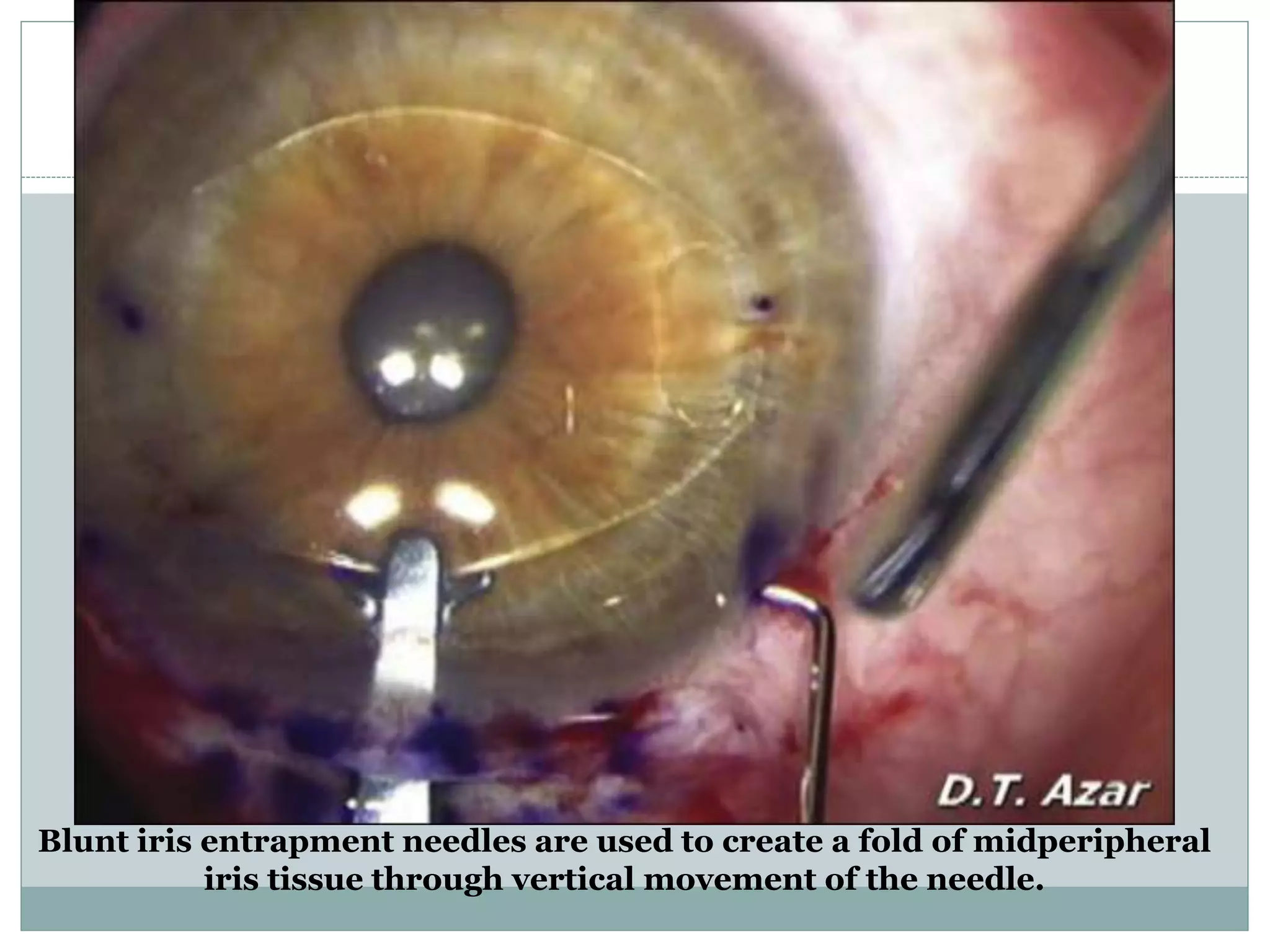
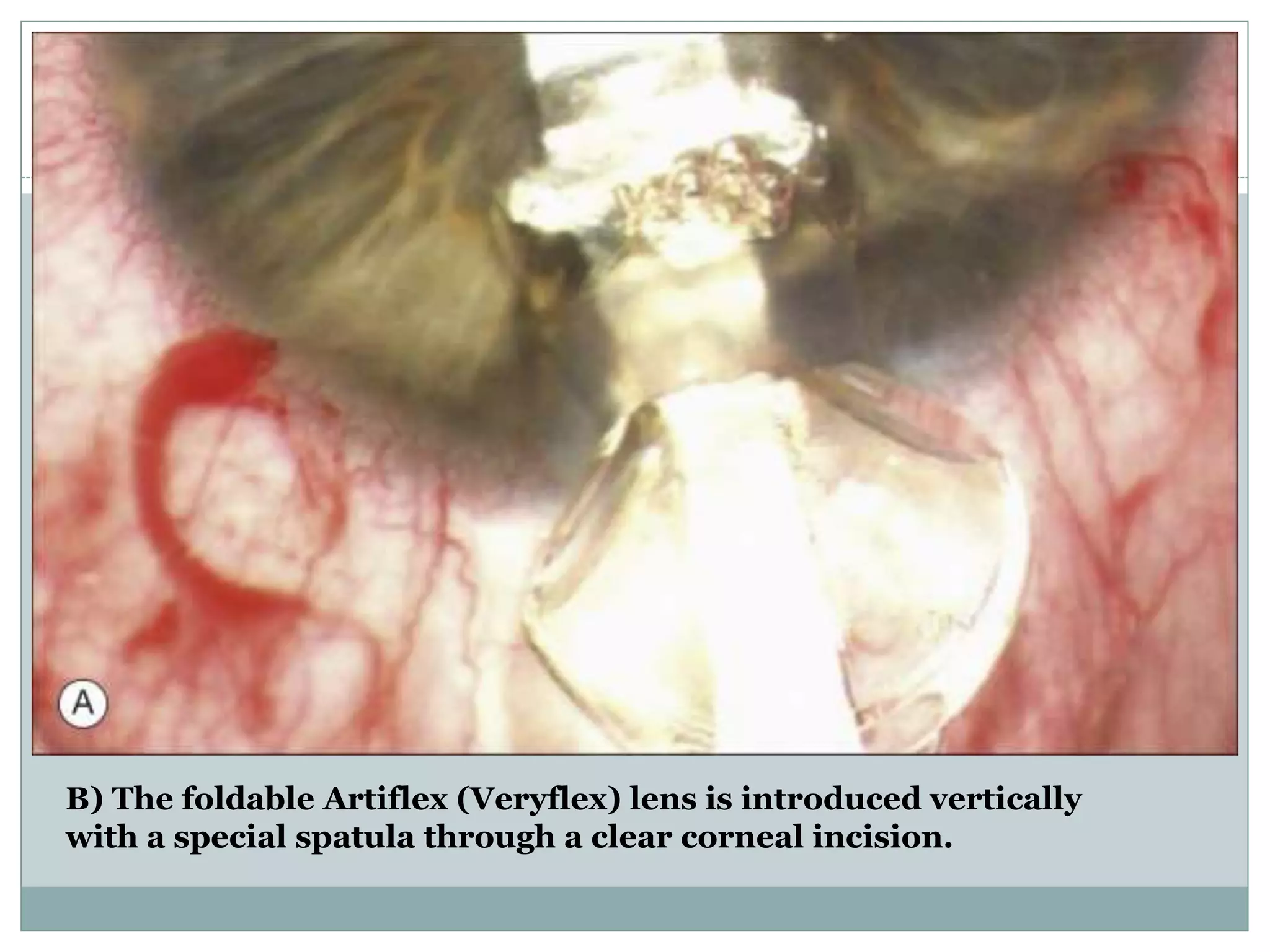
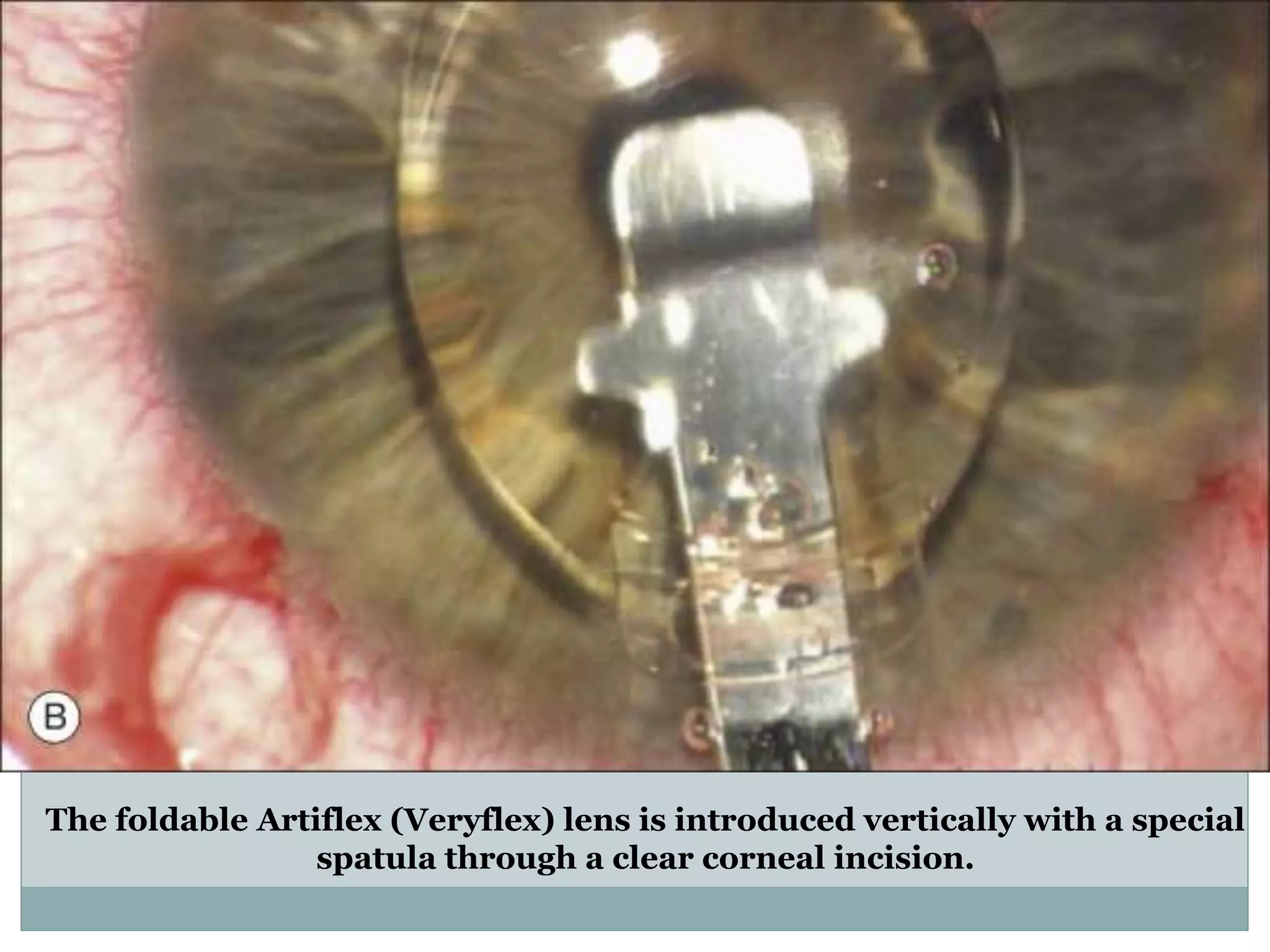
