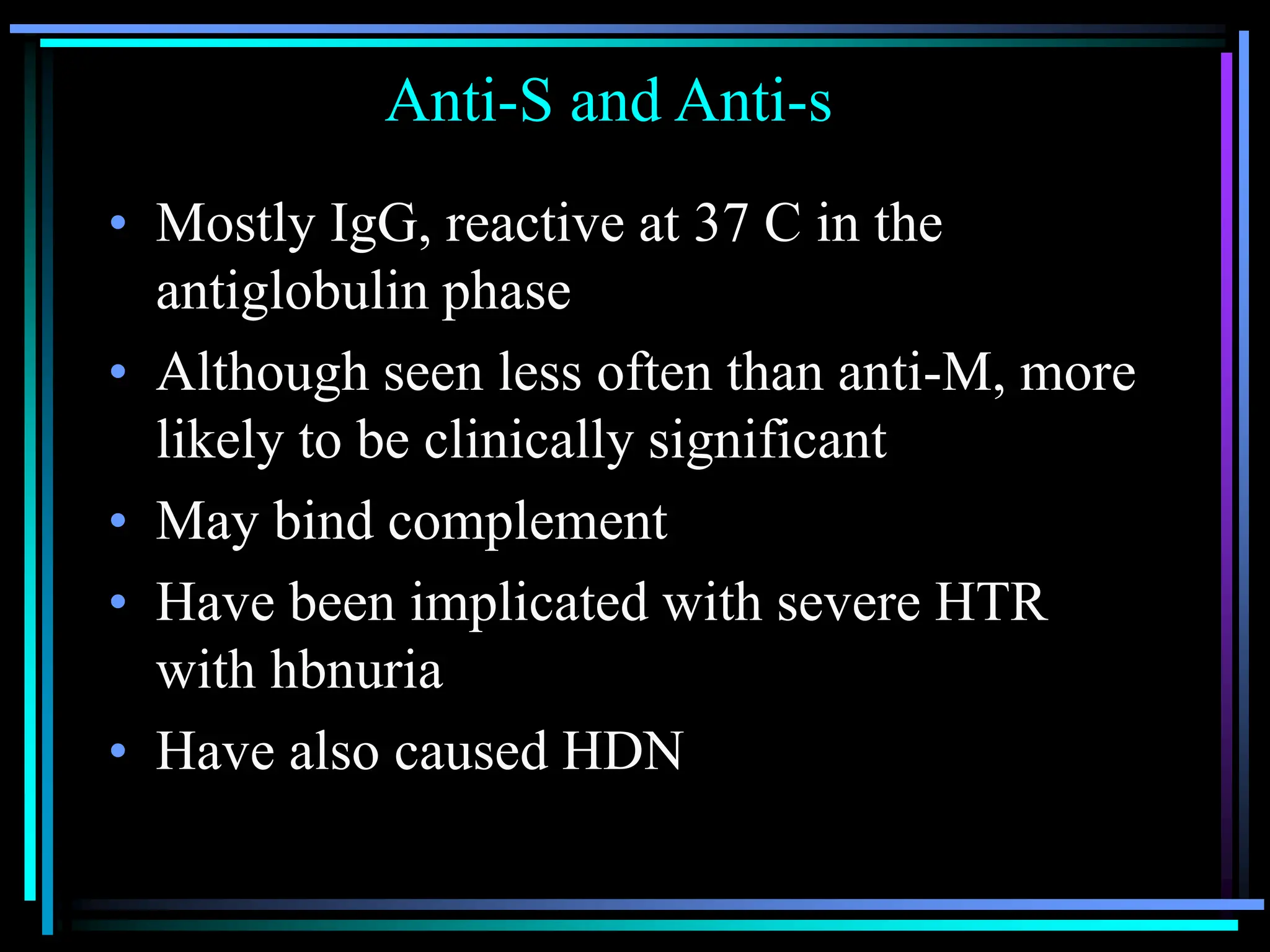
