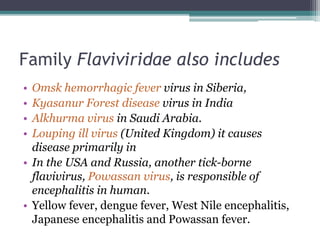
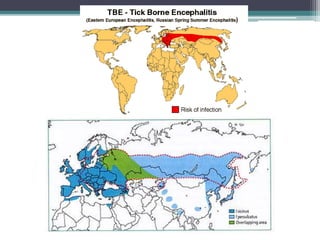
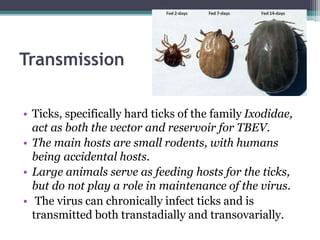
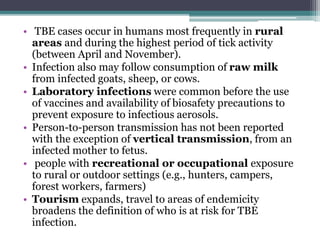
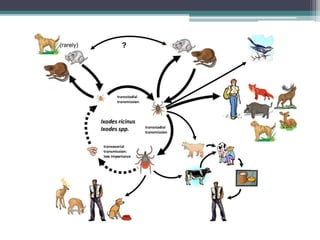
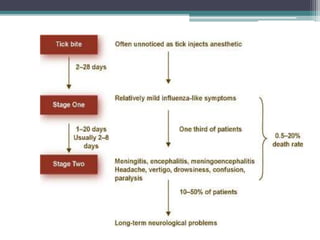
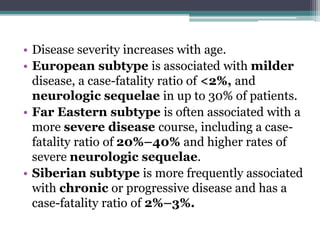
This document discusses tick-borne encephalitis (TBE), a viral infection transmitted through tick bites that affects the central nervous system. TBE is caused by the tick-borne encephalitis virus, which is endemic in parts of Europe and Asia. It describes the virus's subtypes, epidemiology, transmission cycle involving ticks and small rodents, clinical signs and symptoms including meningitis and encephalitis, diagnosis through serology or PCR, supportive treatment, and prevention through tick avoidance and the use of vaccines available in Europe.