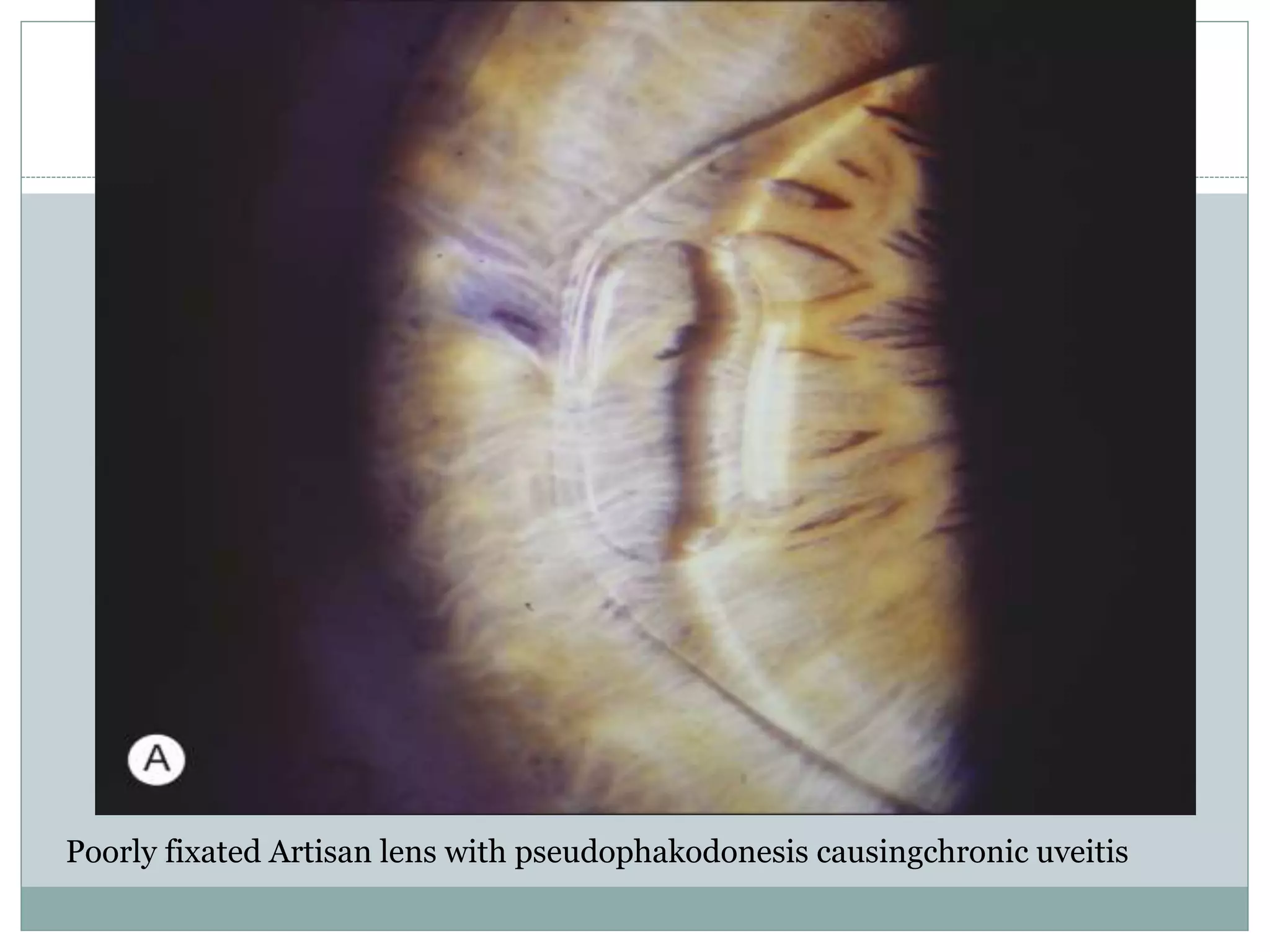
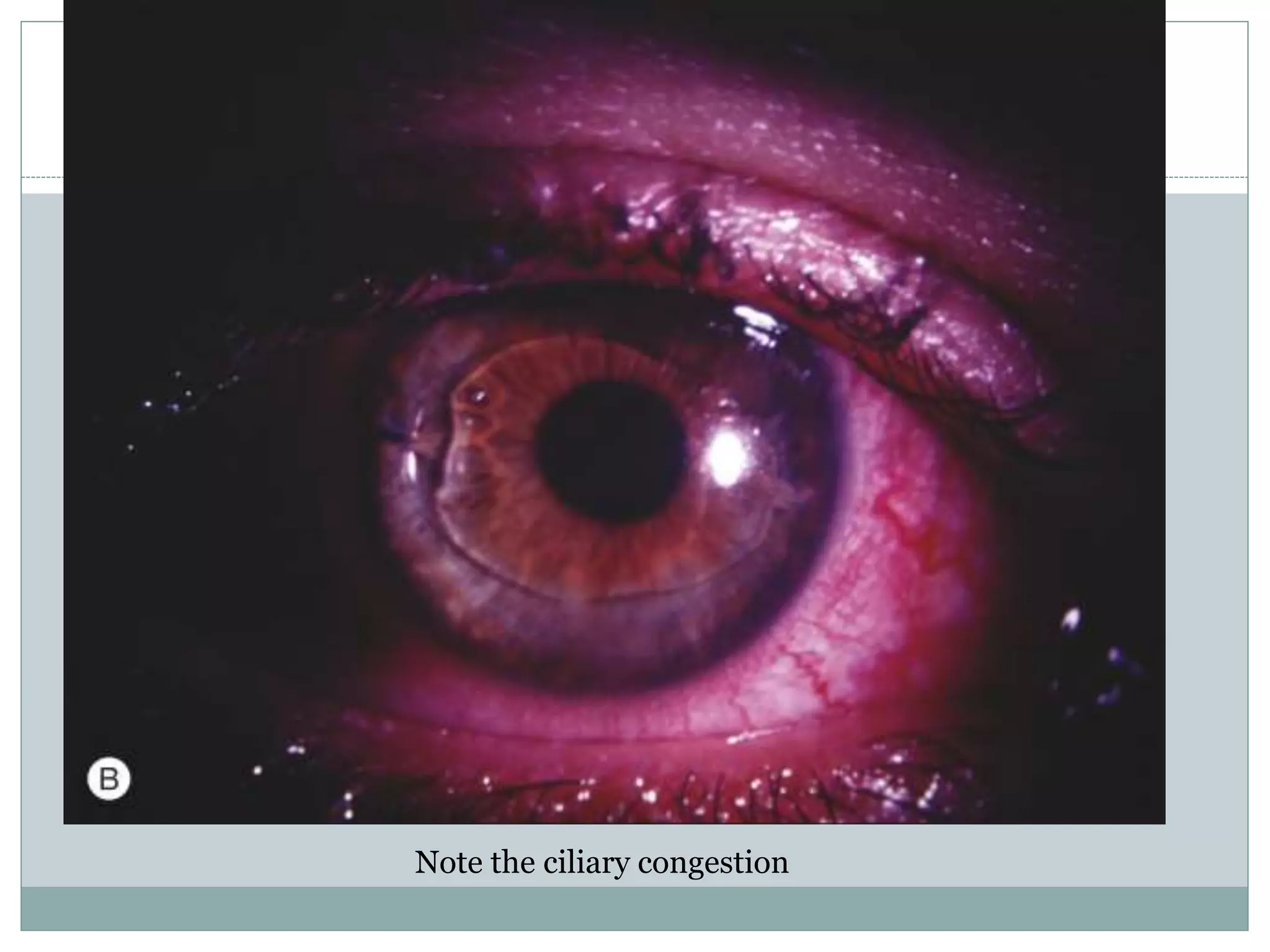
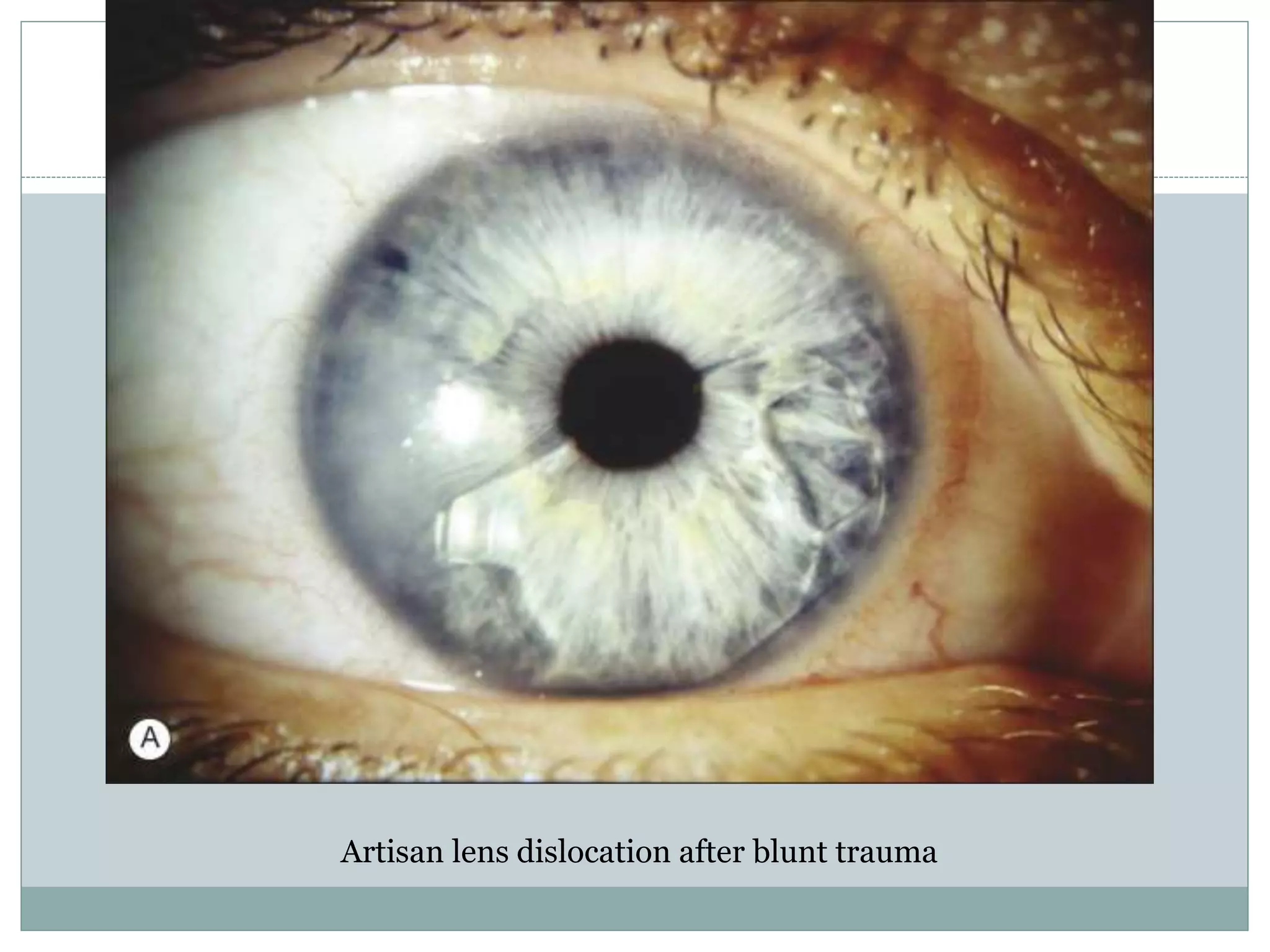
