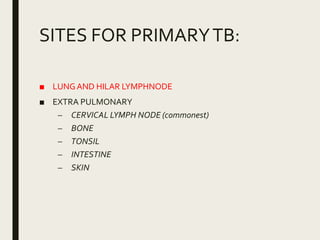
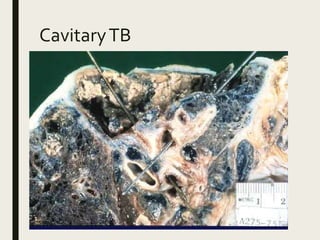
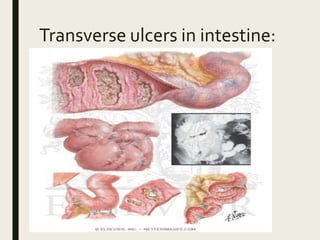
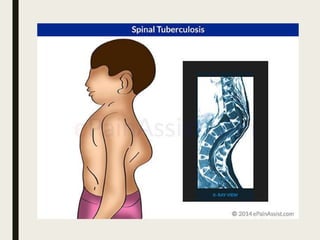
This document discusses tuberculosis (TB), caused by the bacterium Mycobacterium tuberculosis. It spreads through the air and affects the lungs and other organs. Poverty, malnutrition and overcrowding increase the risk. Primary TB occurs via inhaled bacteria forming lesions, while secondary TB results from reactivation of dormant bacteria. Symptoms include cough, fever and weight loss. Diagnosis involves staining samples to identify bacteria and culturing sputum. Treatment requires long-term antibiotic therapy.