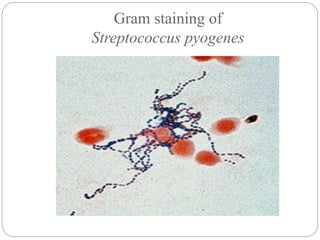
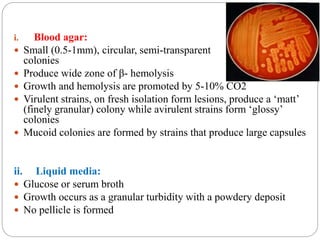
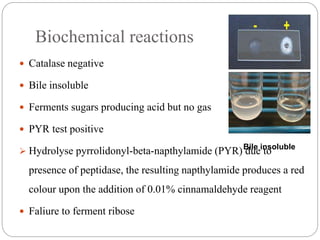
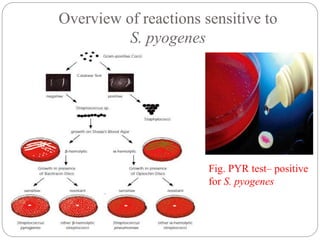
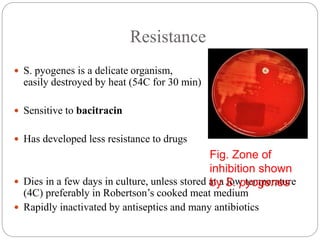
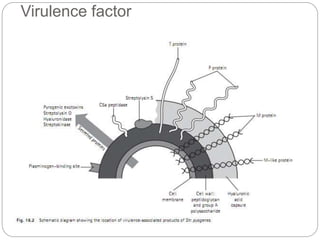
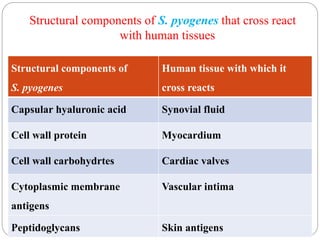
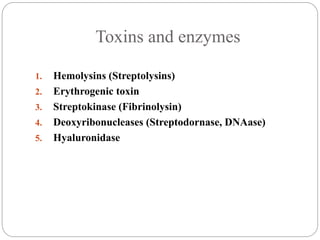
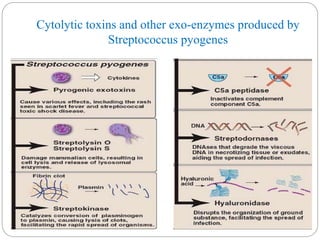
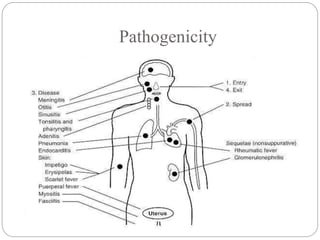
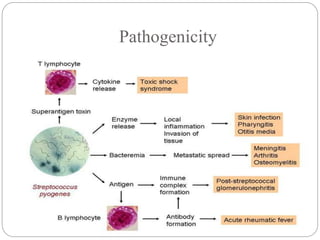
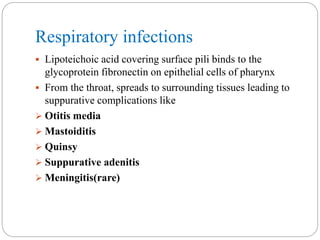
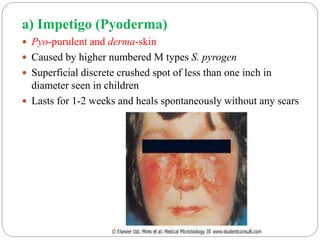
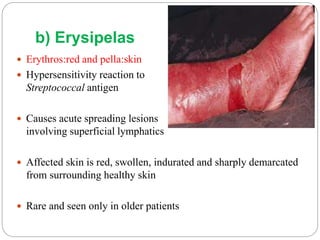
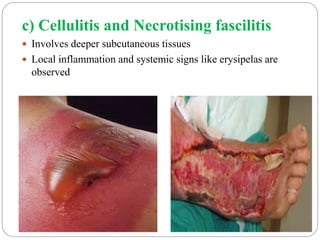
Streptococcus pyogenes is a Gram-positive bacterium that can cause a variety of infections in humans. It commonly colonizes the throat and skin. It produces toxins and enzymes that contribute to its virulence and ability to cause disease. S. pyogenes can cause suppurative infections like pharyngitis, impetigo, and necrotizing fasciitis. It can also cause non-suppurative sequelae after infection like acute rheumatic fever and glomerulonephritis. Diagnosis involves culturing samples on blood agar and testing for sensitivity to bacitracin. Treatment involves antibiotics like penicillin. Prevention focuses on proper treatment of streptococcal infections to reduce risk of