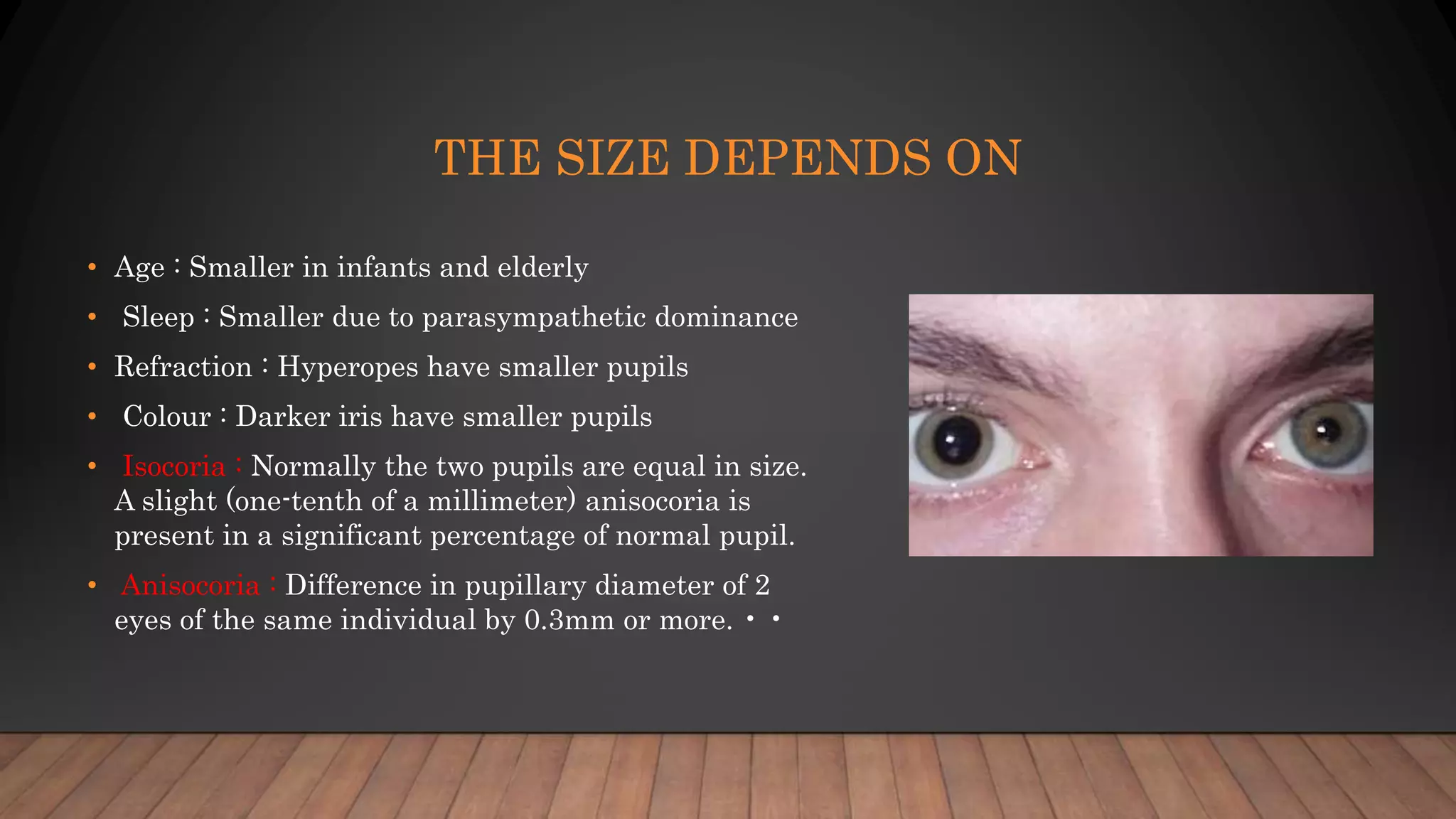
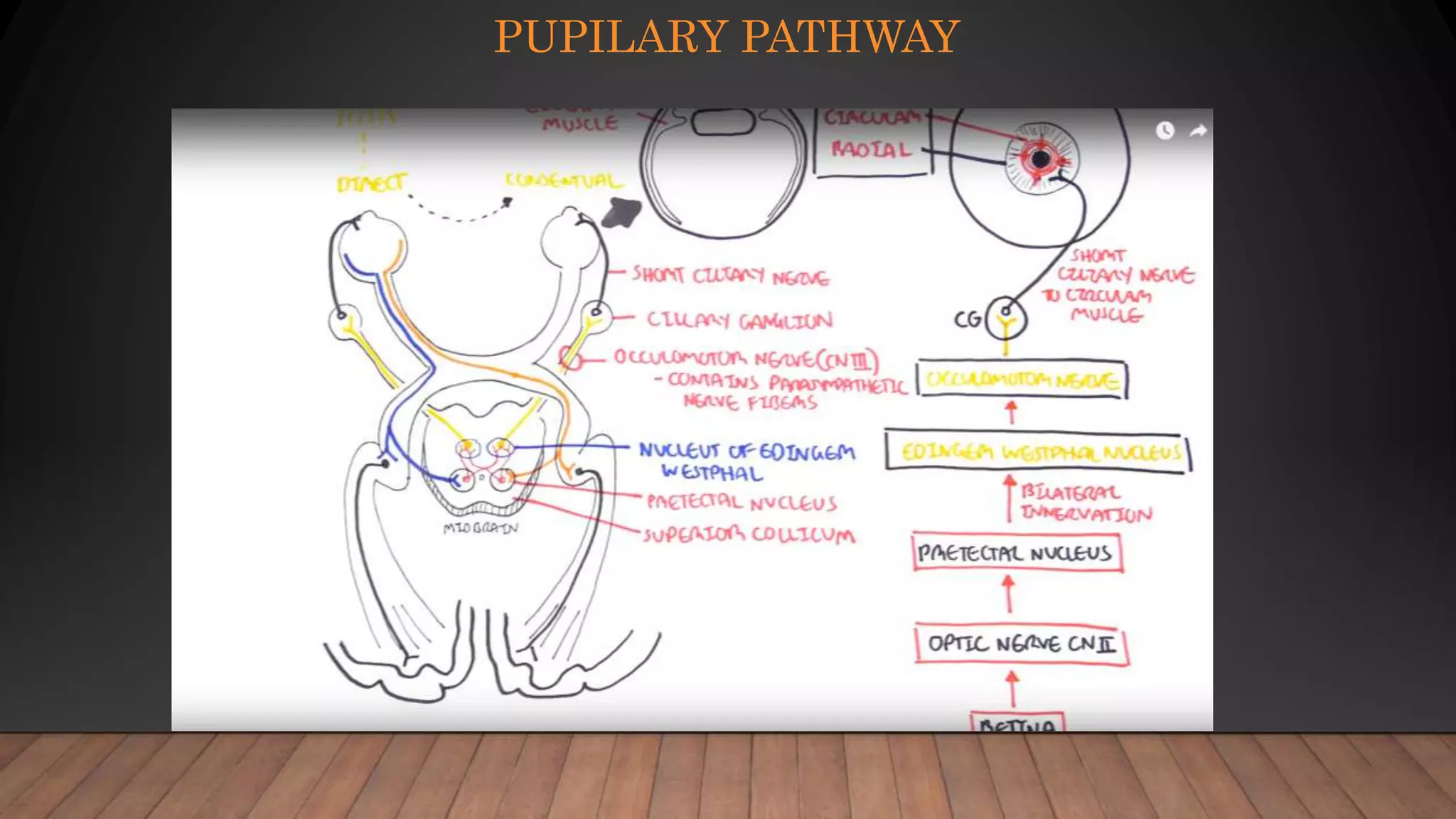
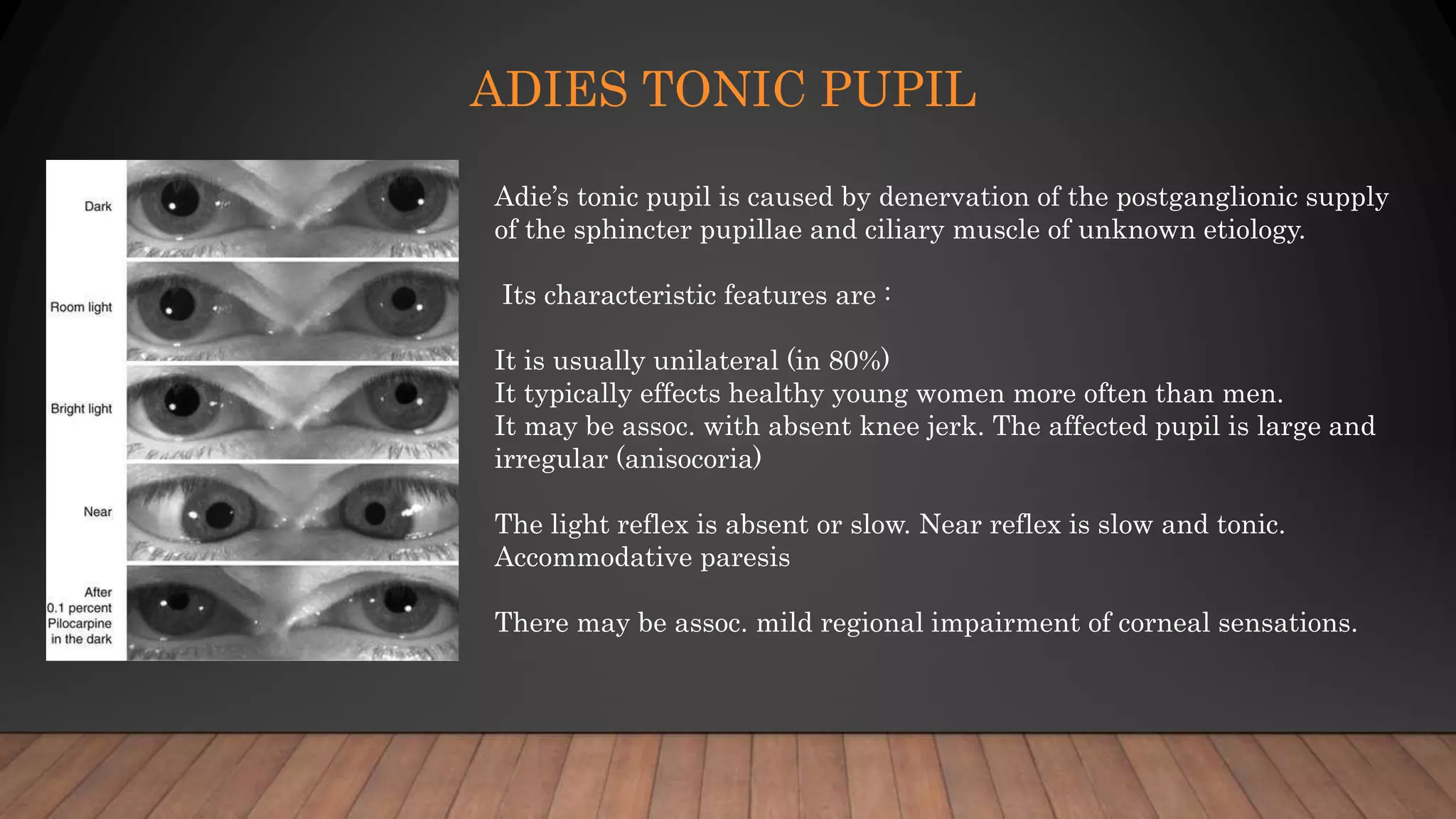
