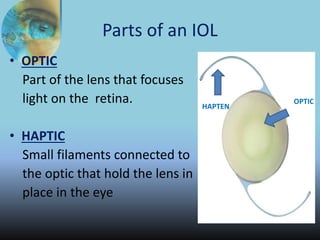
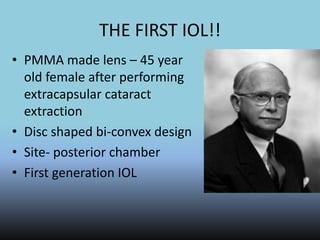
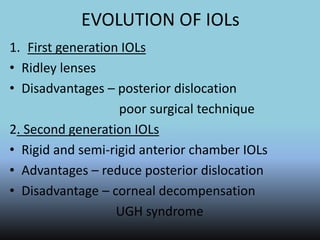
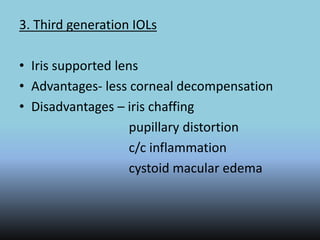
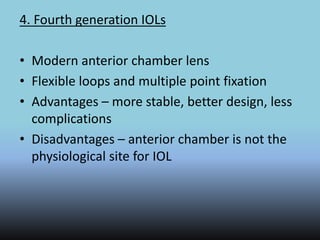
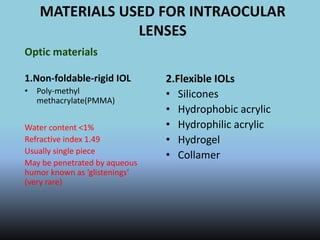
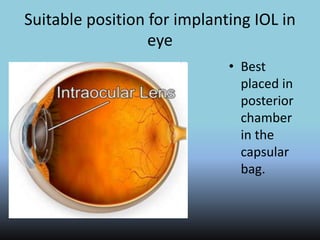
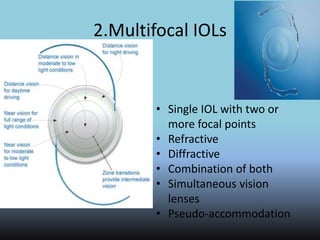
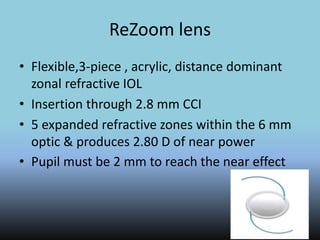
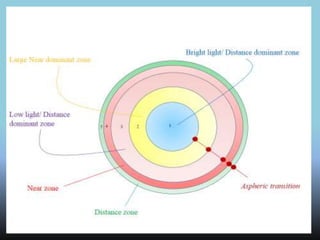
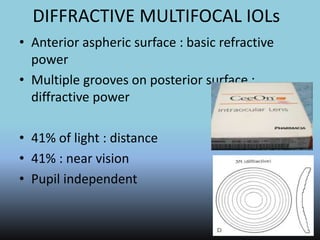
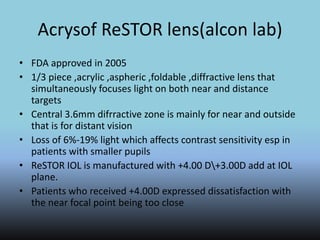
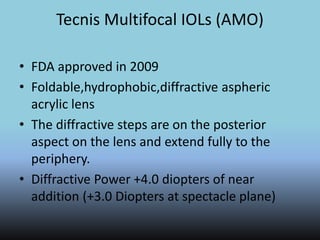
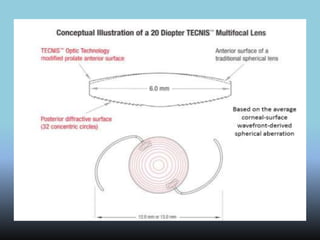
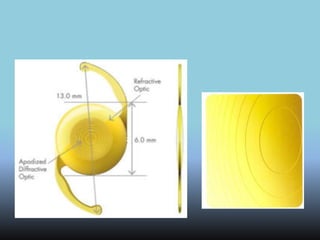
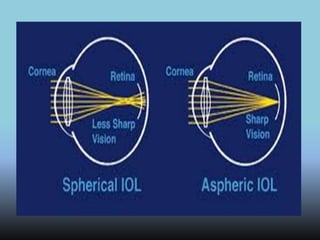
1) Intraocular lenses (IOLs) are artificial lenses implanted during cataract surgery to replace the clouded natural lens and correct vision. 2) IOLs have evolved over generations from rigid PMMA lenses to modern foldable designs made of silicone, acrylic, or hydrogel materials. 3) IOLs can be mono-focal, providing a single vision correction, or multi-focal, attempting to provide both near and distance vision without glasses. Accommodating IOL designs also aim to restore the eye's ability to focus at different distances.