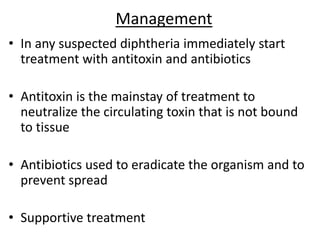
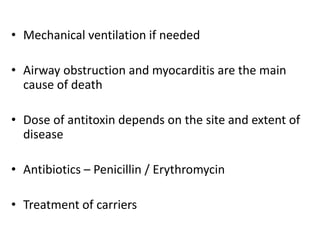
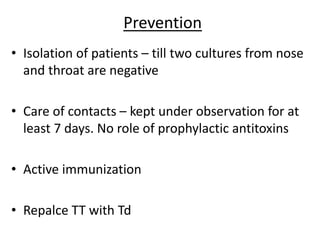
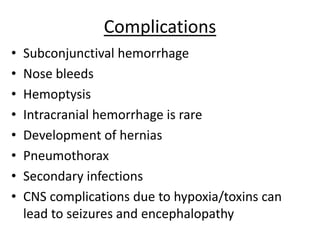
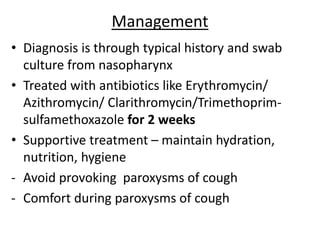
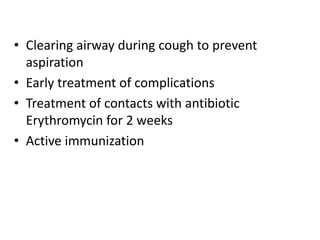
This document provides information on the bacterial infections diphtheria and pertussis. It describes diphtheria as an acute infection caused by Corynebacterium diphtheriae that produces a potent exotoxin. Clinical features include a thick gray membrane in the throat and complications affecting the heart, kidneys and nerves. Pertussis is caused by Bordetella pertussis and is characterized by paroxysmal coughing fits ending in a distinctive whoop. Both are highly contagious and can be prevented by vaccination.