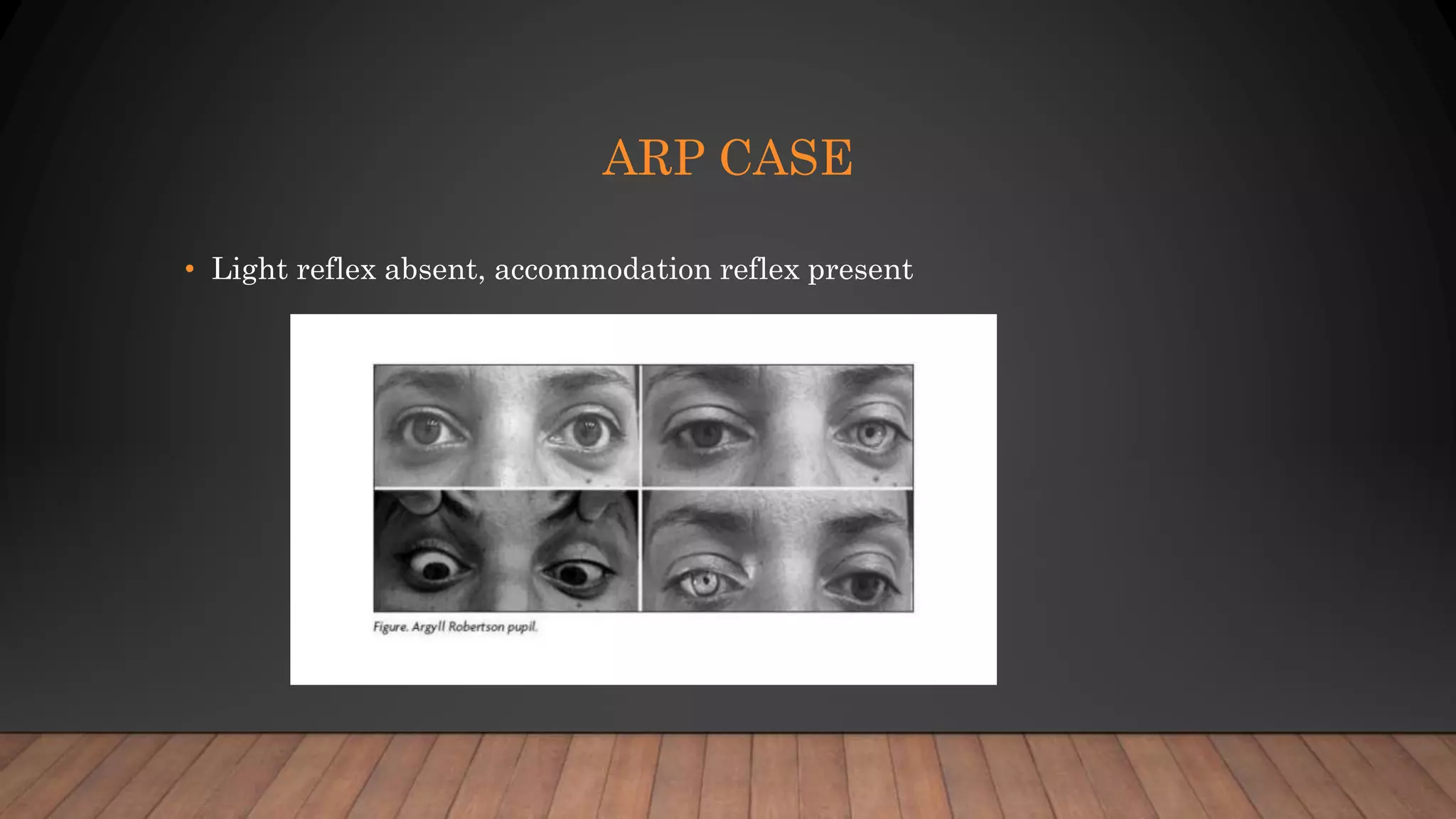
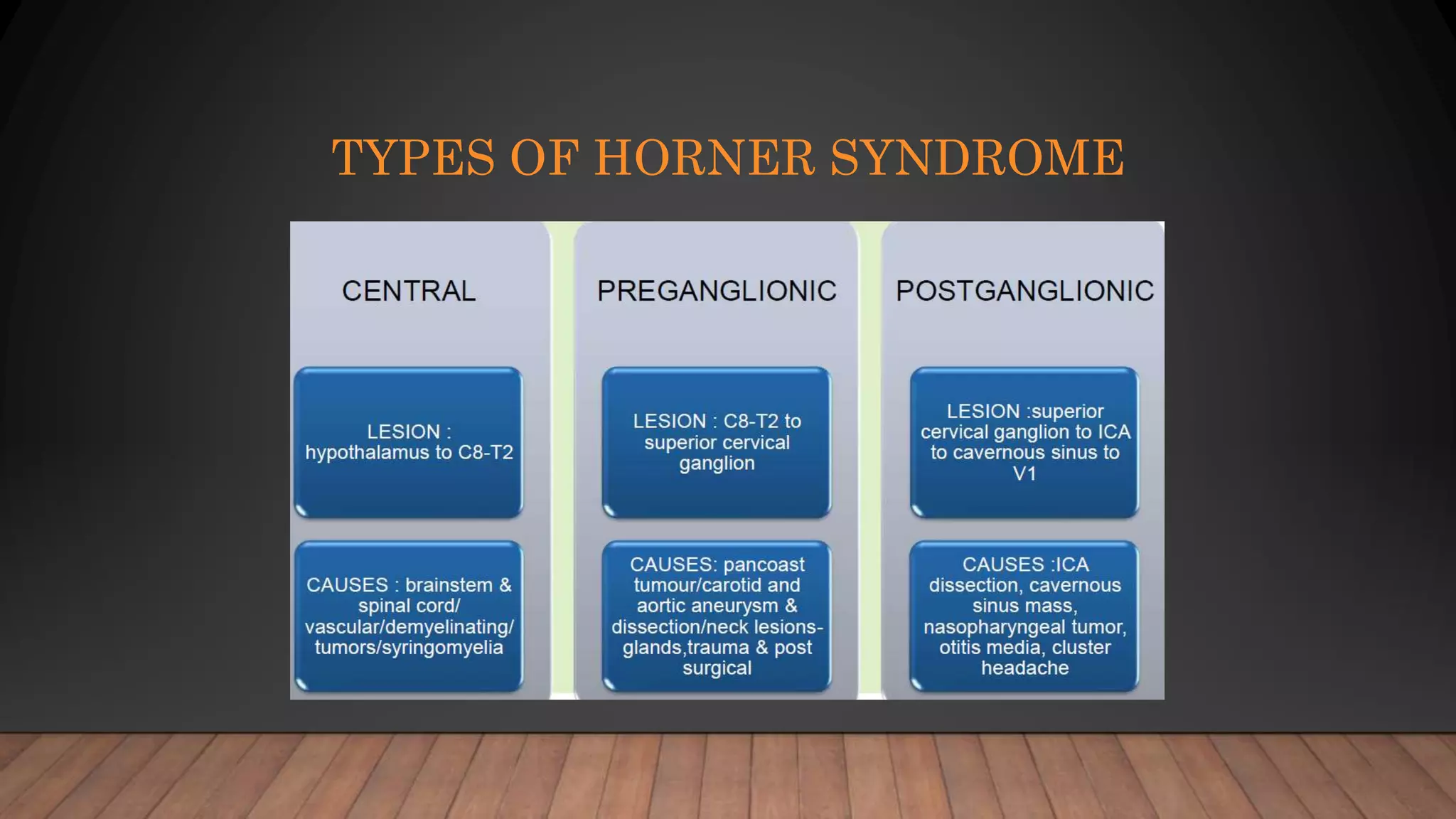
