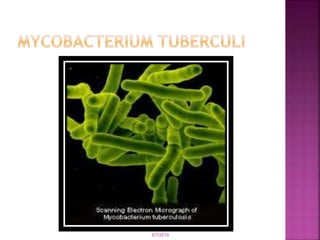
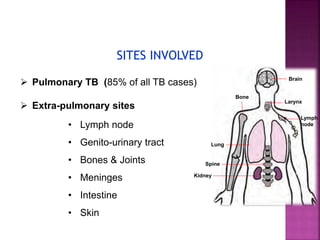
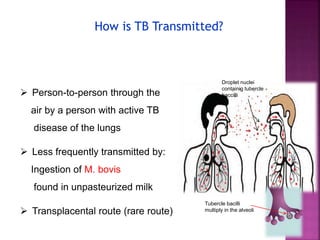
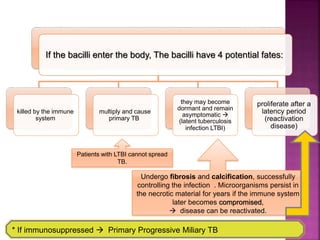
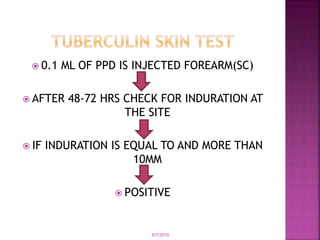
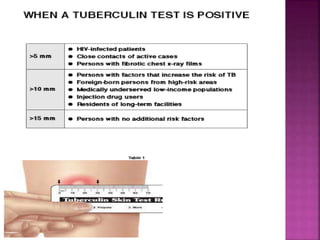
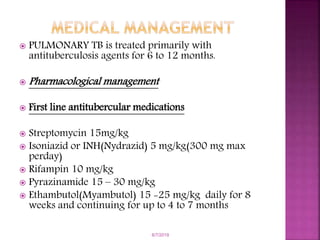
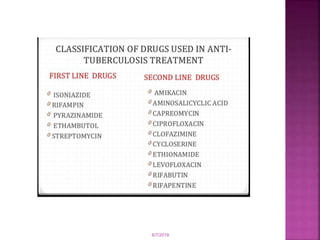
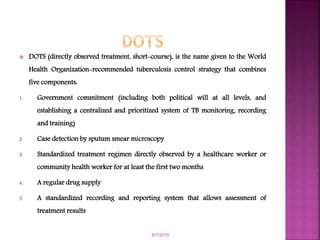
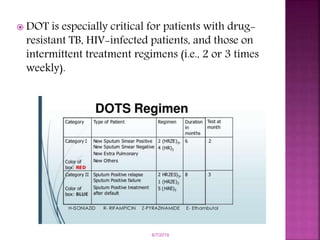
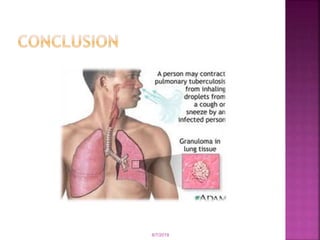
Tuberculosis is an infectious disease caused by the bacterium Mycobacterium tuberculosis, which most commonly affects the lungs. It spreads through inhaling droplets from the coughs or sneezes of an infected individual. Typical symptoms include cough, fever, night sweats and weight loss. Diagnosis involves chest x-rays, sputum smear tests and the tuberculin skin test. Treatment requires taking multiple antibiotics daily for 6-12 months. Strict adherence to treatment is important to cure the infection and prevent drug resistance.