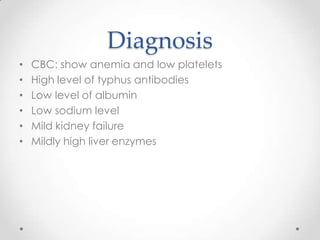
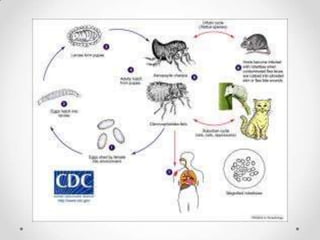
Typhus is caused by Rickettsia bacteria, which are intracellular parasites carried by arthropod hosts like lice and ticks. There are several types of typhus including epidemic typhus spread by human lice and Rocky Mountain spotted fever spread by ticks. Symptoms can range from mild to severe fever, headache, rash and organ damage. Diagnosis involves identifying the bacteria through PCR testing, antibody levels or tissue staining. Treatment is with doxycycline or chloramphenicol antibiotics.