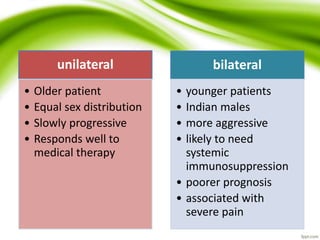
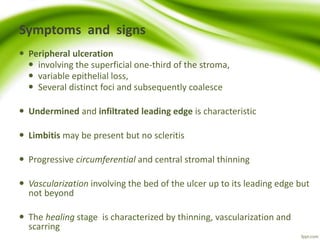
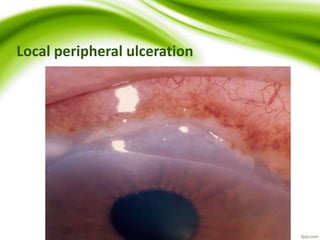
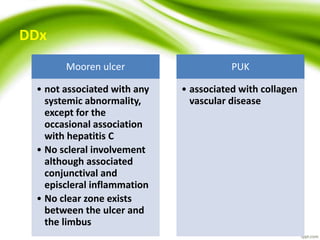
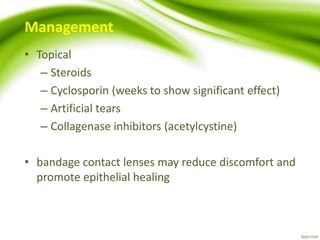
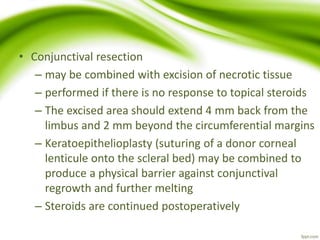
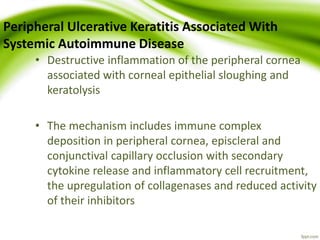
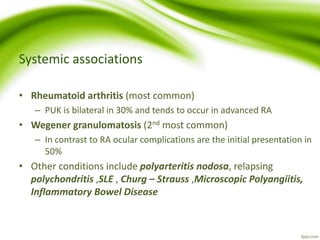
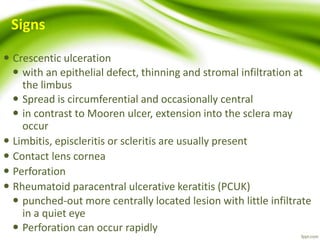
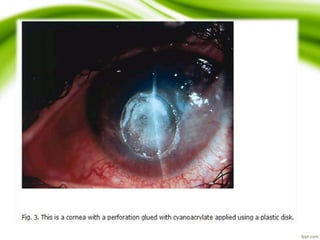
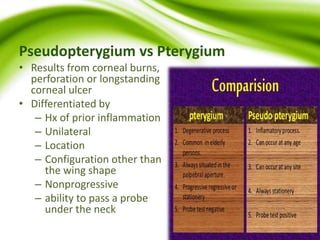
This document discusses peripheral ulcerative keratitis (PUK), a group of inflammatory diseases that cause thinning and ulceration of the peripheral cornea. It describes several types of PUK including Mooren's ulcer, marginal keratitis, Terrien's marginal degeneration, and PUK associated with autoimmune diseases. Mooren's ulcer is a rare autoimmune disease characterized by progressive, peripheral, circumferential ulceration. Marginal keratitis is caused by a hypersensitivity reaction to Staphylococcus exotoxins. Terrien's marginal degeneration causes thinning of the peripheral cornea. PUK associated with autoimmune diseases like rheumatoid arthritis is linked to immune complex deposition in the peripheral cornea. Management involves topical