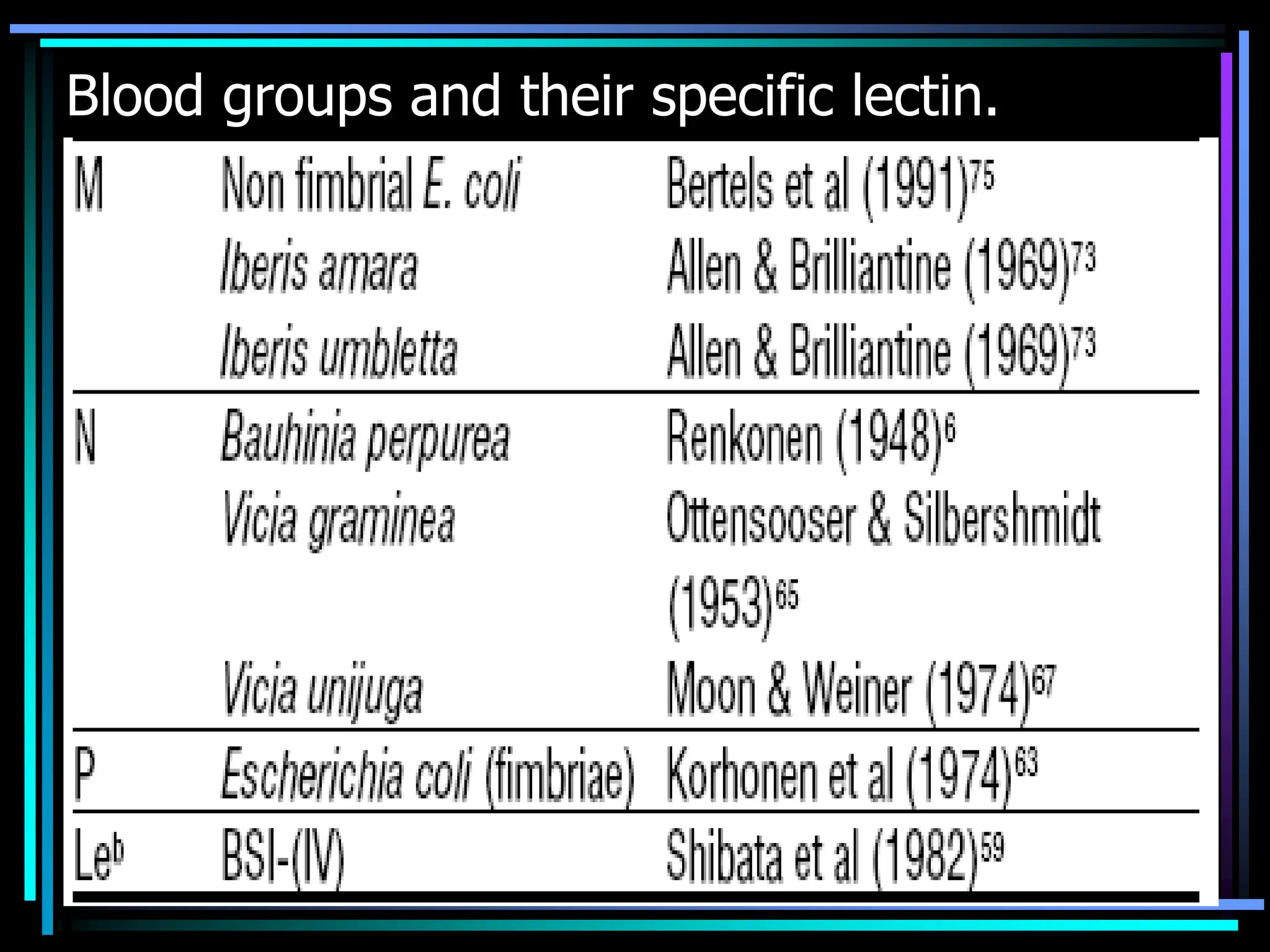
