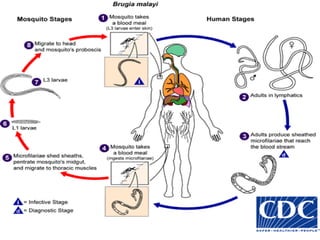
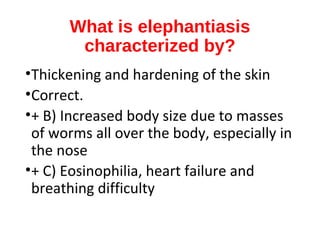
Lymphatic filariasis, also known as elephantiasis, is caused by parasitic roundworms that are spread by mosquitoes and black flies. It affects over 120 million people worldwide. The parasites block the lymphatic system leading to swelling in the limbs and genitals. Diagnosis was difficult previously but can now be made through blood tests that detect parasites or antibodies. While some infected individuals show no symptoms, others develop severe elephantiasis characterized by thickening of the skin and limbs. Treatment aims to eliminate parasites and prevent further transmission and symptoms.















































![Prevention
•By decreasing contact between humans
and vectors or by decreasing the
amount of infection the vector can
acquire
•Population: through reducing the
numbers of mosquito vectors
•2-drug treatment regimens (selecting
among albendazole and either
ivermectin or diethylcarbamazine [DEC])](https://image.slidesharecdn.com/filarisisteaching-150916054642-lva1-app6892/85/Filariasis-53-320.jpg)