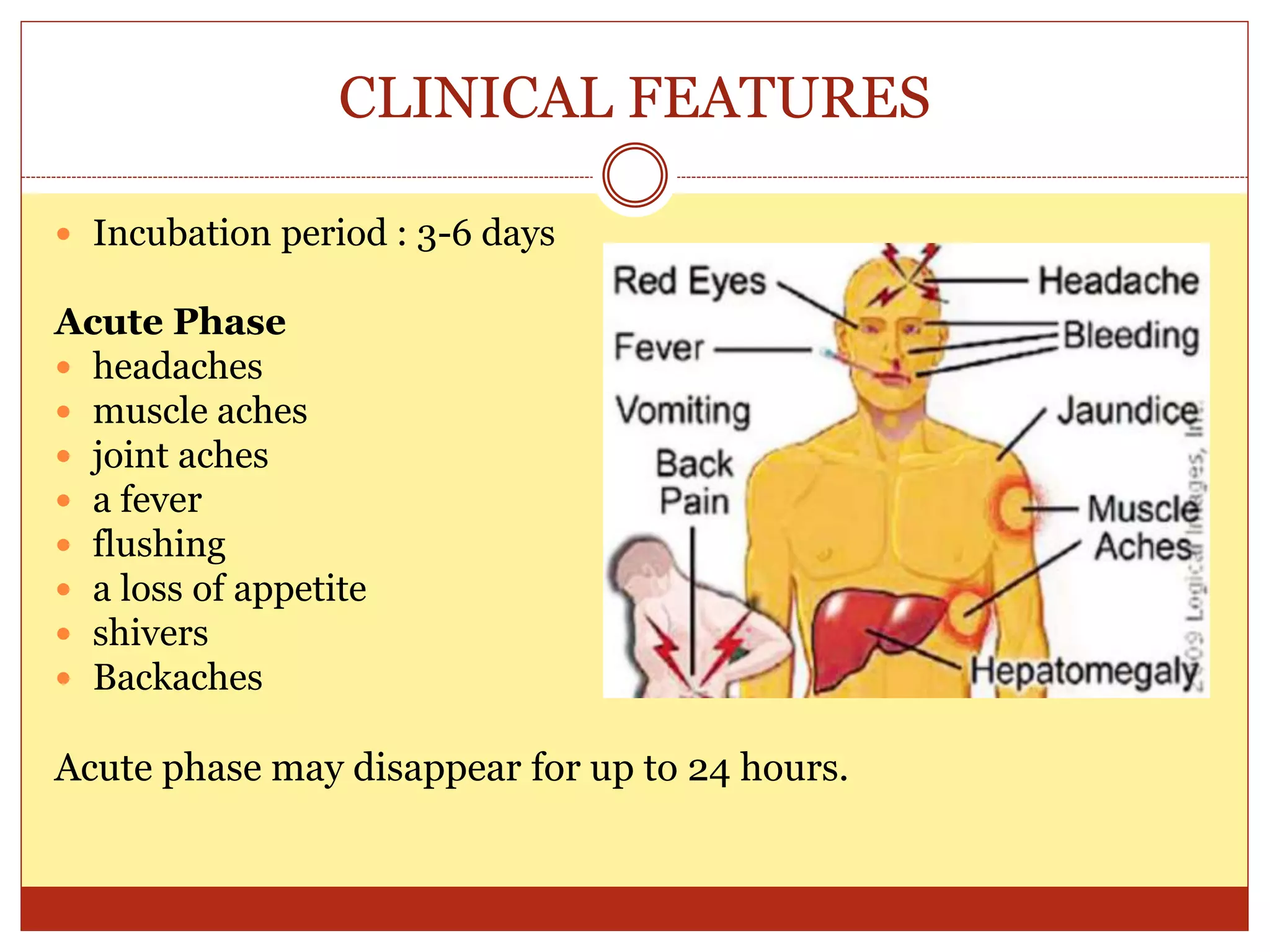
This document defines yellow fever, discusses its transmission via infected mosquitoes, and outlines its epidemiology, clinical features, diagnosis, treatment, and control. Yellow fever is an acute viral disease transmitted by Aedes and Haemogogus mosquitoes that causes jaundice and can be fatal. It is diagnosed through blood tests and treated symptomatically with rest and fever relief. Vaccination and mosquito control are important for prevention.