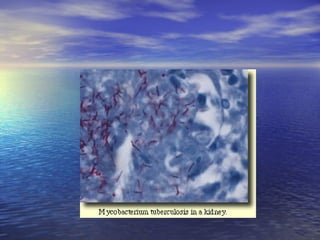
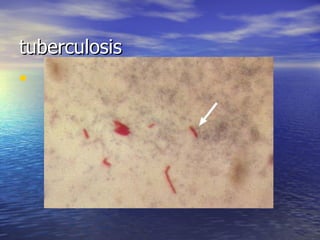
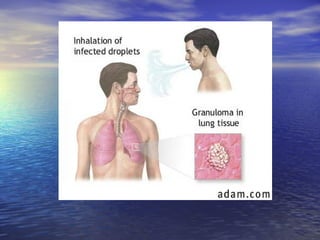
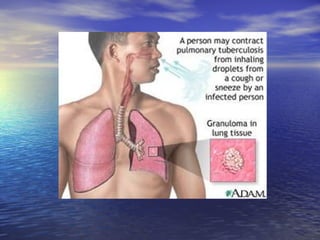
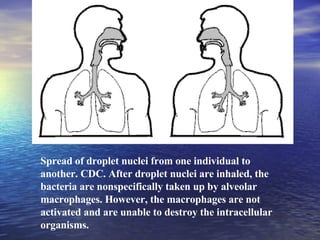
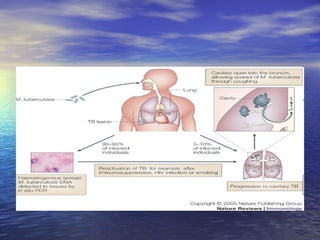
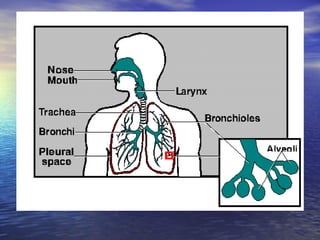
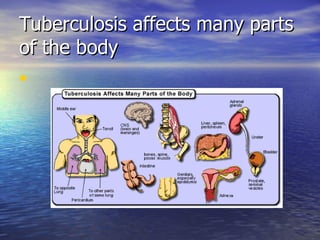
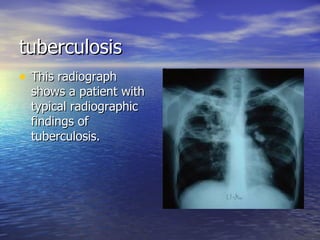
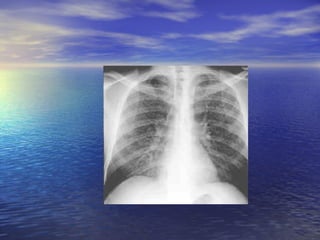
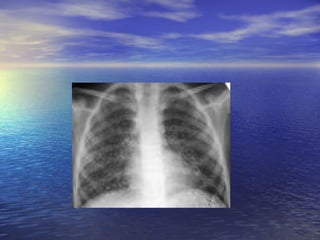
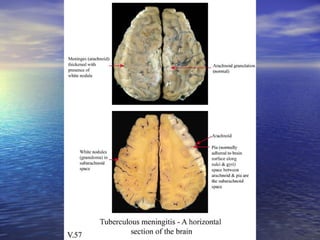
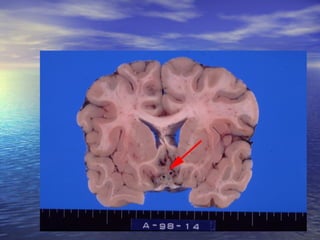
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis. It affects many parts of the body and has a variable clinical presentation ranging from no symptoms to severe symptoms like fever, cough, and weight loss. Diagnosis involves tests like the tuberculin skin test and imaging tests. Treatment requires a long course of multiple anti-tuberculosis medications.