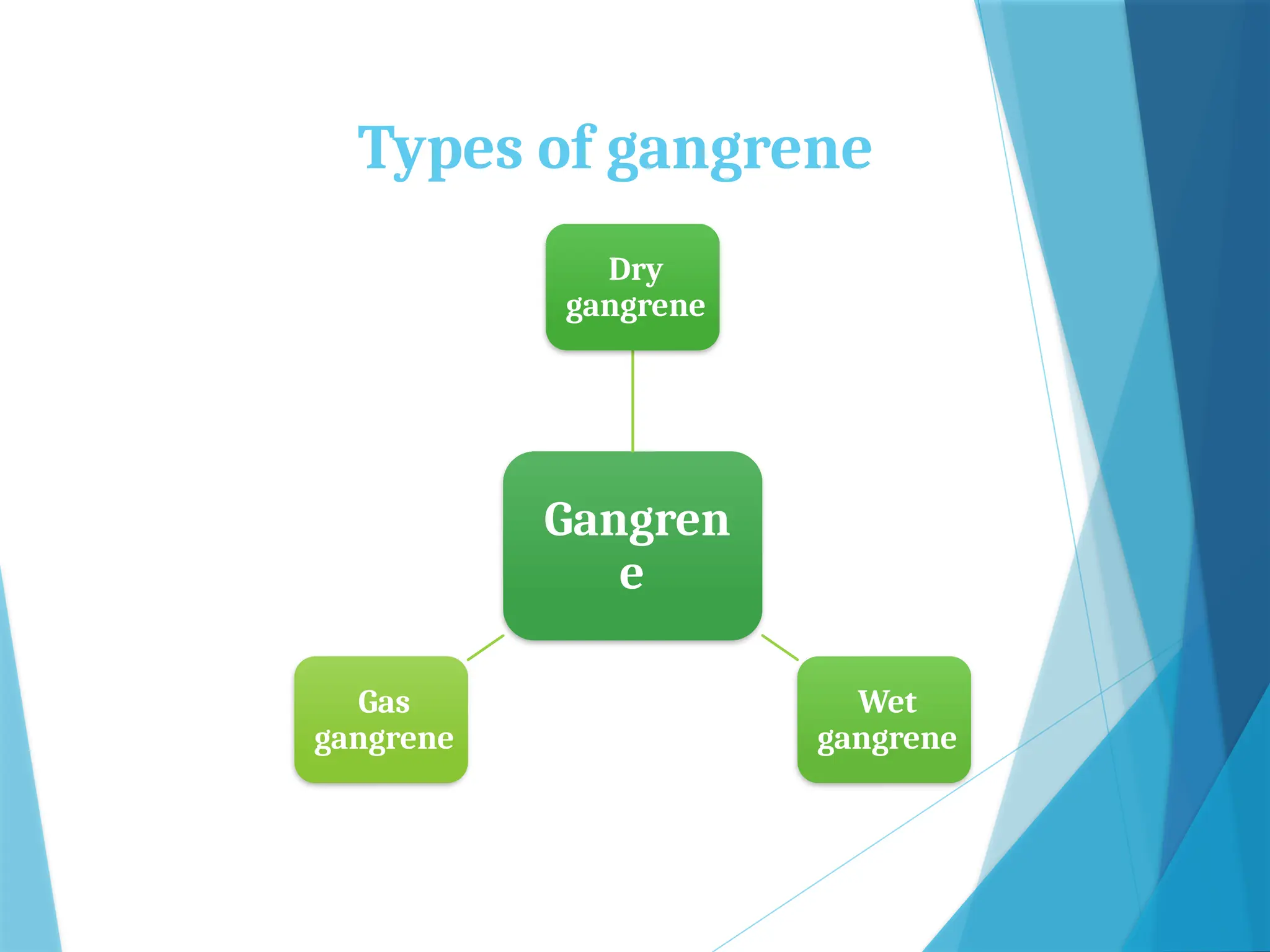
The document discusses cell injury, detailing its causes, types, and pathogenesis, distinguishing between reversible and irreversible injury. Reversible injuries may allow for recovery if harmful stimuli are removed, while irreversible ones lead to cell death through mechanisms such as necrosis or apoptosis. It also elaborates on various types of necrosis and gangrene, outlining their characteristics, causes, and clinical features.