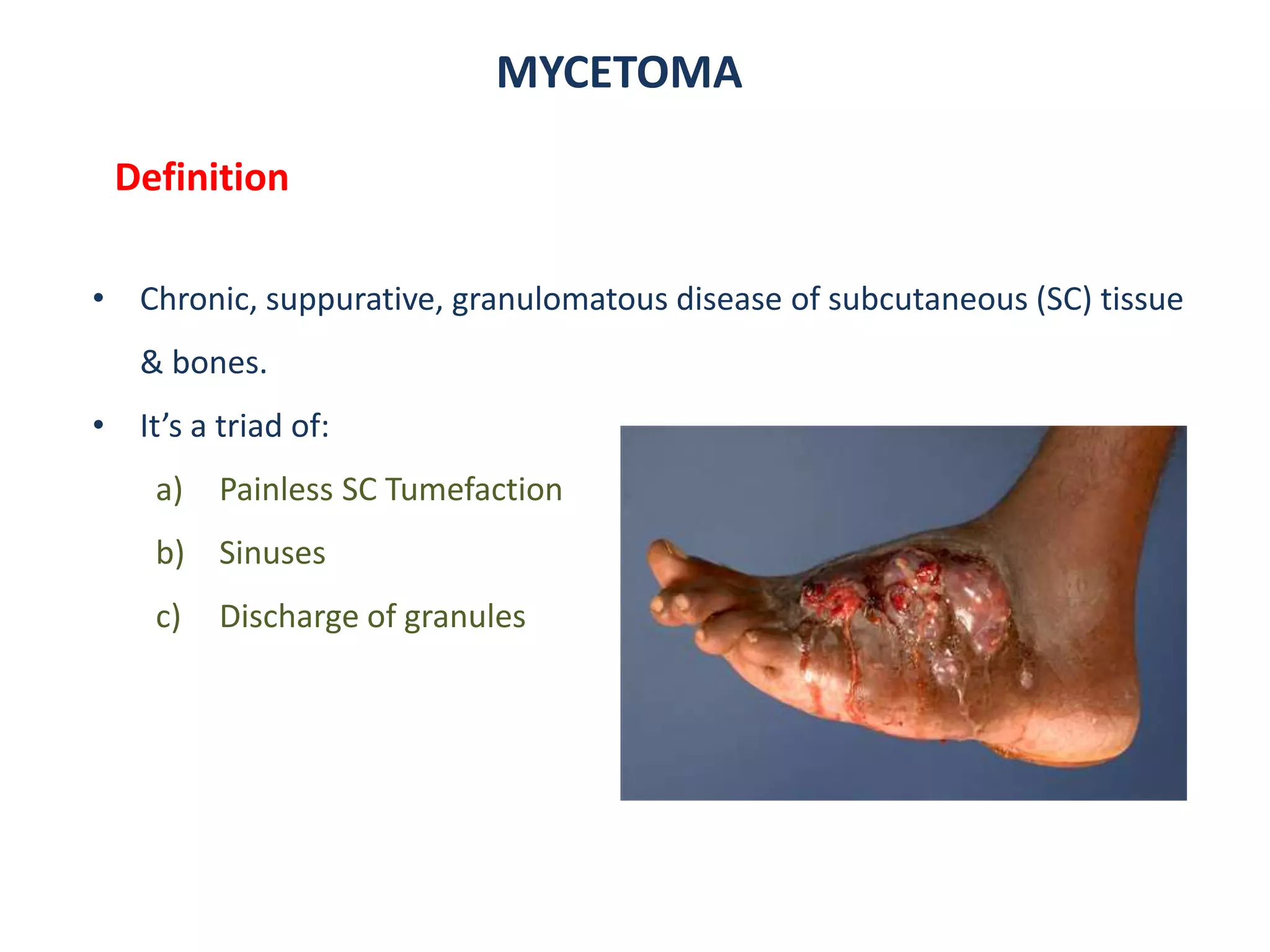
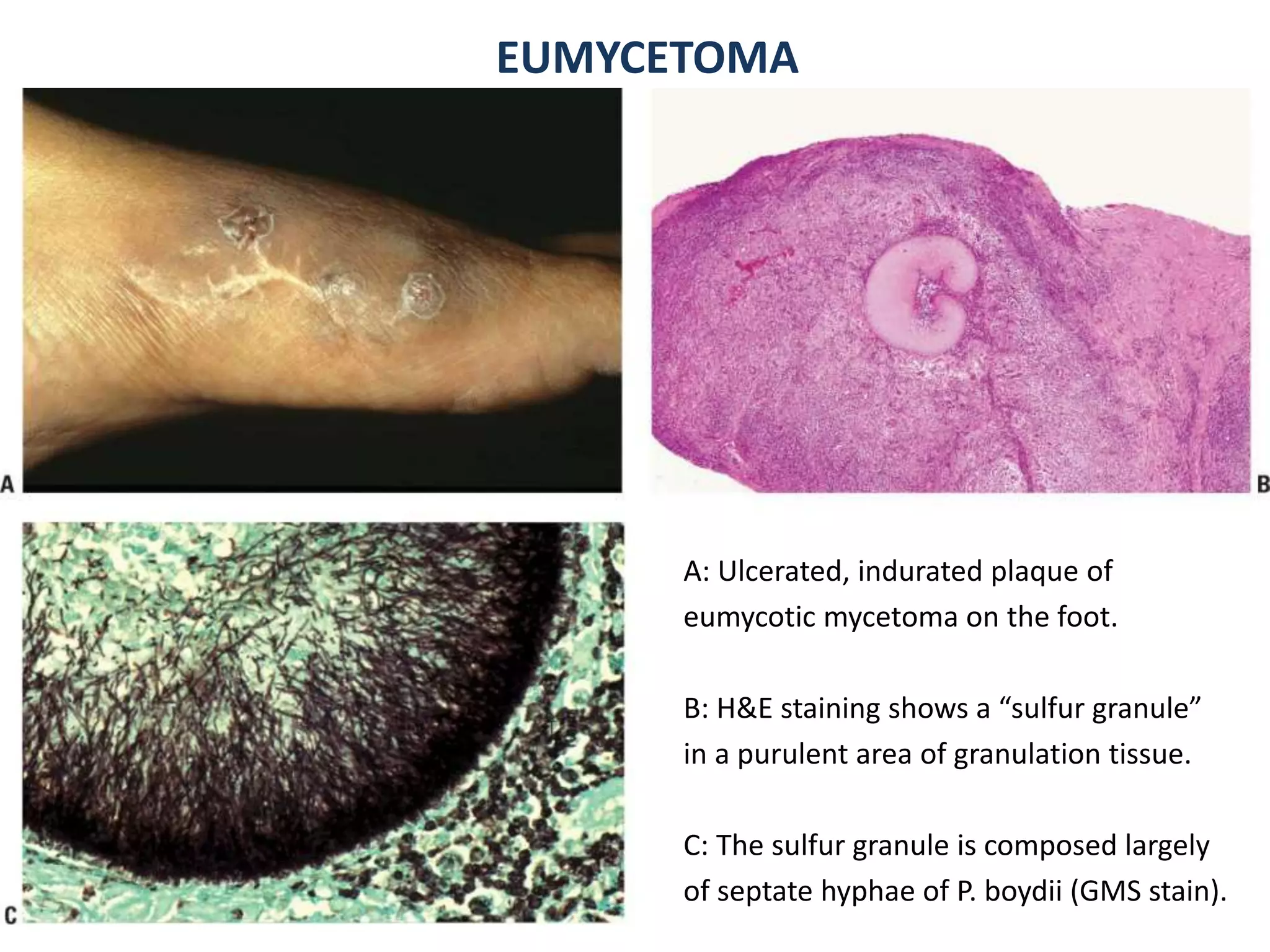
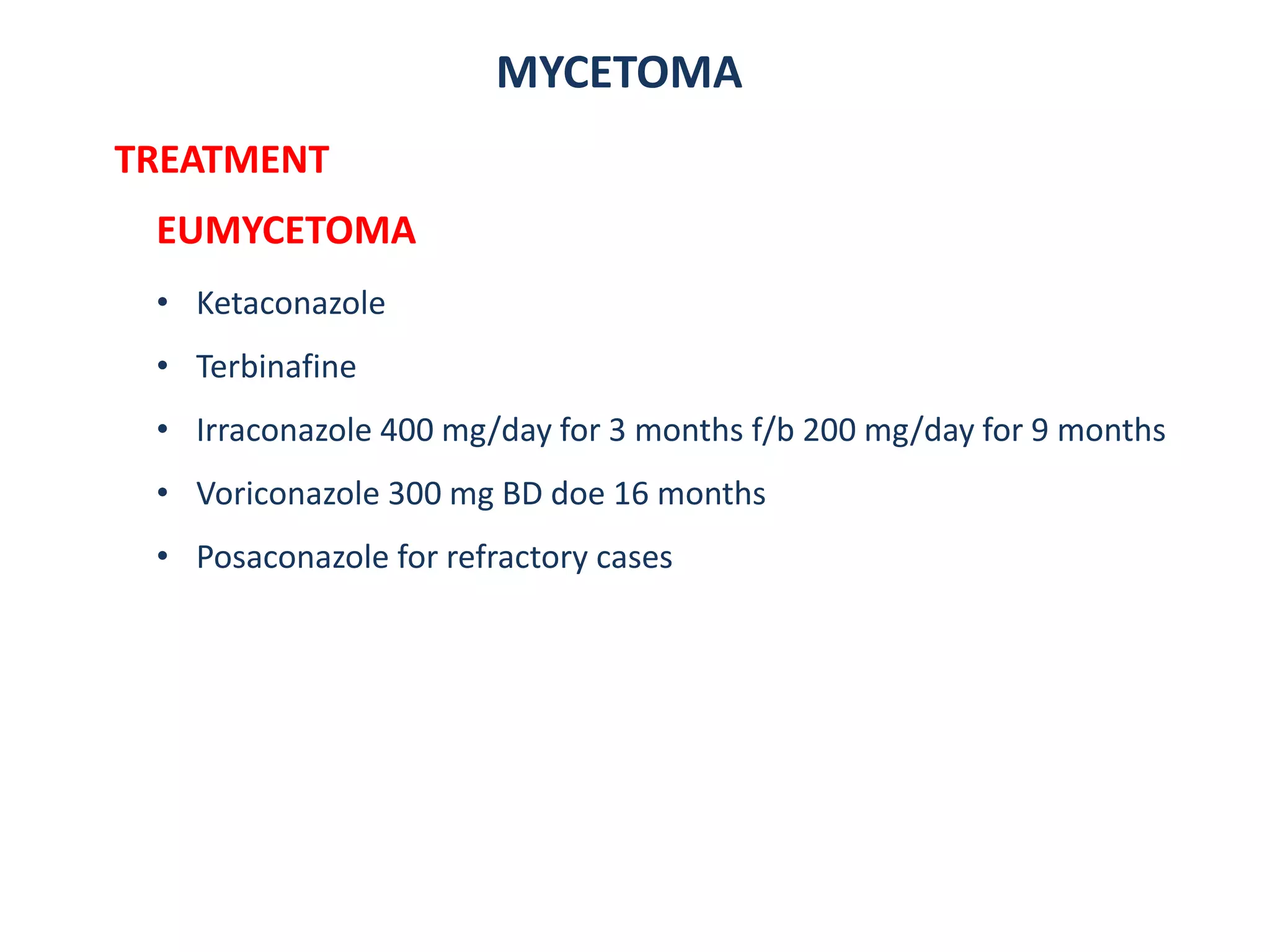
1. Mycetoma is a chronic subcutaneous infection characterized by painless swelling, sinuses, and discharge of characteristic grains. It is mostly caused by fungi (eumycetoma) or bacteria (actinomycetoma) transmitted through skin trauma in tropical areas.
