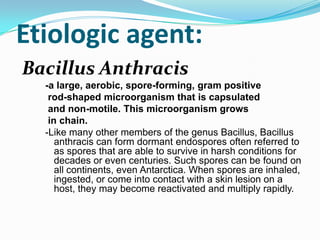
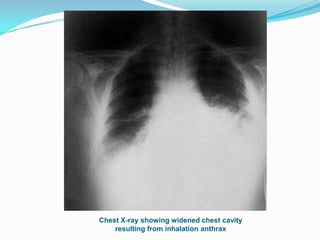
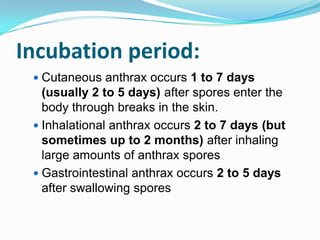
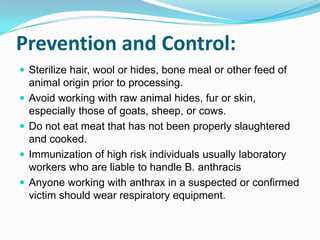
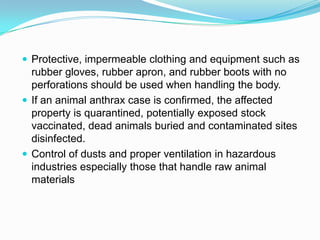
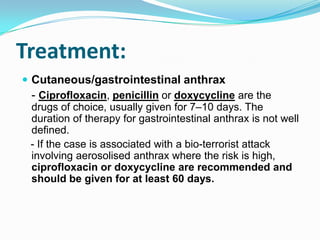
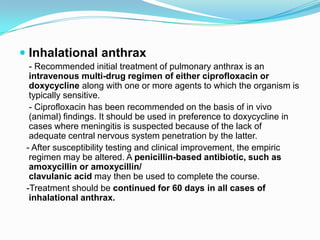
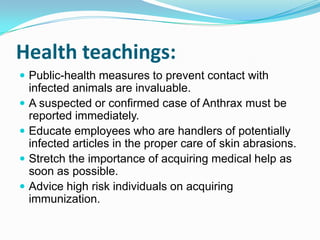
Bacillus anthracis is the etiologic agent that causes the zoonotic disease anthrax. It forms spores that can survive in soil for decades and become activated when they enter the body. There are three main forms depending on route of entry: cutaneous (skin), inhalational (lungs), and gastrointestinal (ingestion). Symptoms vary but can include lesions, fever, vomiting and respiratory distress. Transmission occurs through contact with infected animals/products or inhaling spores. Treatment involves antibiotics like ciprofloxacin or doxycycline for 7-60 days. Prevention involves proper animal product handling, hygiene and immunization of high risk groups.