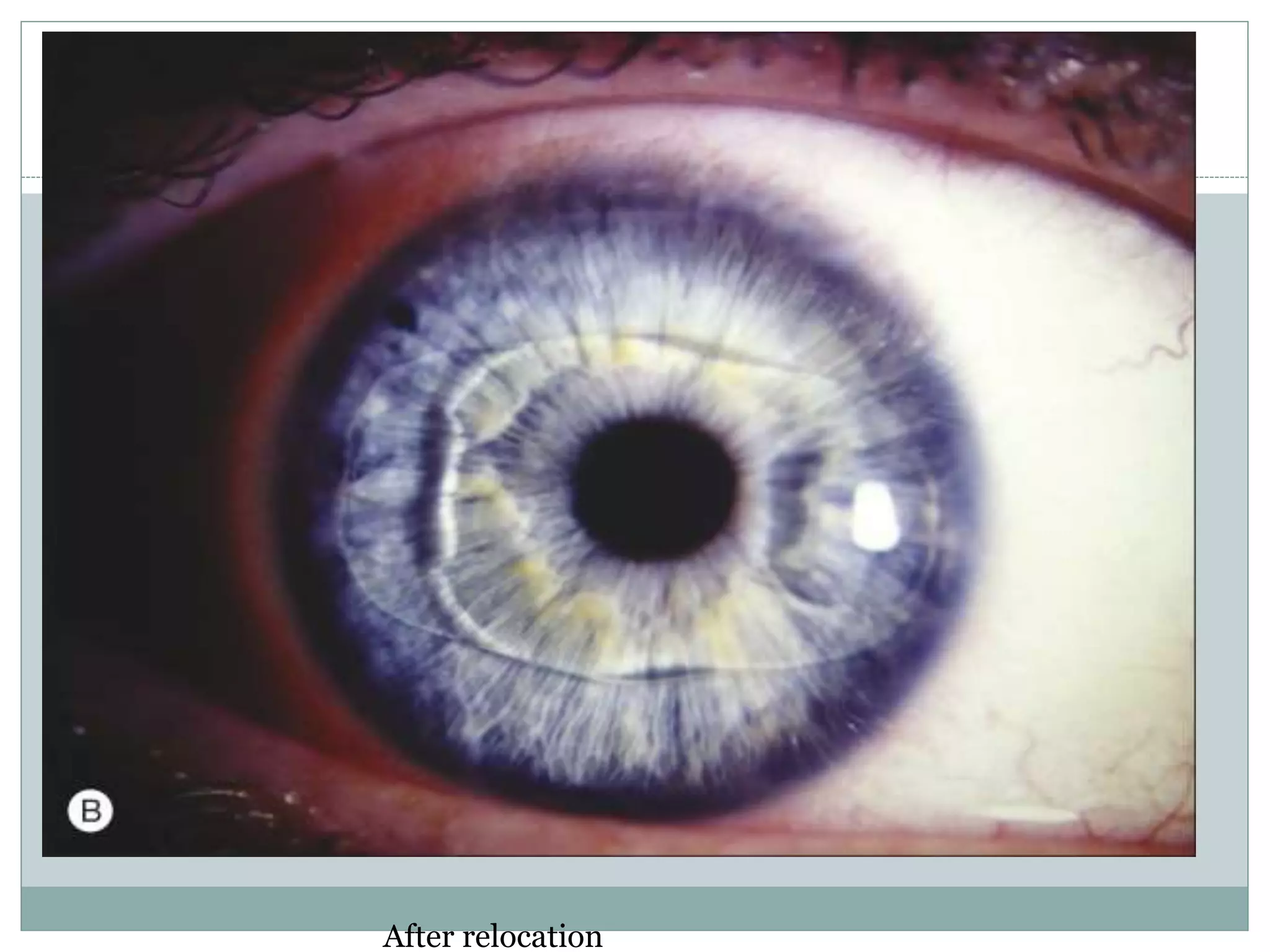
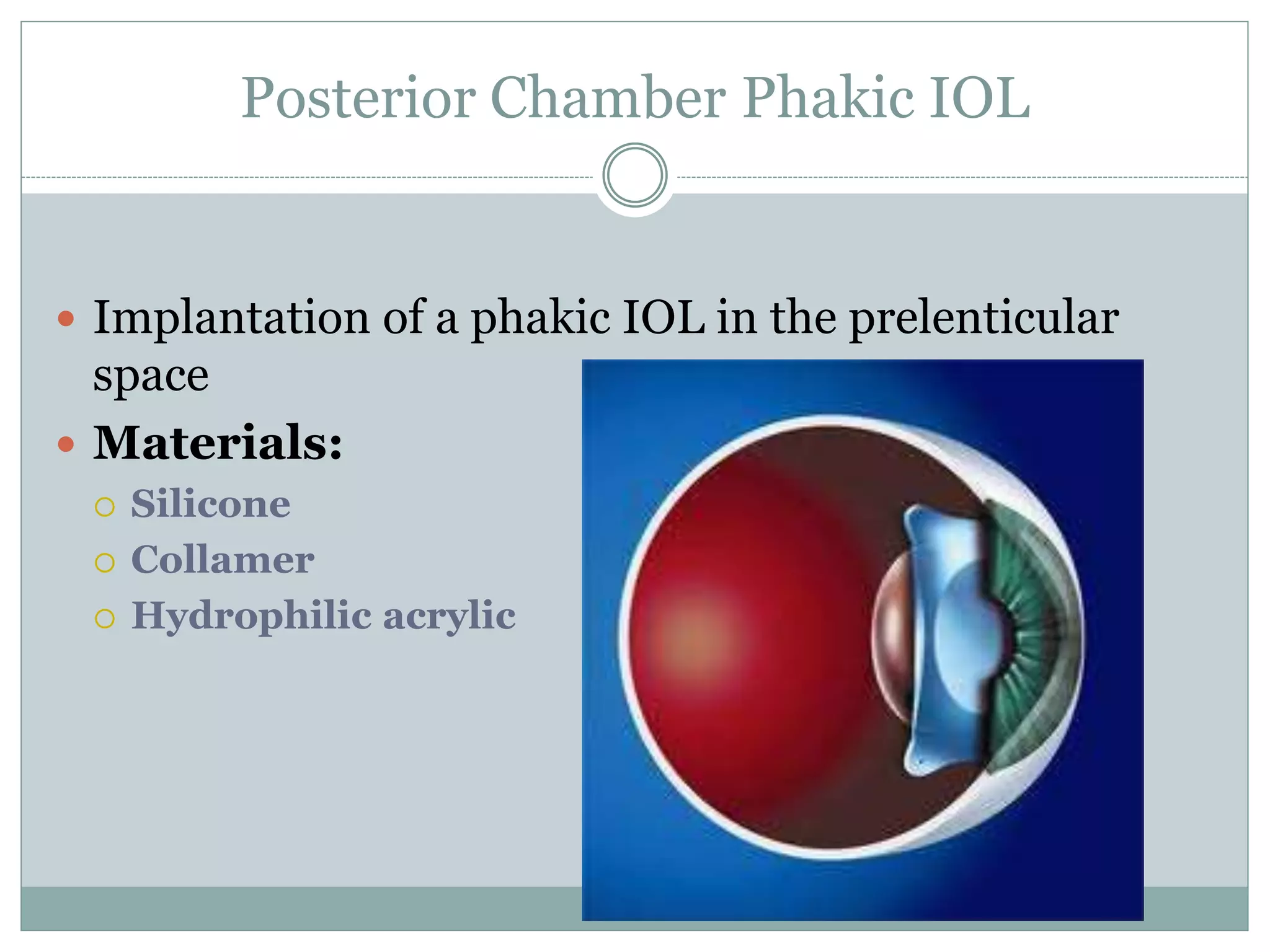
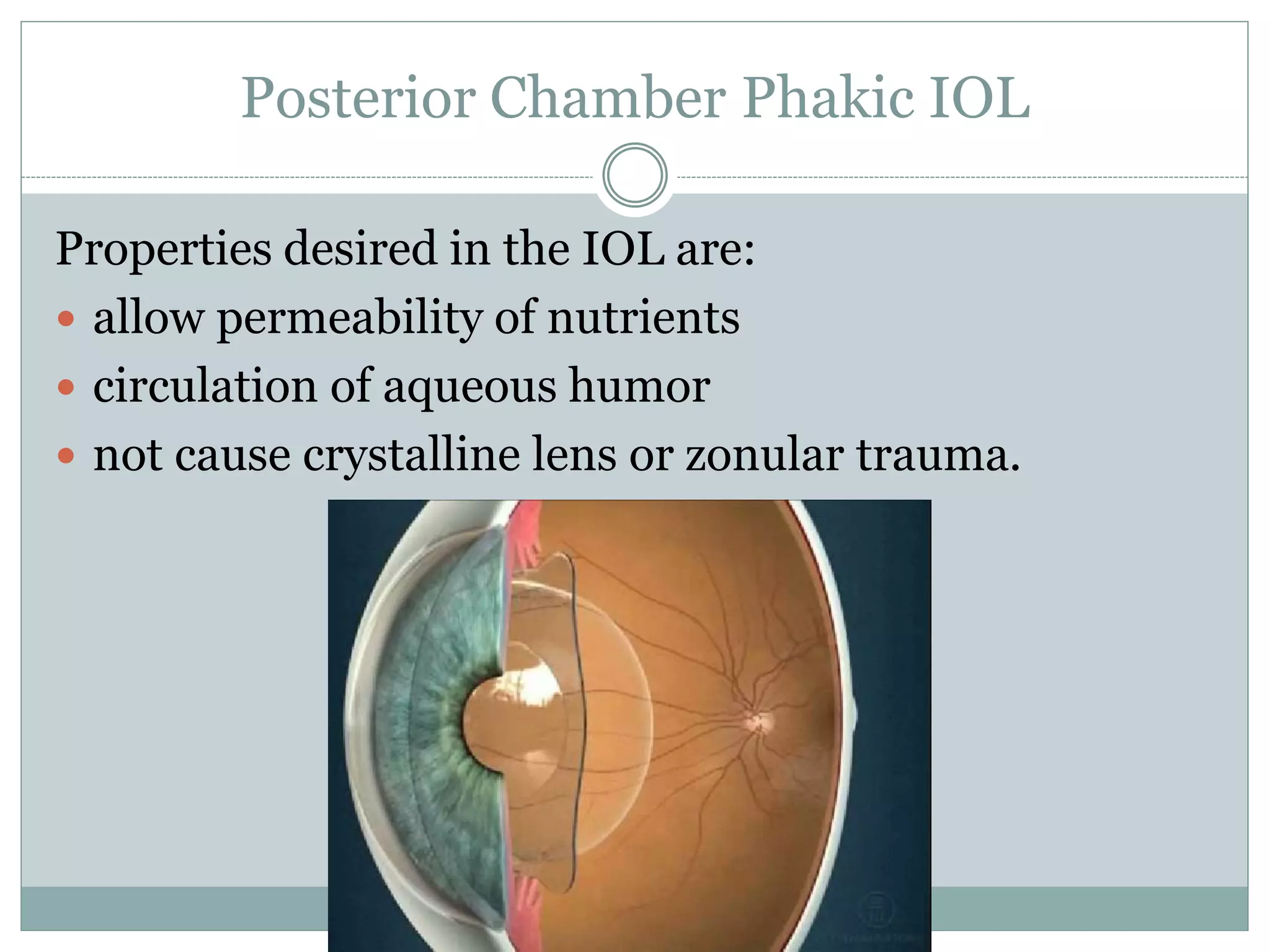