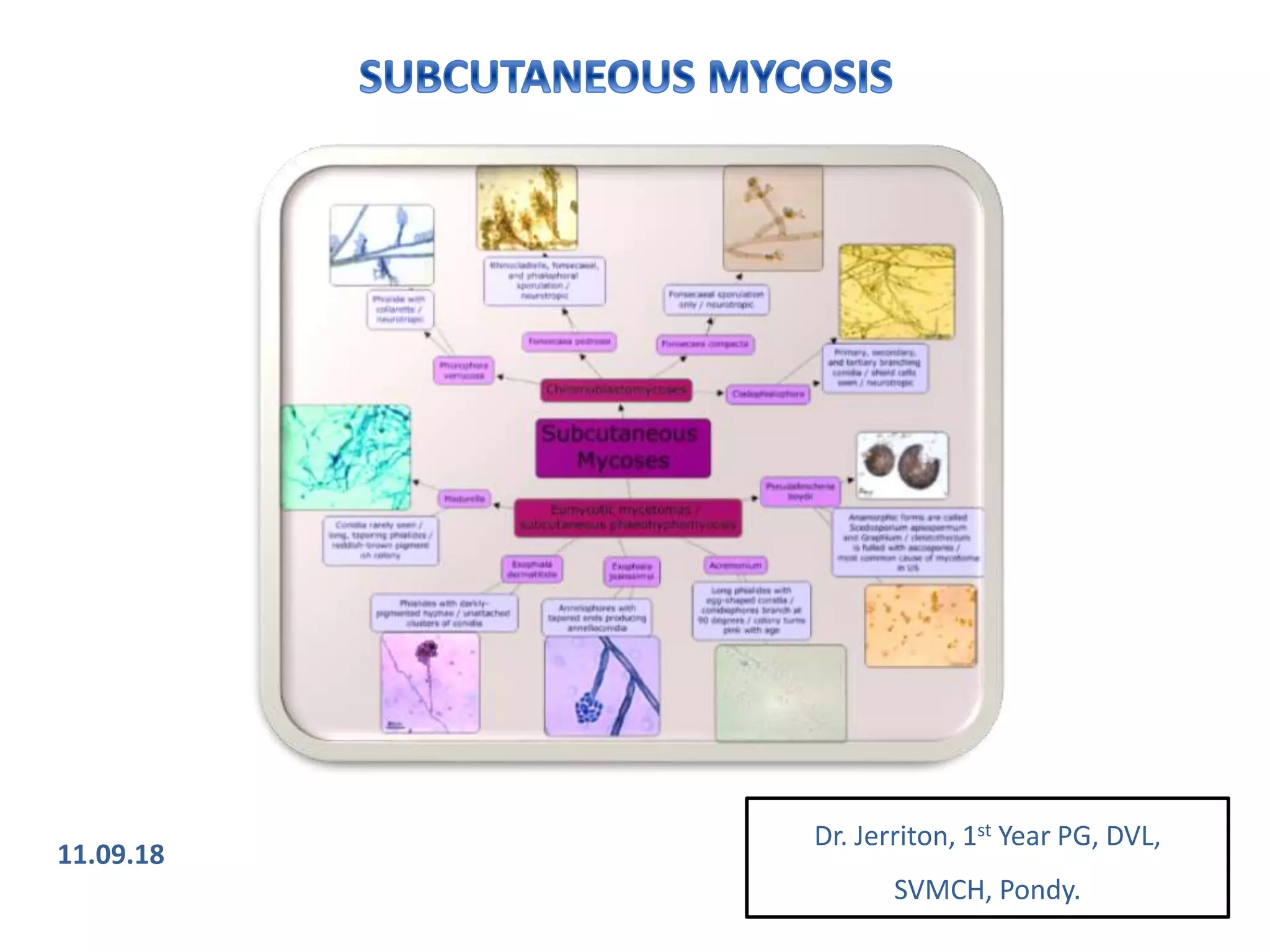
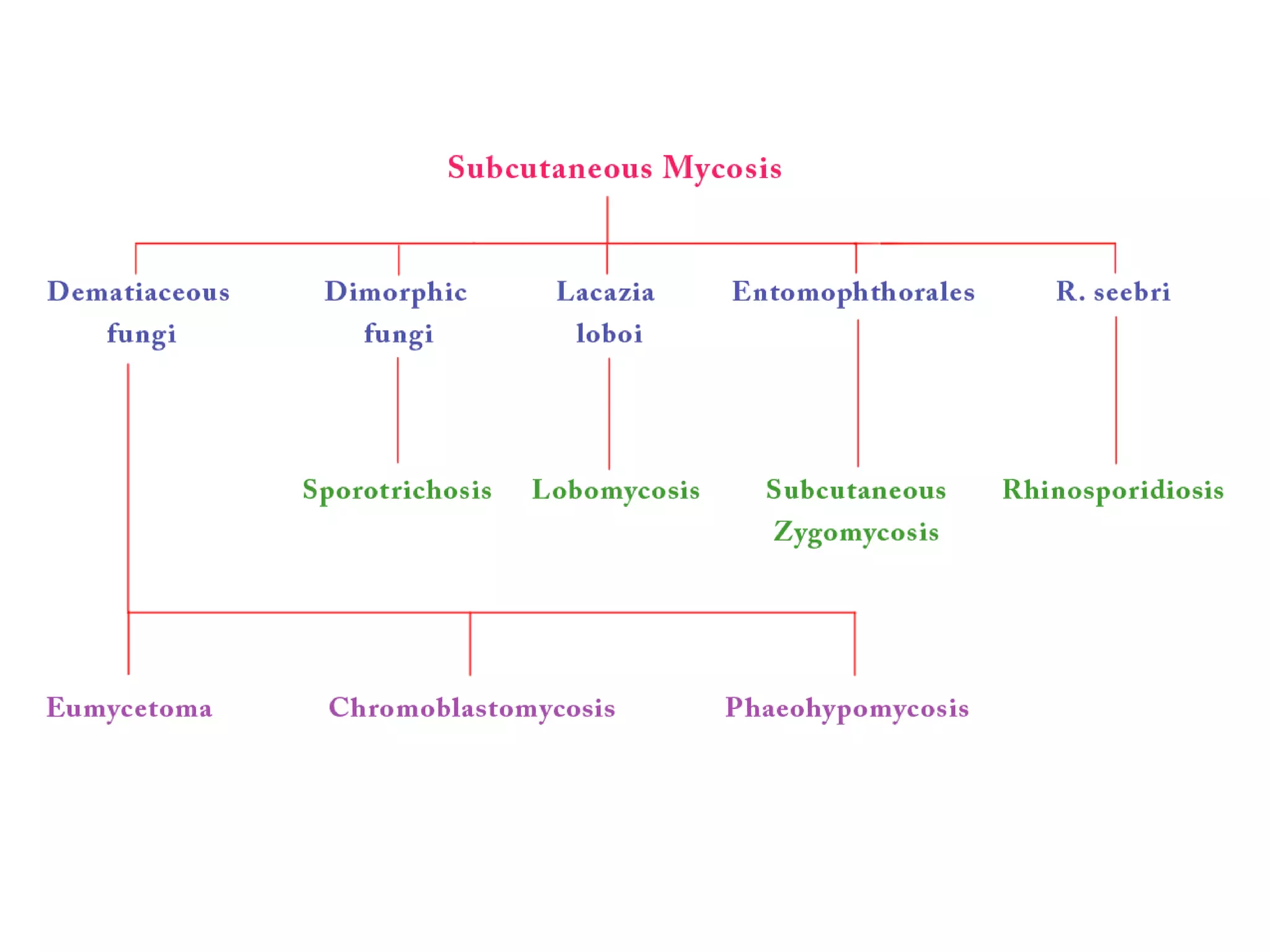
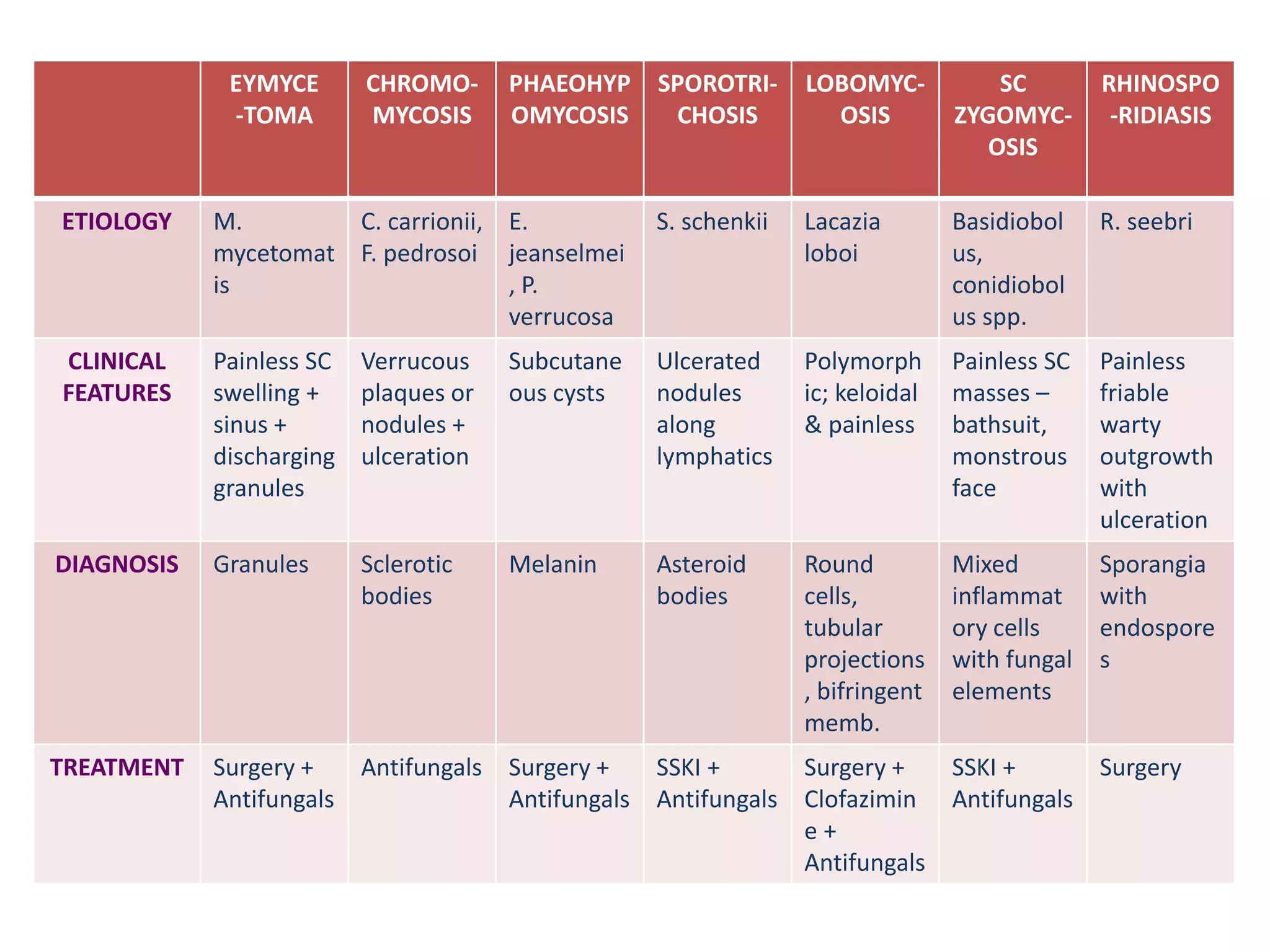
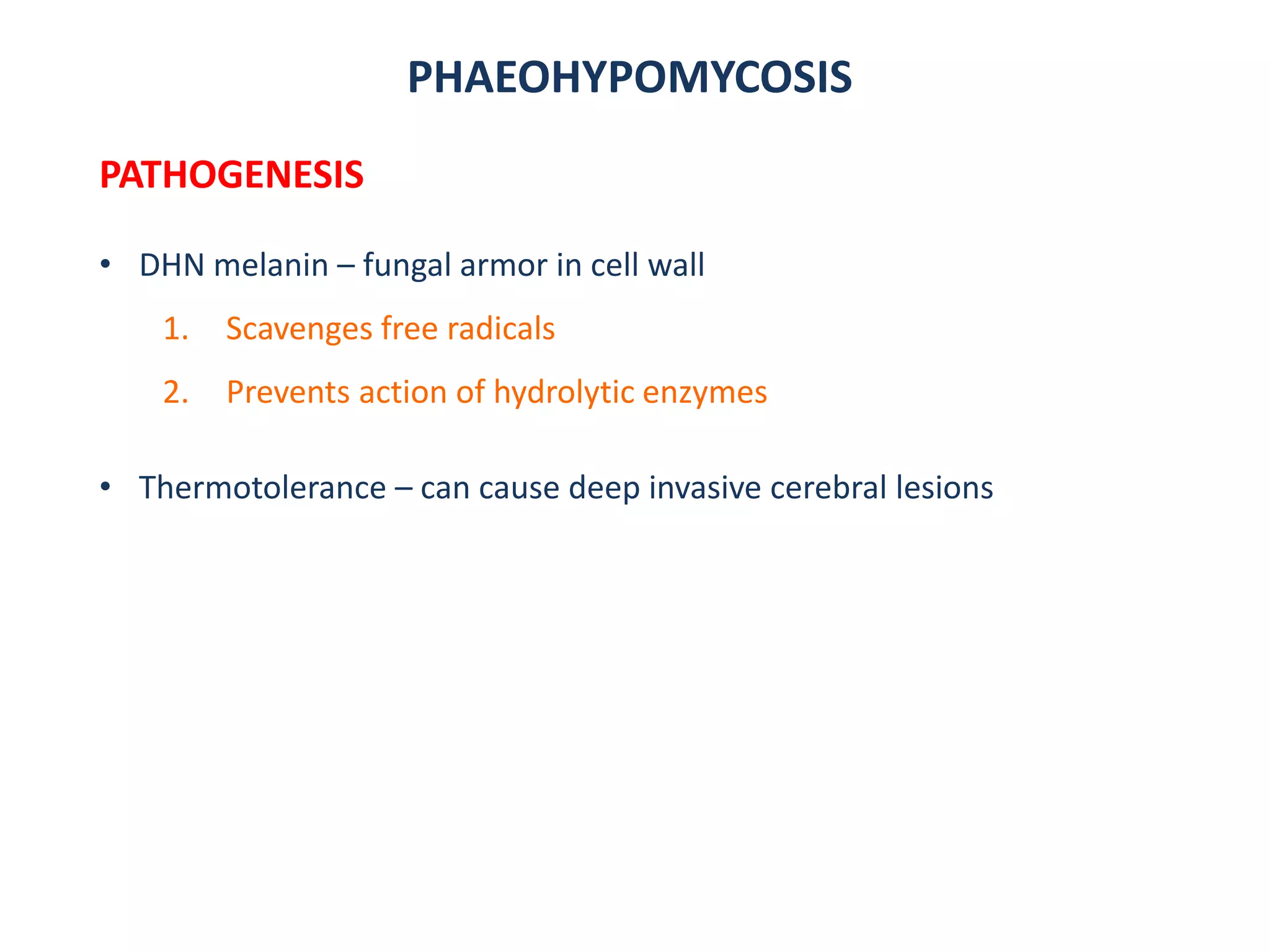