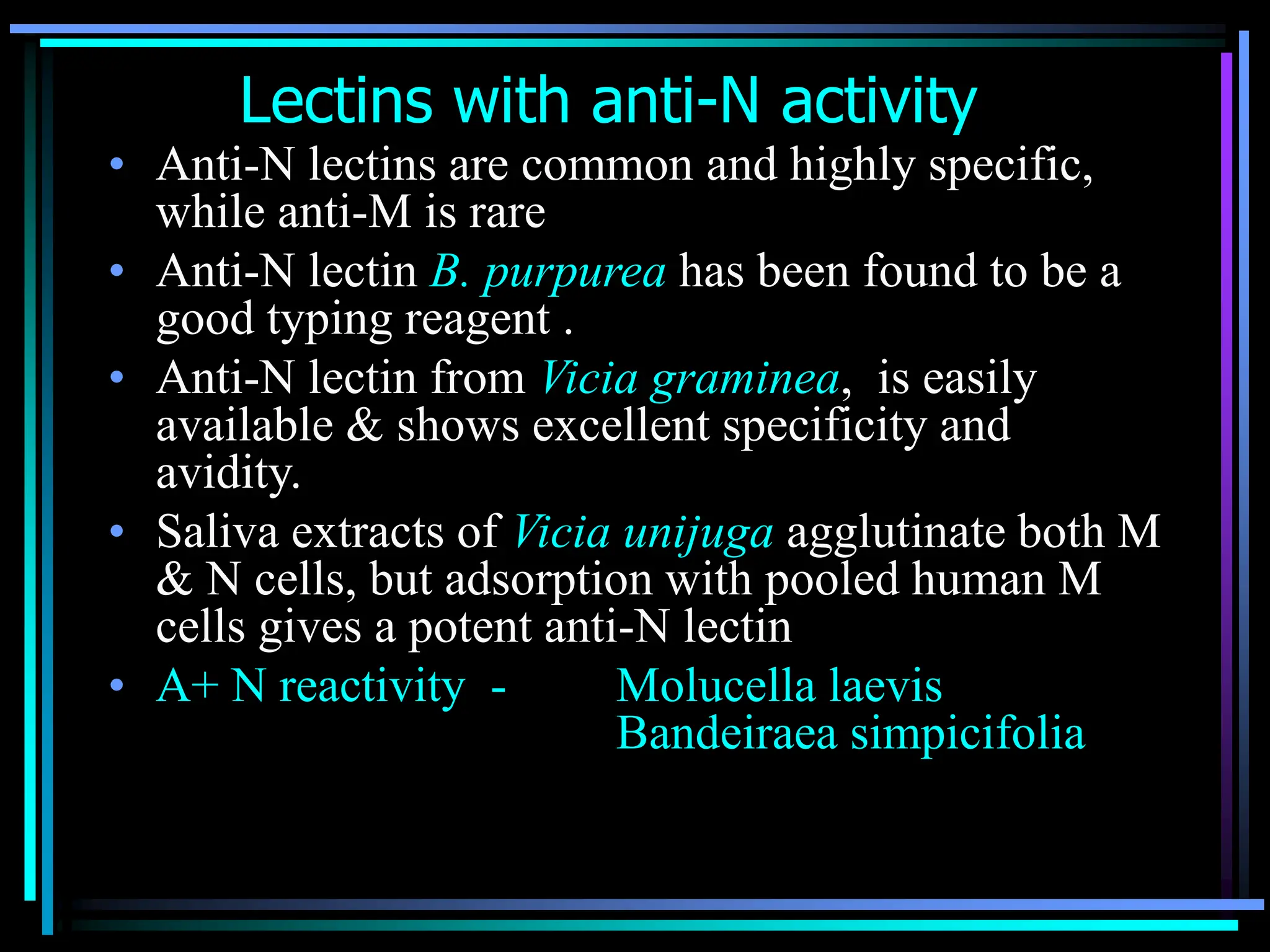