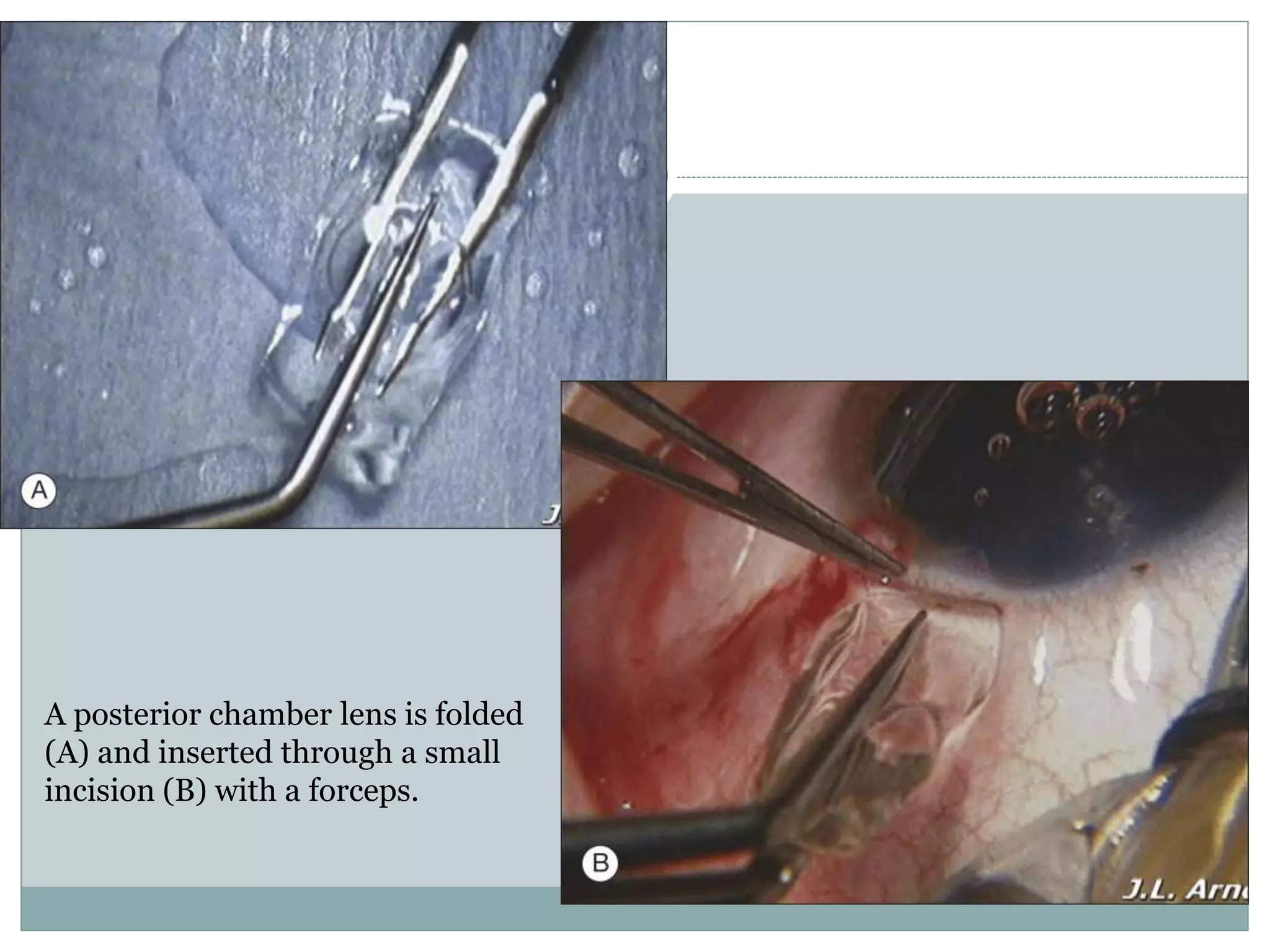
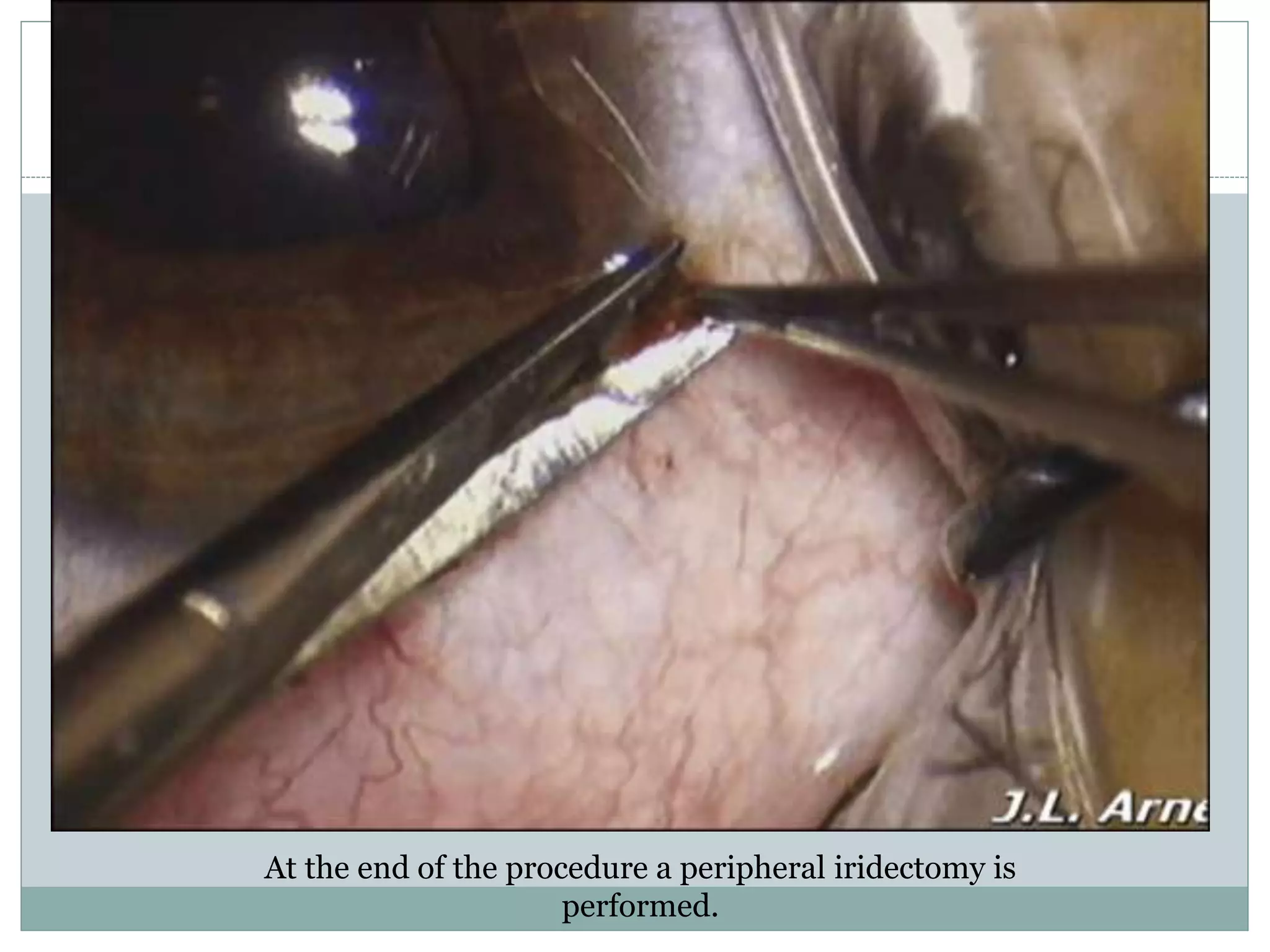
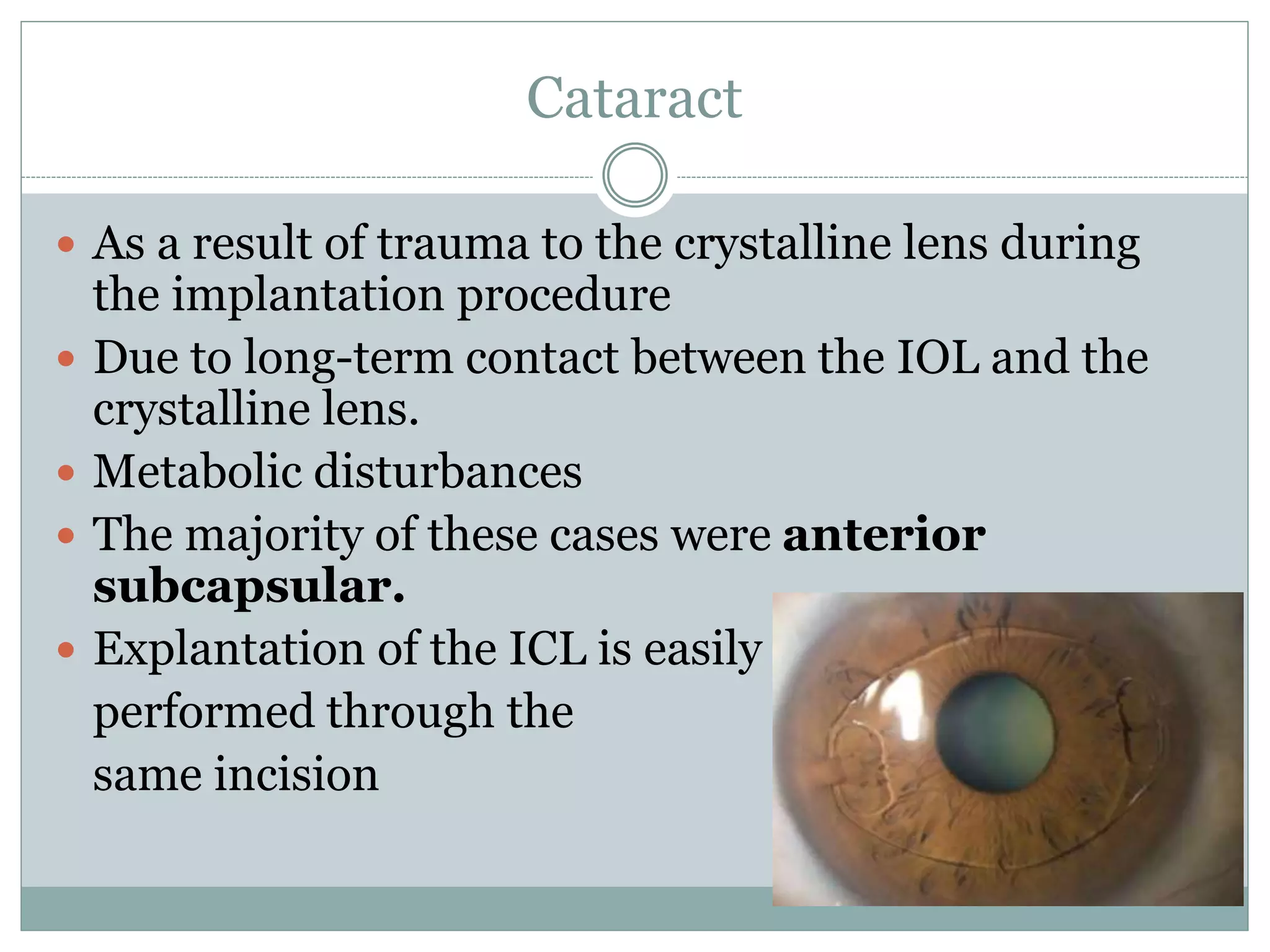
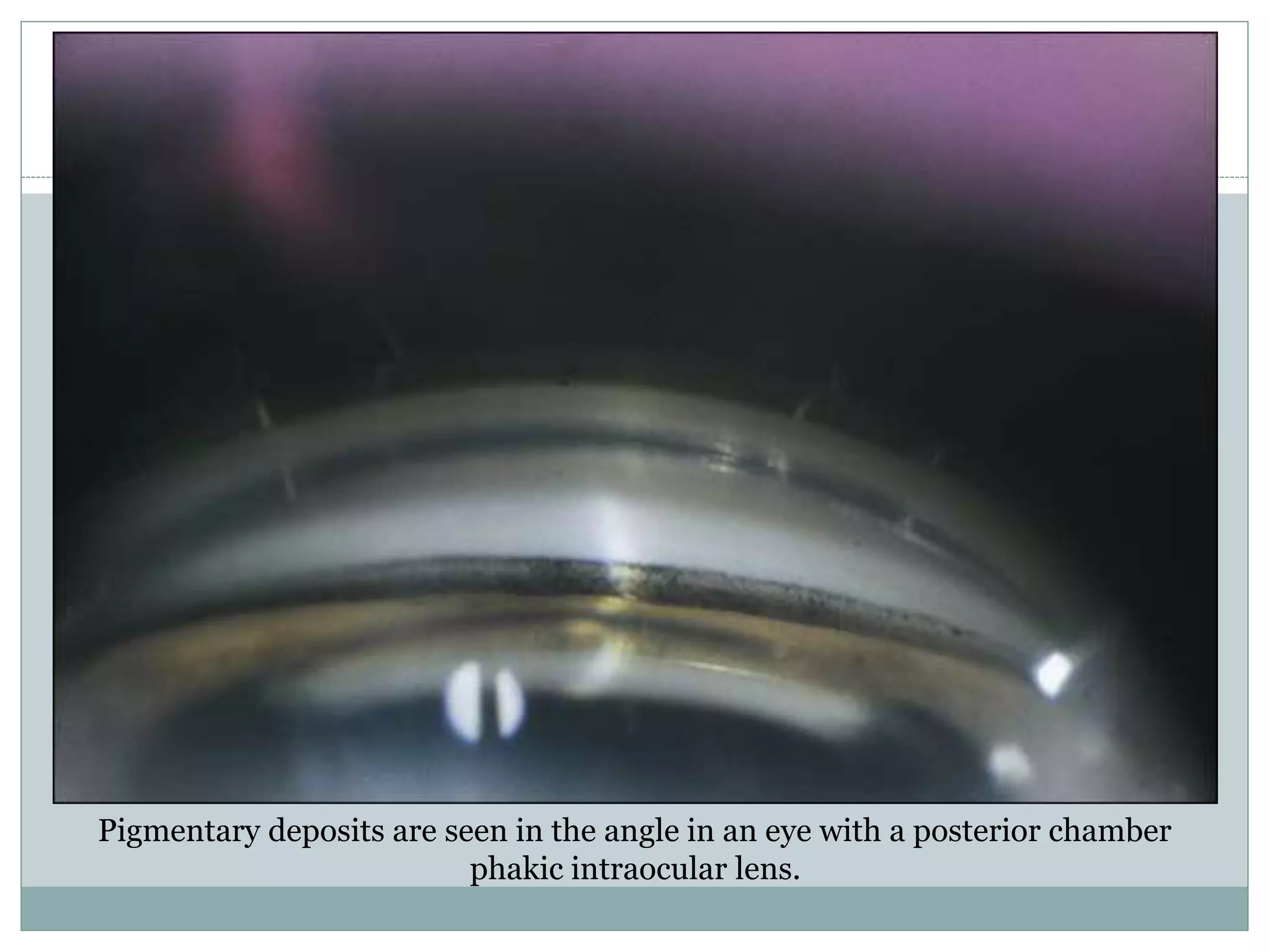
This document provides information on various types of phakic intraocular lenses (IOLs) that are implanted to correct refractive errors while leaving the natural lens in place. It discusses the history of phakic IOLs and describes anterior chamber angle-supported IOLs, iris-fixated IOLs, and posterior chamber phakic IOLs. The key points covered include the indications, surgical procedures, power calculation methods, potential complications, and advantages/disadvantages of each phakic IOL type.