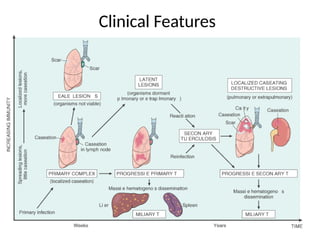
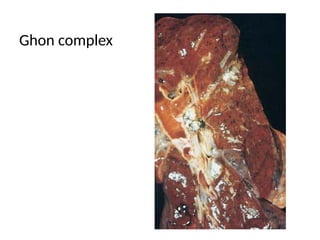
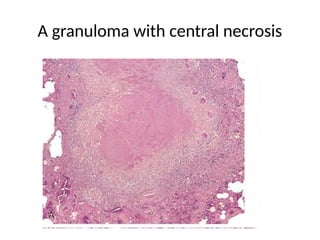
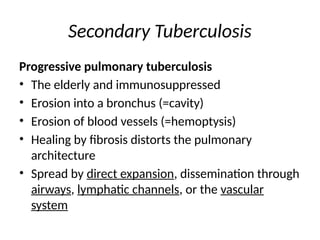
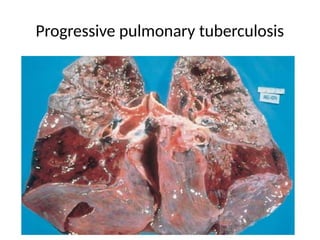
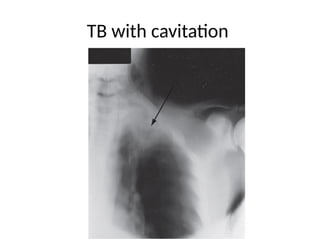
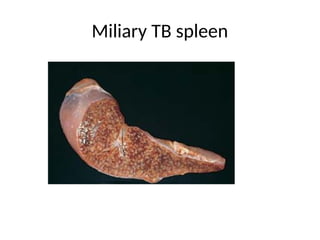
This document provides an overview of tuberculosis (TB), a disease caused by mycobacteria, primarily affecting humans and transmitted through airborne droplets. It discusses the disease's epidemiology, pathogenesis, clinical features, and connections to HIV, highlighting the complexities in diagnosing and managing the infection. The text also addresses the various forms of TB, including primary, secondary, and extrapulmonary TB, along with diagnostic approaches and treatment options.