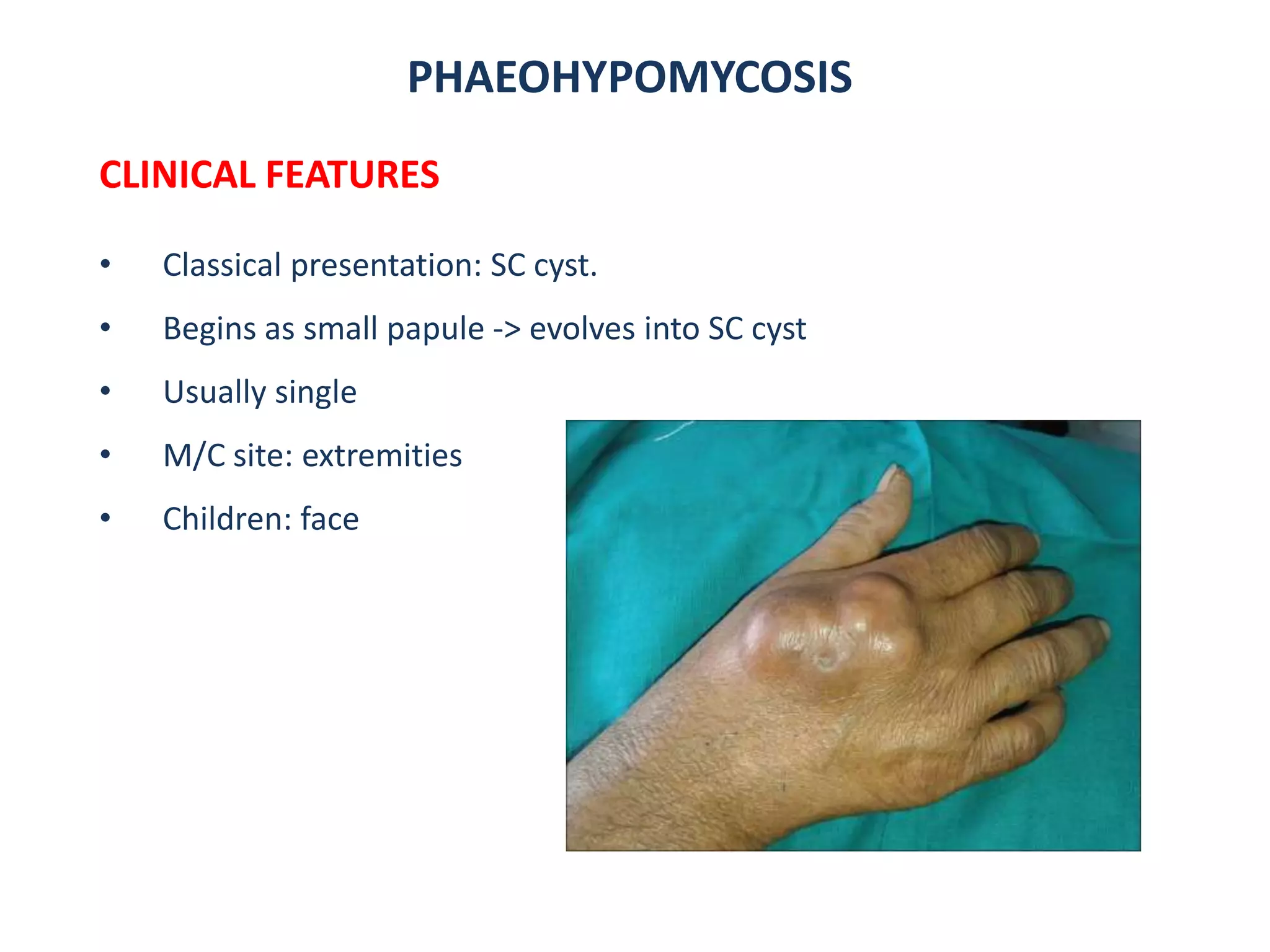
2. Chromoblastomycosis presents as verrucous plaques or nodules that may ulcerate, caused by dematiaceous fungi transmitted through skin abrasions in tropical regions. Phaeohypomycosis is a related fungal infection characterized by subcutaneous cysts.
