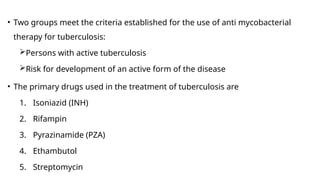
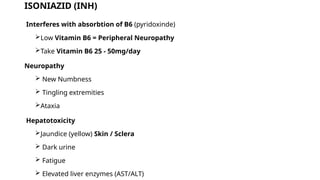
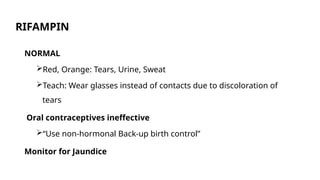
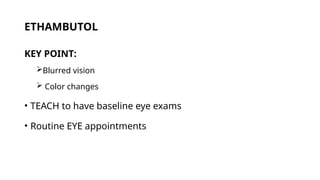
This document provides an overview of airborne diseases, focusing on tuberculosis (TB), its causes, modes of transmission, forms, and risk factors. It discusses the diagnosis, treatment options, and the importance of adherence to medication regimens for effective management and prevention of TB. Additionally, it emphasizes the public health implications of TB, particularly in vulnerable populations and the rising infection rates among individuals with HIV.