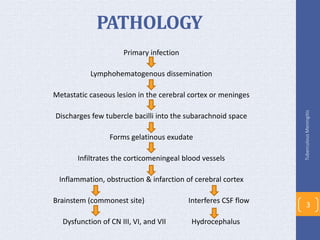
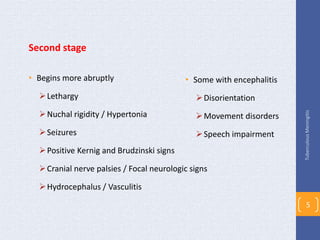
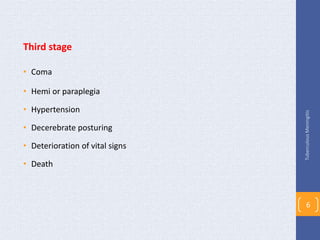
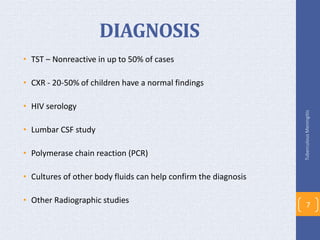
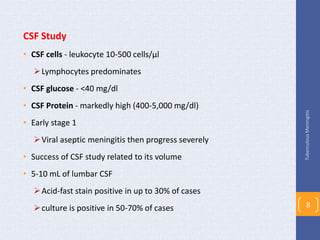
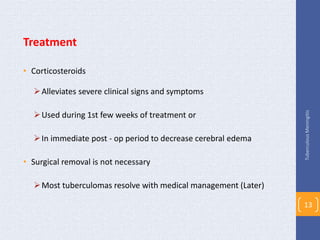
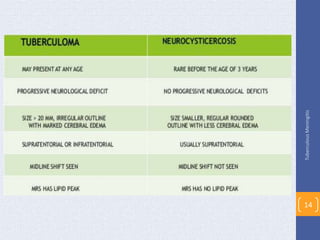
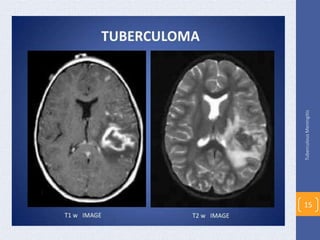
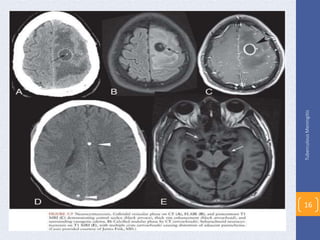
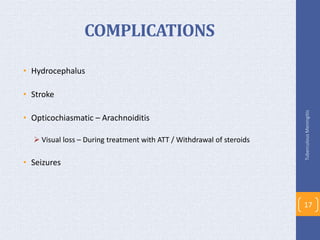
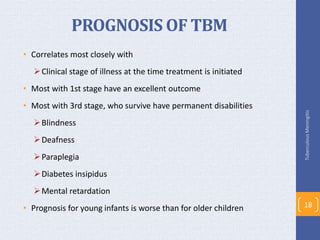
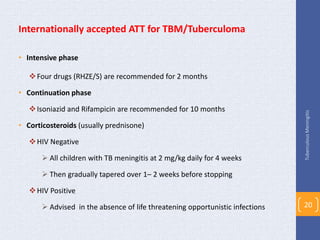
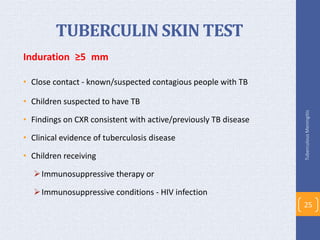
This document discusses tuberculous meningitis (TBM), the most common form of central nervous system tuberculosis. TBM can have rapid or gradual progression and commonly affects children between 6 months and 4 years old. Diagnosis involves lumbar CSF study, which typically shows lymphocytic pleocytosis and high protein levels. Treatment involves 12 months of anti-tuberculosis medications including an intensive initial phase with four drugs for 2 months followed by isoniazid and rifampin for 10 months. Prognosis depends on the clinical stage at treatment initiation, with those in the first stage having the best outcomes and those in the third stage often having permanent disabilities if they survive.