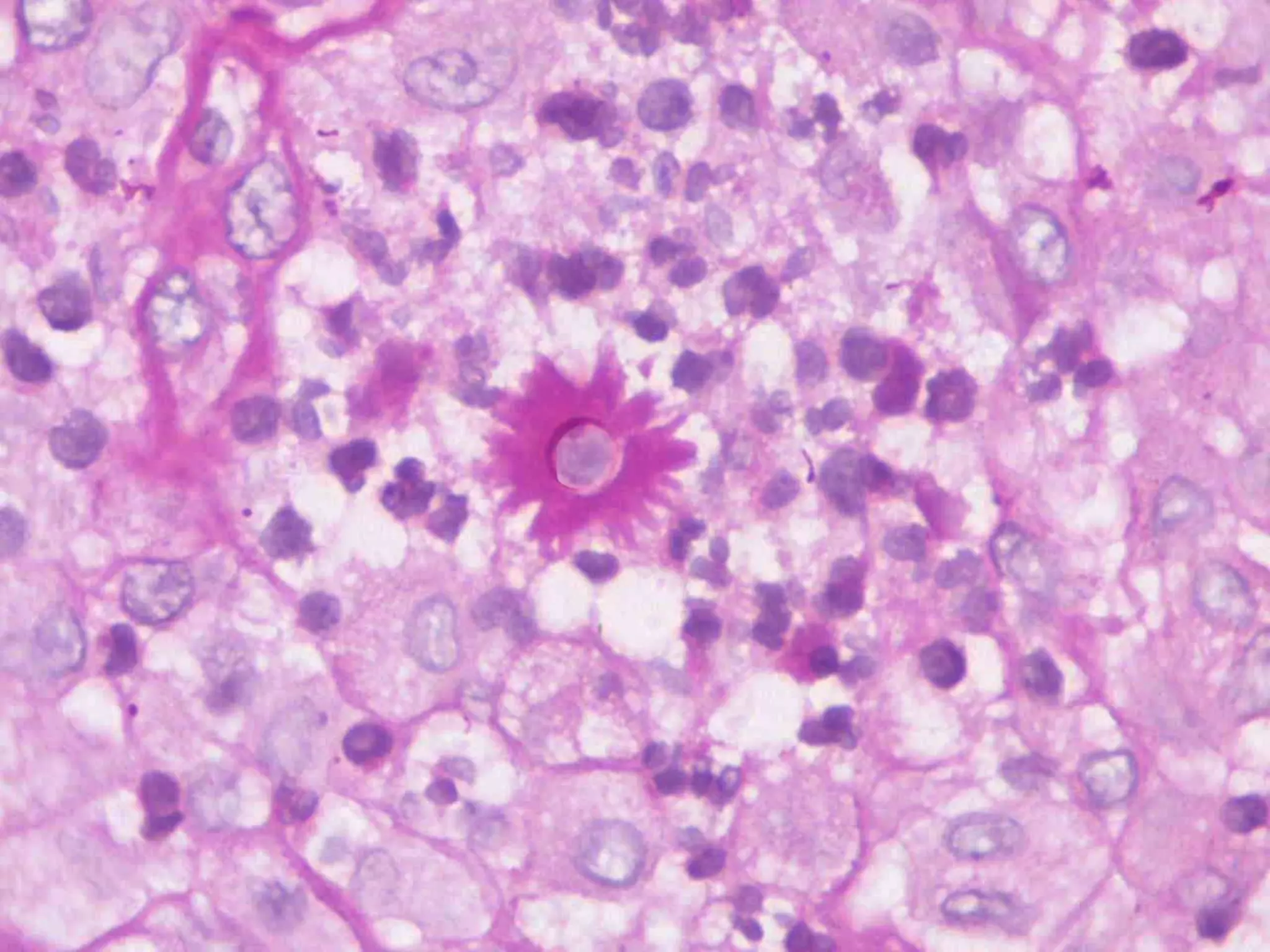
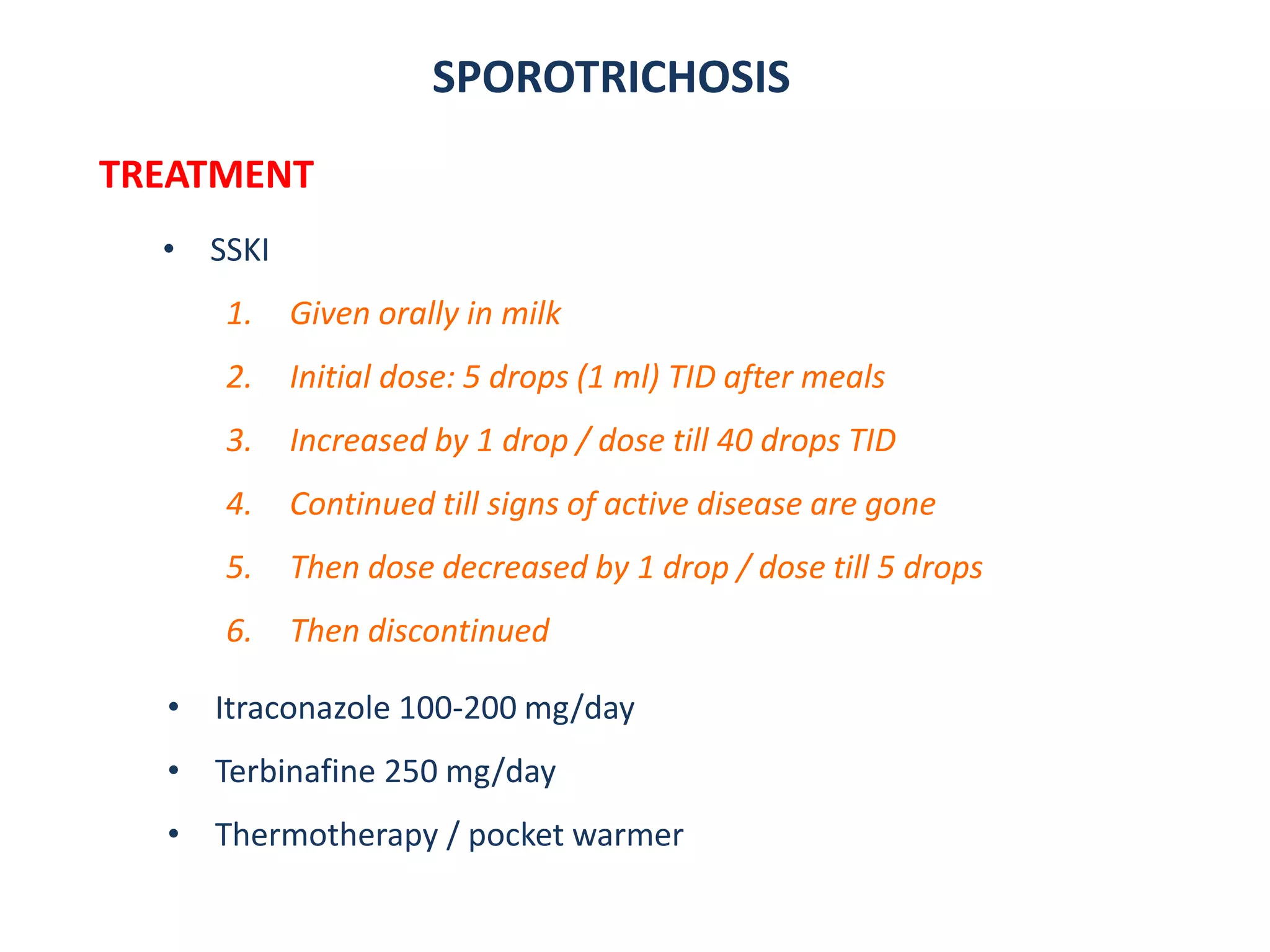
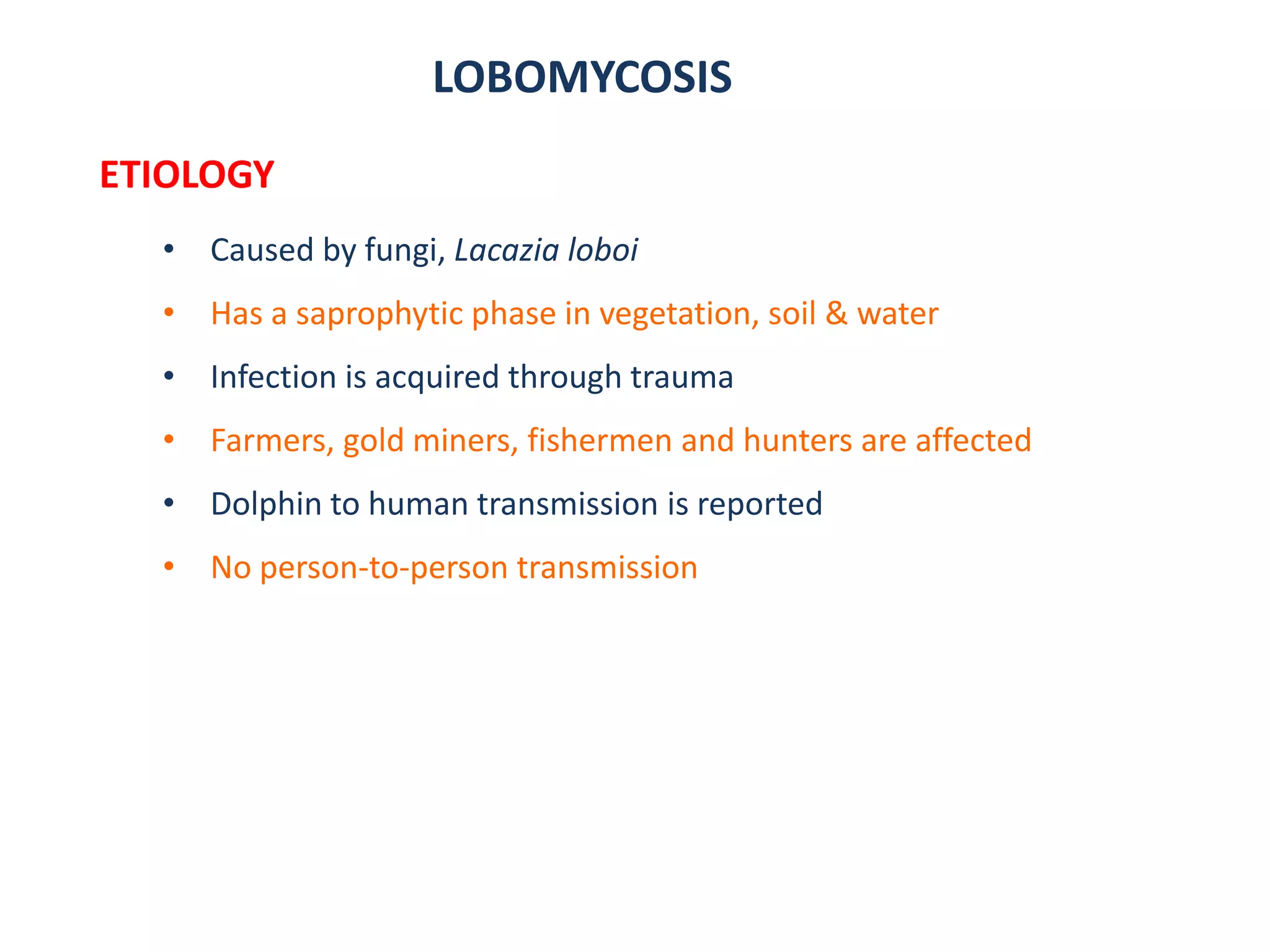
