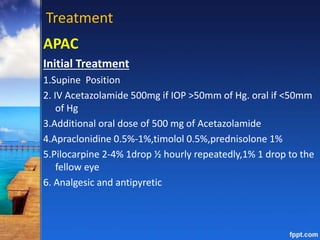
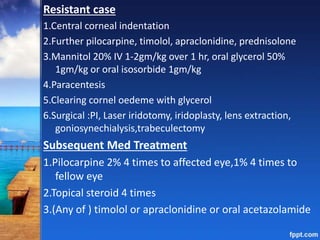
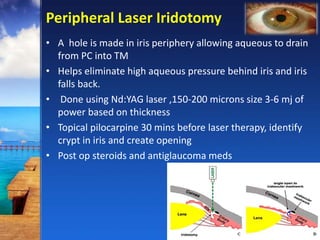
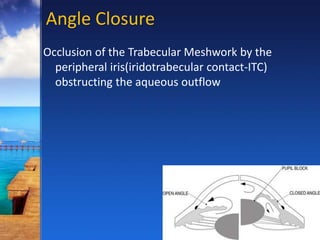
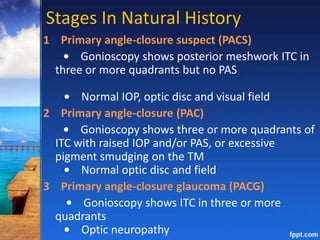
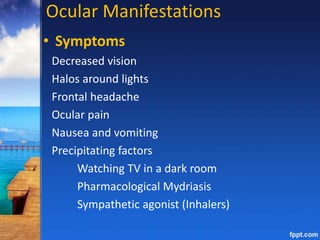
This document discusses primary angle closure glaucoma (PACG). It begins by describing the stages of PACG from primary angle closure suspect to primary angle closure glaucoma. It then covers risk factors, mechanisms (including pupillary block and non-pupillary block), signs and symptoms, investigations, and treatment approaches including laser iridotomy, medications, and surgery. The treatment goal is to eliminate iris blockage and lower elevated intraocular pressure to prevent optic nerve damage.

![Mechanism
Relative Pupillary Block
• Failure of aqueous flow through the mid dilated
pupil leads to a pressure differential between the
anterior and posterior chambers, with resultant
anterior bowing of the lax iris [Iris bombe] blocks
trabecular meshwork and iridolenticular contact](https://image.slidesharecdn.com/pacg-161105155039/85/Primary-Angle-Closure-Glaucoma-Dr-Ferdous-5-320.jpg)
![Signs
APAC
Elevated IOP risen rapidly
Conjunctival congestion
Corneal epithelial /stromal edema
Shallow or flat peripheral AC
Mid dilated [vertical oval] pupil
Absent /sluggish pupil reaction
Fellow eye generally shows an occludable angle
Subacute Angle Closure](https://image.slidesharecdn.com/pacg-161105155039/85/Primary-Angle-Closure-Glaucoma-Dr-Ferdous-10-320.jpg)
![Resolved APAC
• Folds in Descemet membrane (if IOP has been
reduced rapidly), optic nerve head congestion and
choroidal folds.
• Later iris atrophy [spiral-like configuration],
irregular pupil, posterior synechiae and
glaukomflecken
• Iris torsion](https://image.slidesharecdn.com/pacg-161105155039/85/Primary-Angle-Closure-Glaucoma-Dr-Ferdous-11-320.jpg)
![Chronic Presentation
• ‘Creeping’ angle-closure [gradual band-like anterior
advance of the apparent insertion of the iris].
From deepest part of the angle and spreads
circumferentially
• Episodic (intermittent) ITC is associated with the
formation of discrete PAS, individual lesions having
a pyramidal (‘saw-tooth’) appearance
• Disc cupping /nerve fibre defects with or without
visual field defect](https://image.slidesharecdn.com/pacg-161105155039/85/Primary-Angle-Closure-Glaucoma-Dr-Ferdous-12-320.jpg)

![Investigations
1. Anterior segment OCT
2. Anterior chamber depth measurement
3. Posterior segment USG
4. Provocative tests
Pharmacological test
pupillary block mechanism in mid dilated state ,increased
tension of iris .
Performed with short acting mydriatic [phenylephrine eye
drops]
if test proves positive –acute attack may be triggered](https://image.slidesharecdn.com/pacg-161105155039/85/Primary-Angle-Closure-Glaucoma-Dr-Ferdous-14-320.jpg)