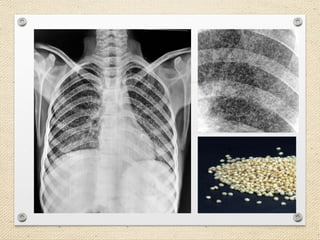
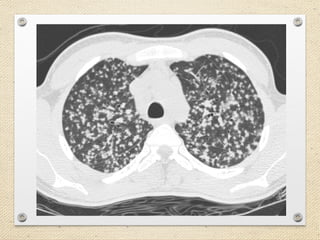
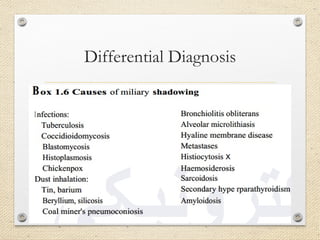
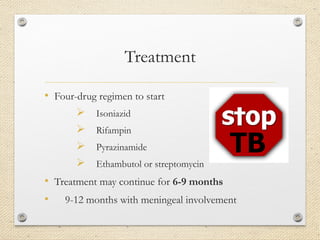
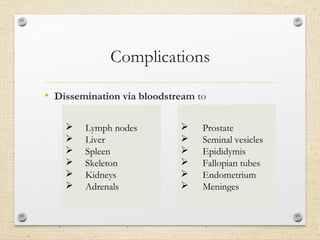
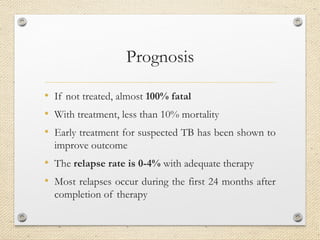
Miliary tuberculosis is a rare form of tuberculosis characterized by the widespread dissemination of tuberculosis bacteria through the bloodstream, forming small nodules throughout the body. It represents 1-3% of tuberculosis cases. Risk factors include age, immunosuppression, cancer, HIV, malnutrition, and diabetes. The bacteria spread from the lungs into the bloodstream and infect multiple organs. Symptoms are nonspecific and include weakness, fever, weight loss, and cough. Diagnosis involves imaging tests to identify the small nodules and laboratory tests such as sputum cultures. Treatment requires a multi-drug regimen for 6-9 months.