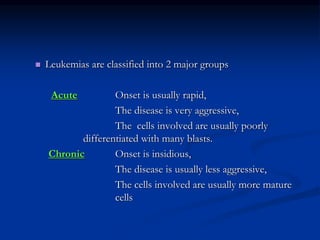
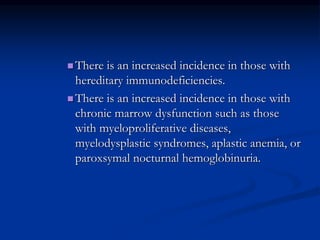
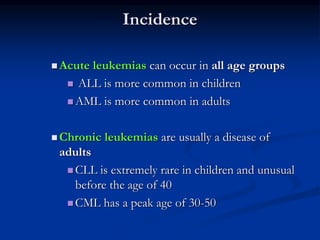
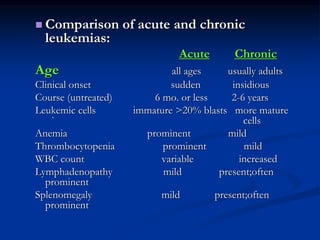
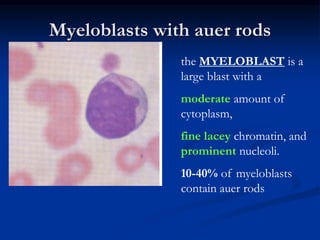
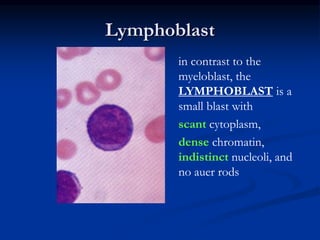
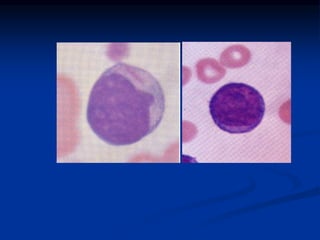
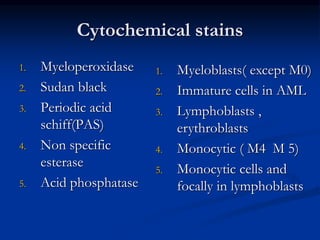
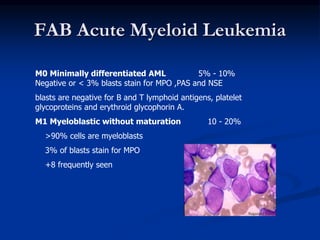
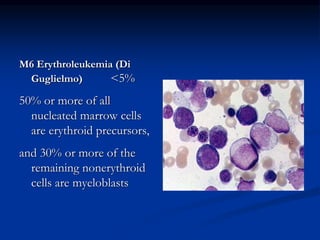
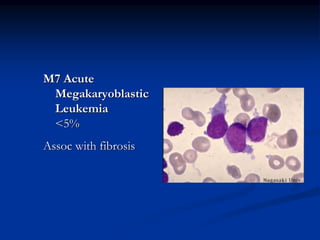
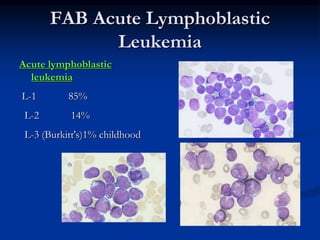
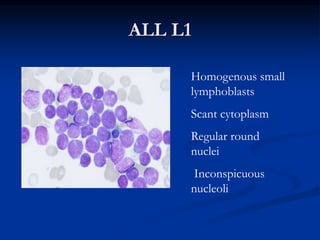
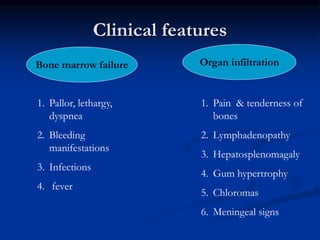
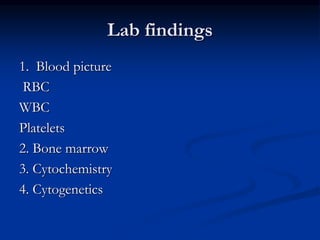
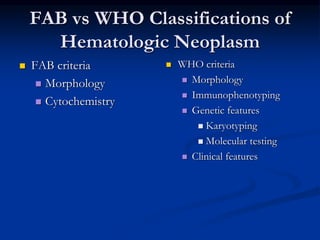
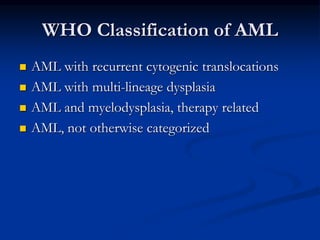
Acute leukemias are cancers of the blood and bone marrow characterized by an overproduction of immature white blood cells. There are two main types: acute myeloid leukemia (AML) involving myeloid cells, and acute lymphoblastic leukemia (ALL) involving lymphoblasts. AML and ALL are classified according to cell morphology, immunophenotyping, genetics, and other lab findings. Common symptoms include fatigue, bleeding, and infections due to low blood cell counts. The document discusses the definitions, types, causes, diagnostic criteria, and clinical manifestations of acute leukemias.