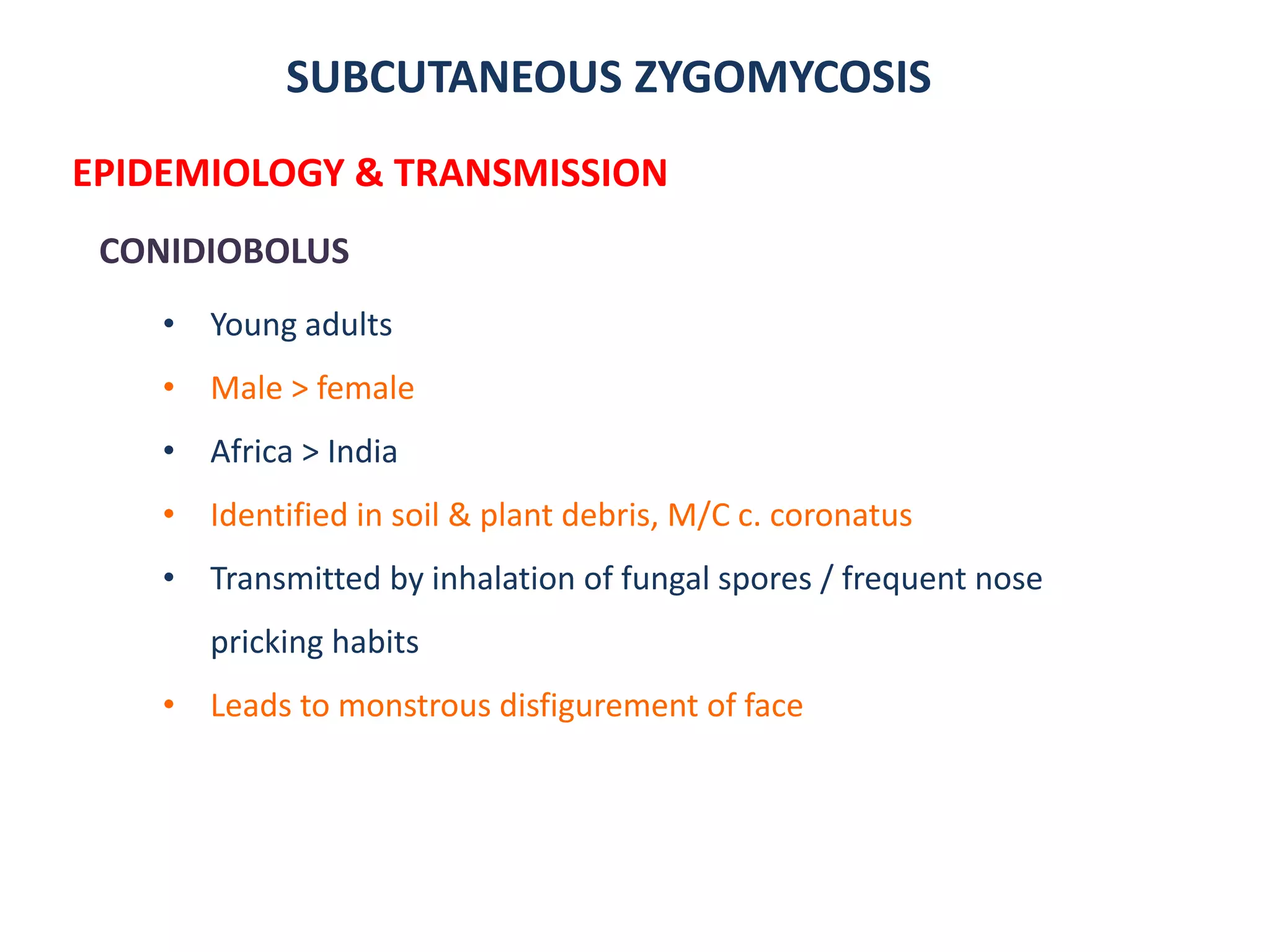
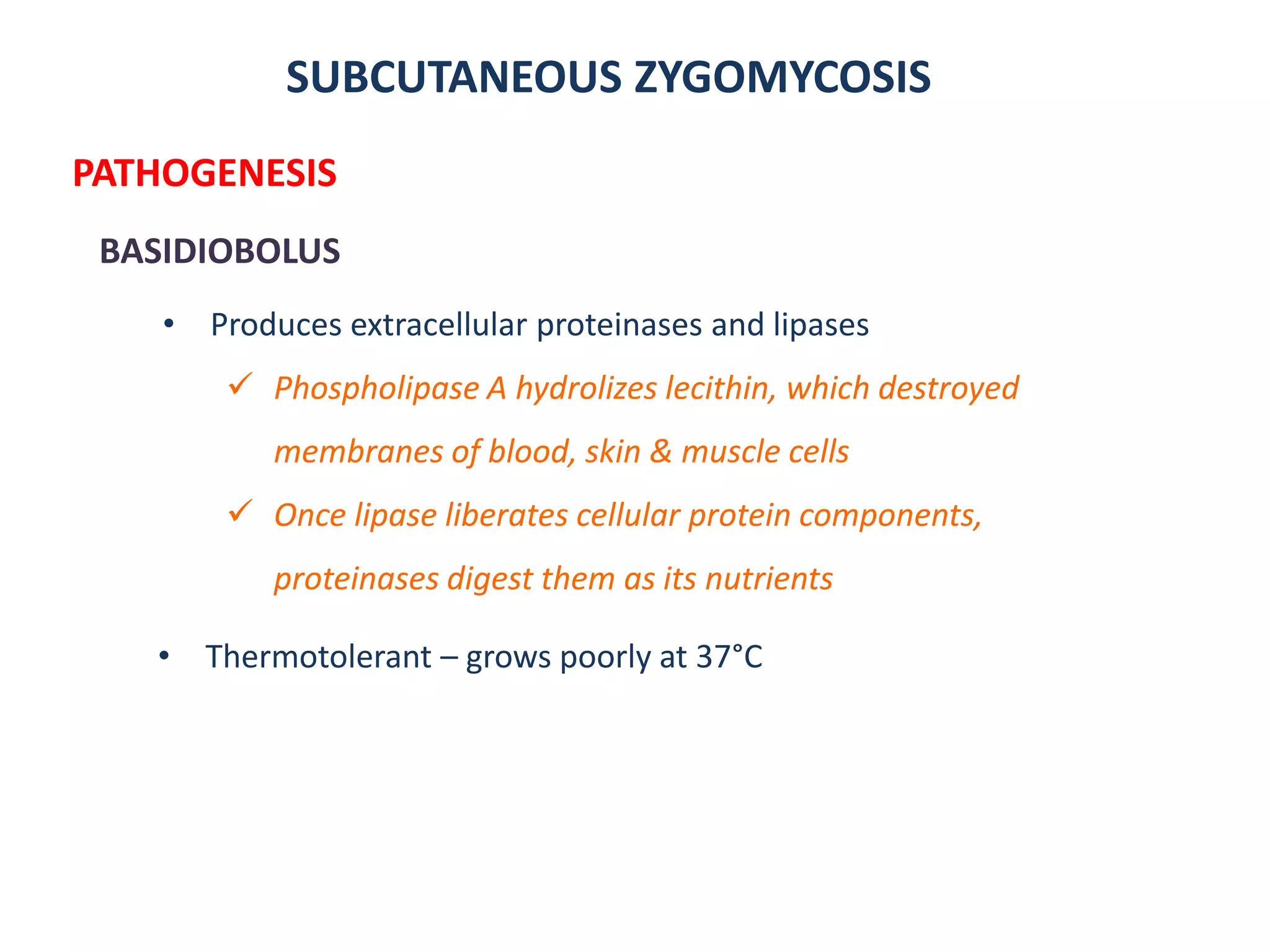
3. Other fungal infections described include sporotrichosis causing ulcerative nodules along lymphatics, lobomy