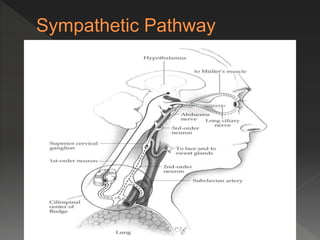
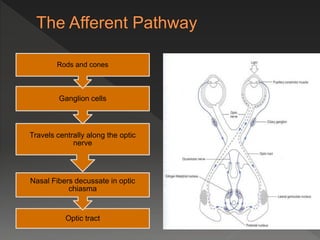
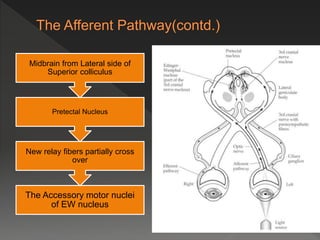
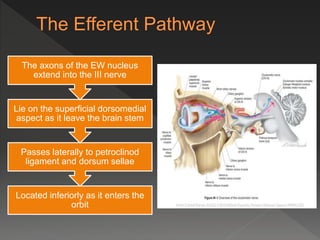
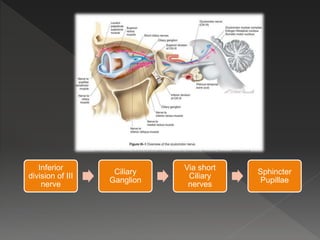
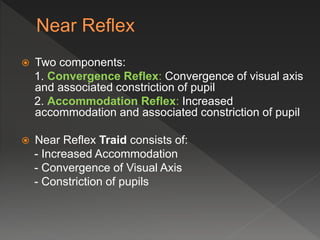
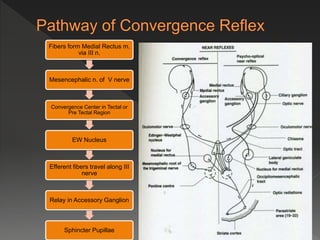
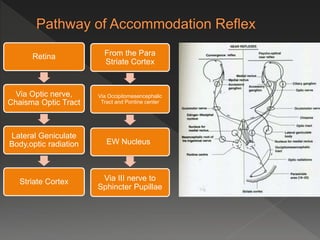
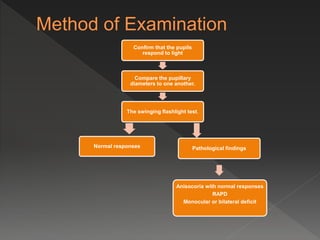
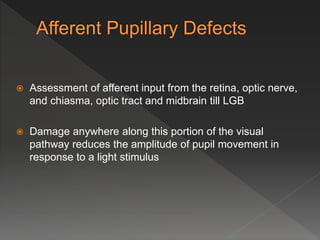
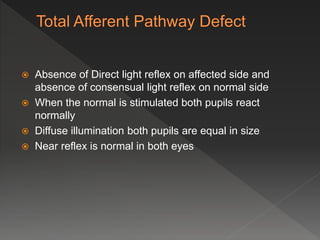
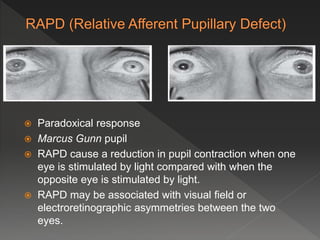
The document describes the anatomy and physiology of the pupillary light reflex pathway. It discusses the iris, pupil size and shape, functions of the iris such as light control and depth of focus. It then covers clinical uses such as assessing light input and pharmacological response. The document outlines the afferent and efferent pathways in detail from the retina to the Edinger-Westphal nucleus. It discusses various clinical tests and findings including anisocoria and causes.

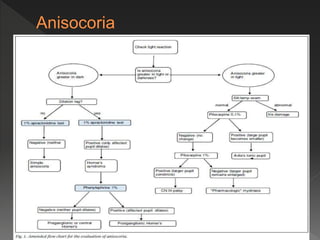
![ If the Larger pupil is abnormal (poor constriction), the
anisocoria is greatest in Bright illumination, as the
normal pupil becomes small
This is caused from the disruption of the
Parasympathetic (efferent) pupillary pathway [BPL]
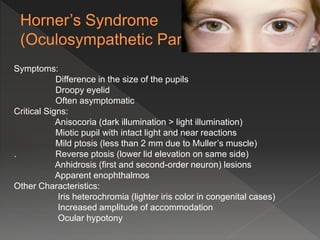
If the Smaller pupil is abnormal (poor dilation), the
anisocoria is greatest in Dark illumination, as the normal
pupil becomes large
It is caused from the disruption of the Sympathetic
pupillary pathway](https://image.slidesharecdn.com/pupilmajferdous-copy-161022131903/85/Pupil-dr-ferdous-24-320.jpg)