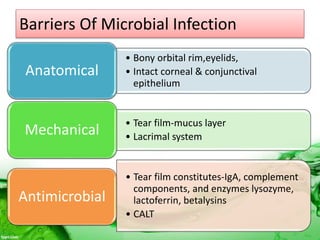
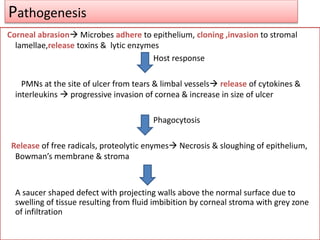
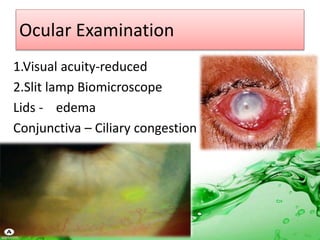
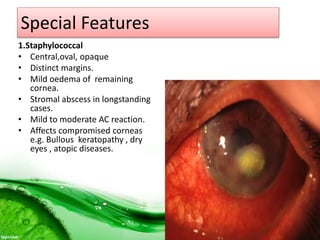
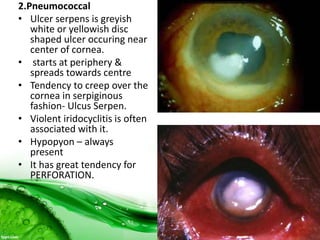
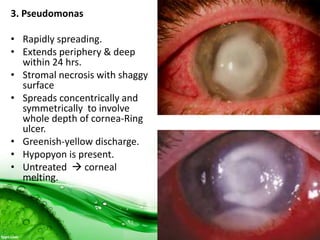
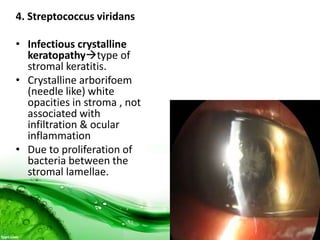
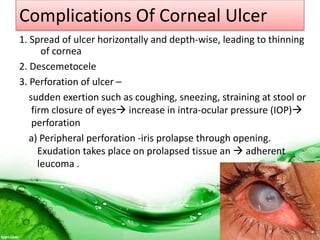
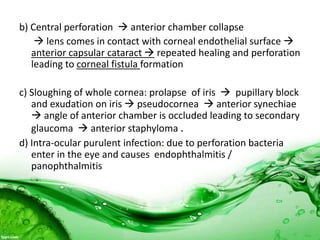
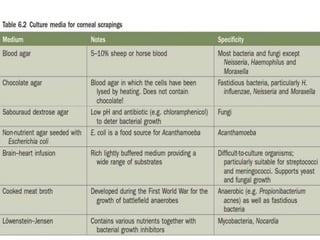
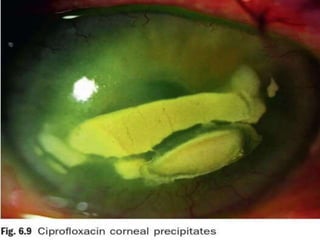
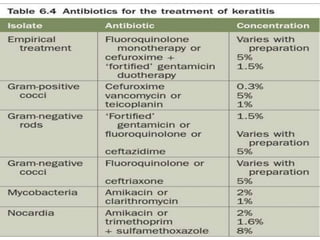
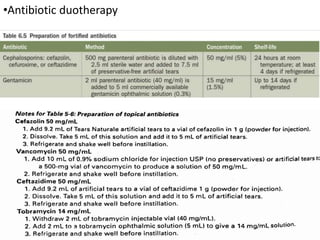
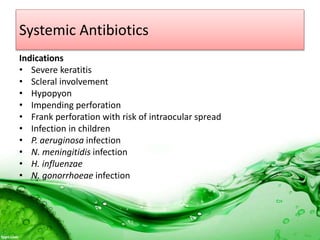
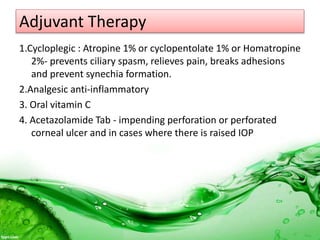
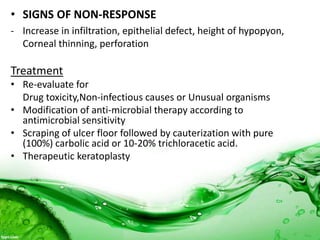
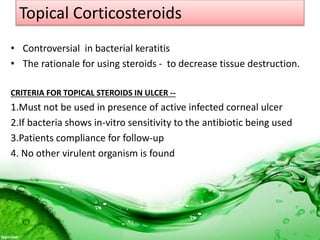
Bacterial keratitis is a sight-threatening condition that develops when the eye's defenses are compromised. It is caused by bacteria such as Pseudomonas, Staphylococcus, and Streptococcus invading the cornea. Risk factors include trauma, ocular surface diseases, contact lens wear, and immunosuppression. Treatment involves local and systemic antibiotics based on smear and culture results, along with cycloplegics and analgesics. For impending perforation, measures to lower pressure and tissue adhesives may be used. Surgery is needed for large perforations or non-healing ulcers.