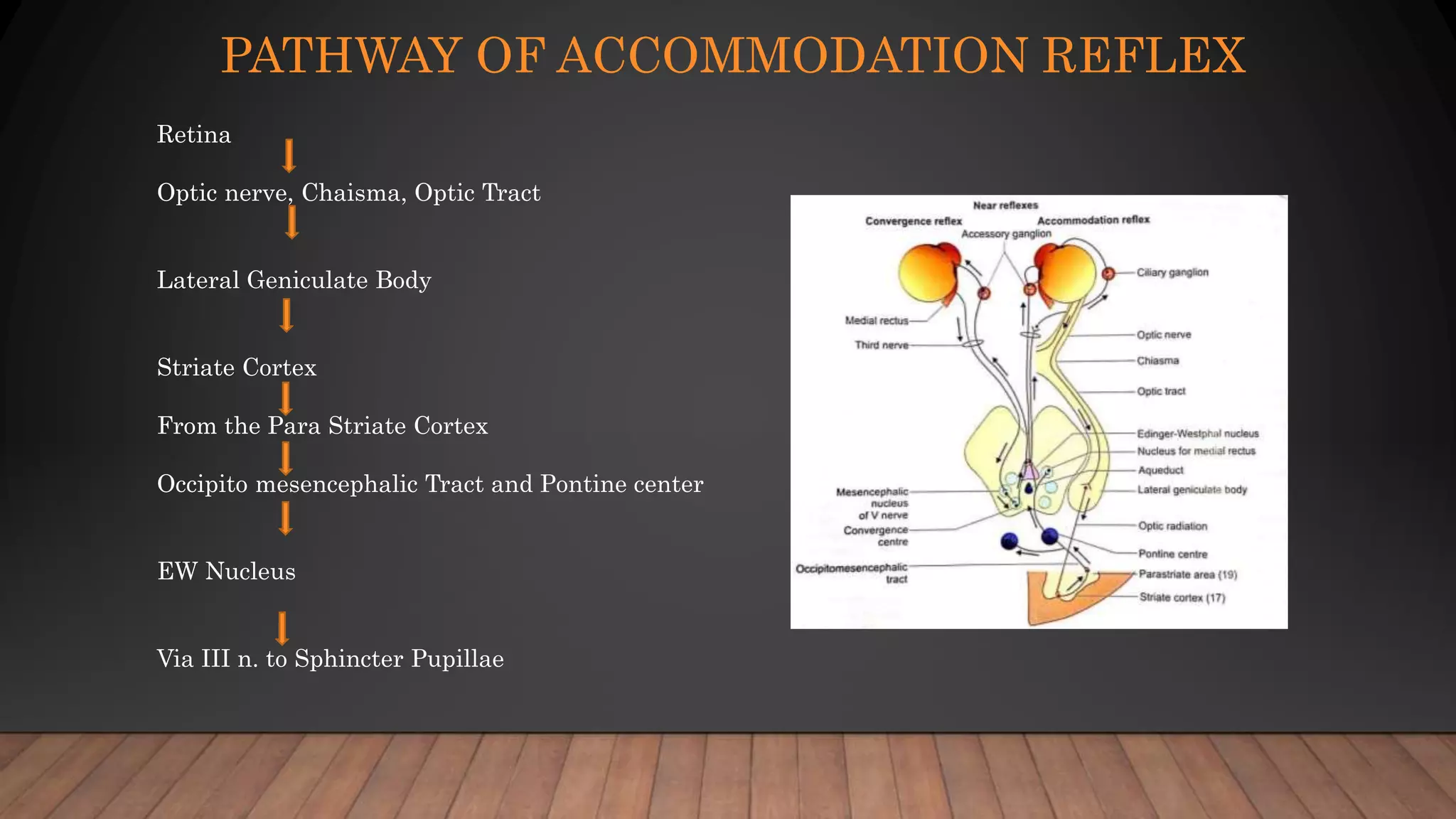
The document discusses the anatomy and physiology of the pupil, including its reflex pathways and disorders. It explains the normal size variations of the pupil, the light reflex mechanism, and various types of pupillary defects such as efferent defects and tonic pupils. The document also details conditions like Horner's syndrome and Argyll Robertson pupil, outlining their clinical features and underlying causes.