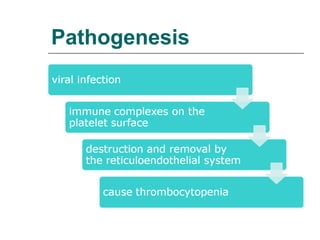
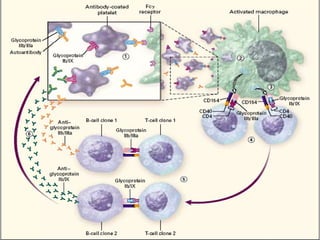
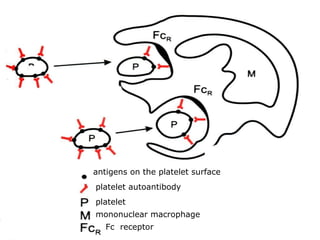
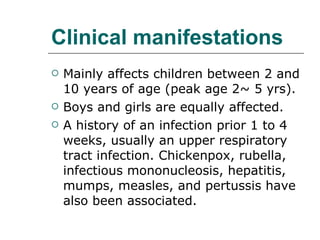
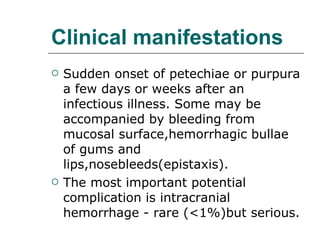
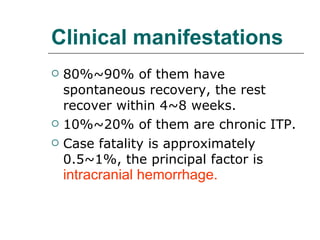
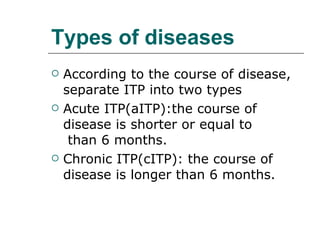
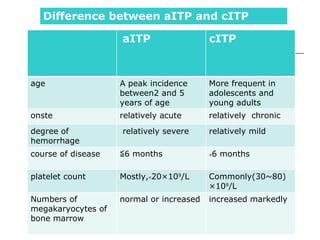
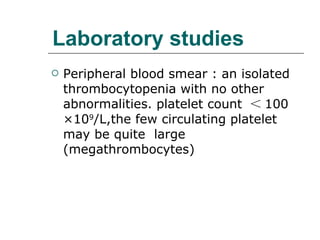
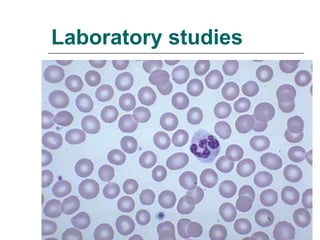
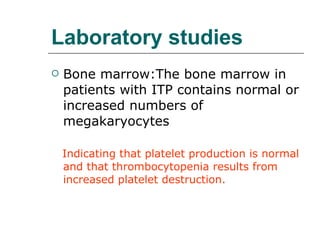
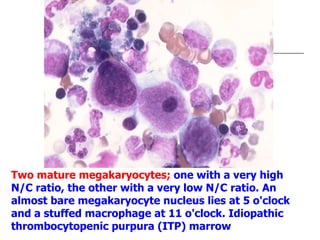
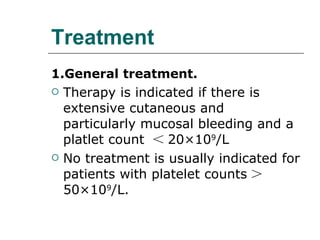
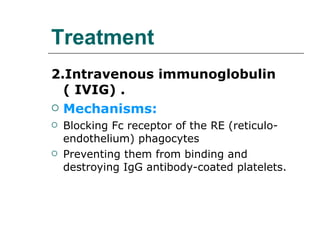
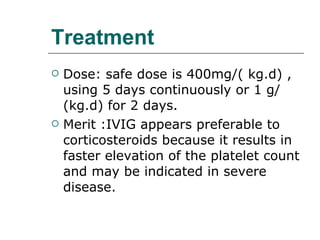
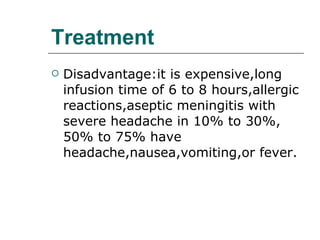
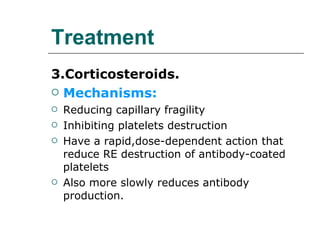
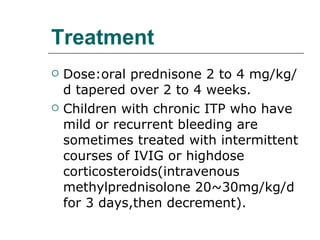
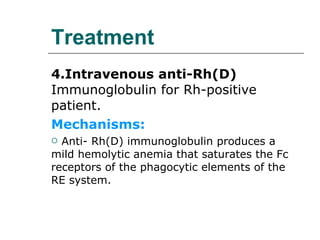
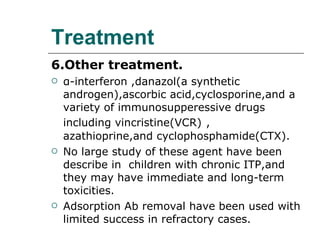
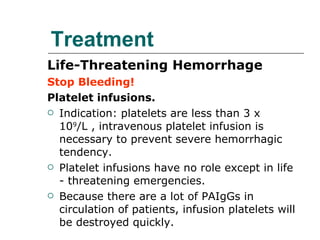
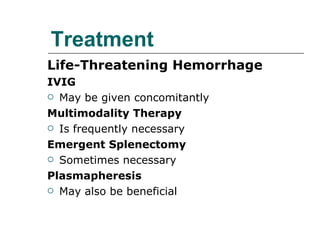
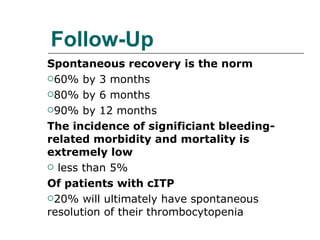
This document summarizes idiopathic thrombocytopenic purpura (ITP), a condition characterized by low platelet count due to increased platelet destruction. ITP can be acute or chronic, with acute cases typically resolving within 6 months. While the cause is unknown, it may involve autoantibodies targeting platelets. Treatment depends on severity and includes corticosteroids, IVIG, anti-D immunoglobulin, and splenectomy for chronic cases. The goal is to raise platelet counts to reduce bleeding risk.