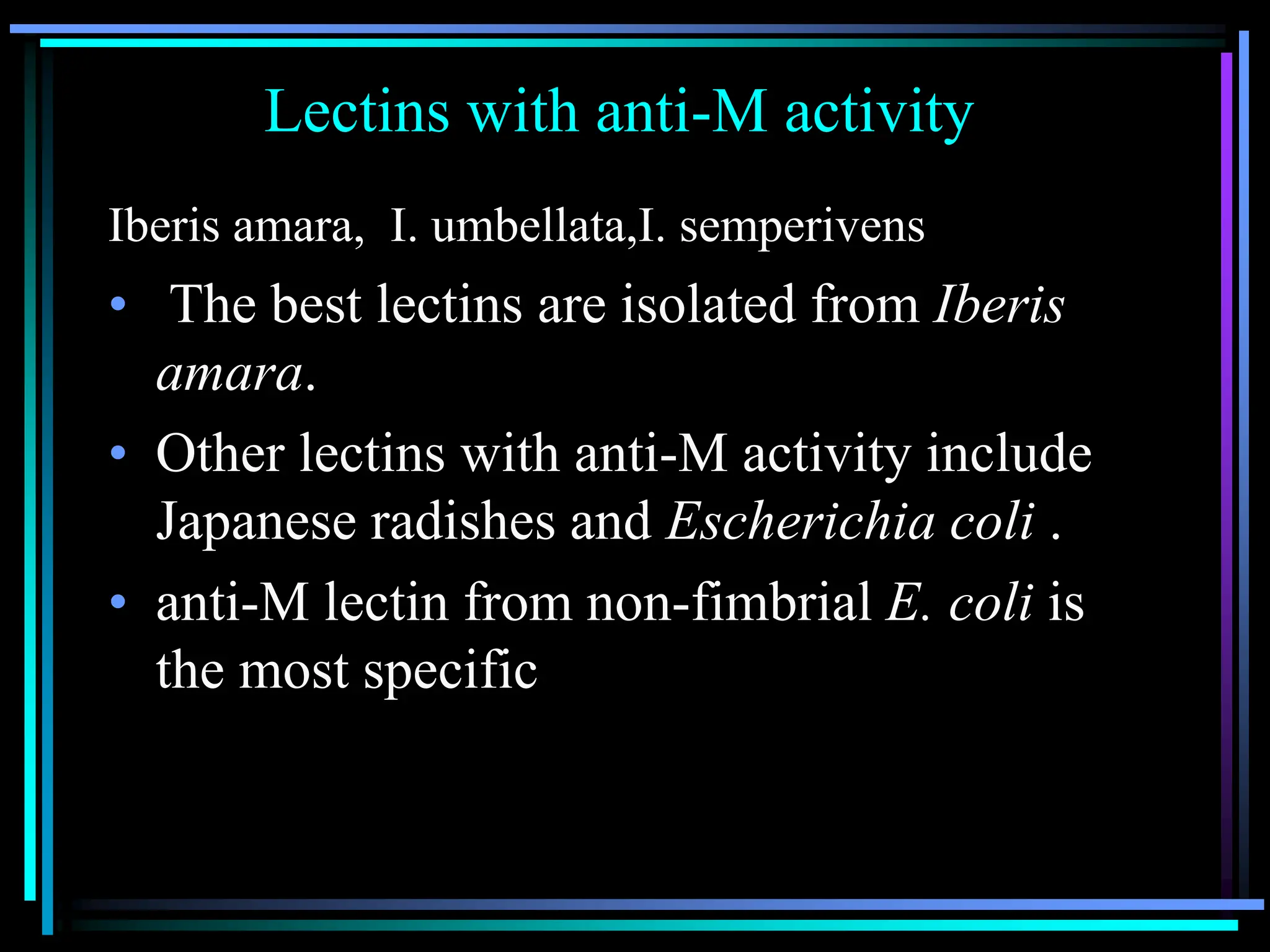
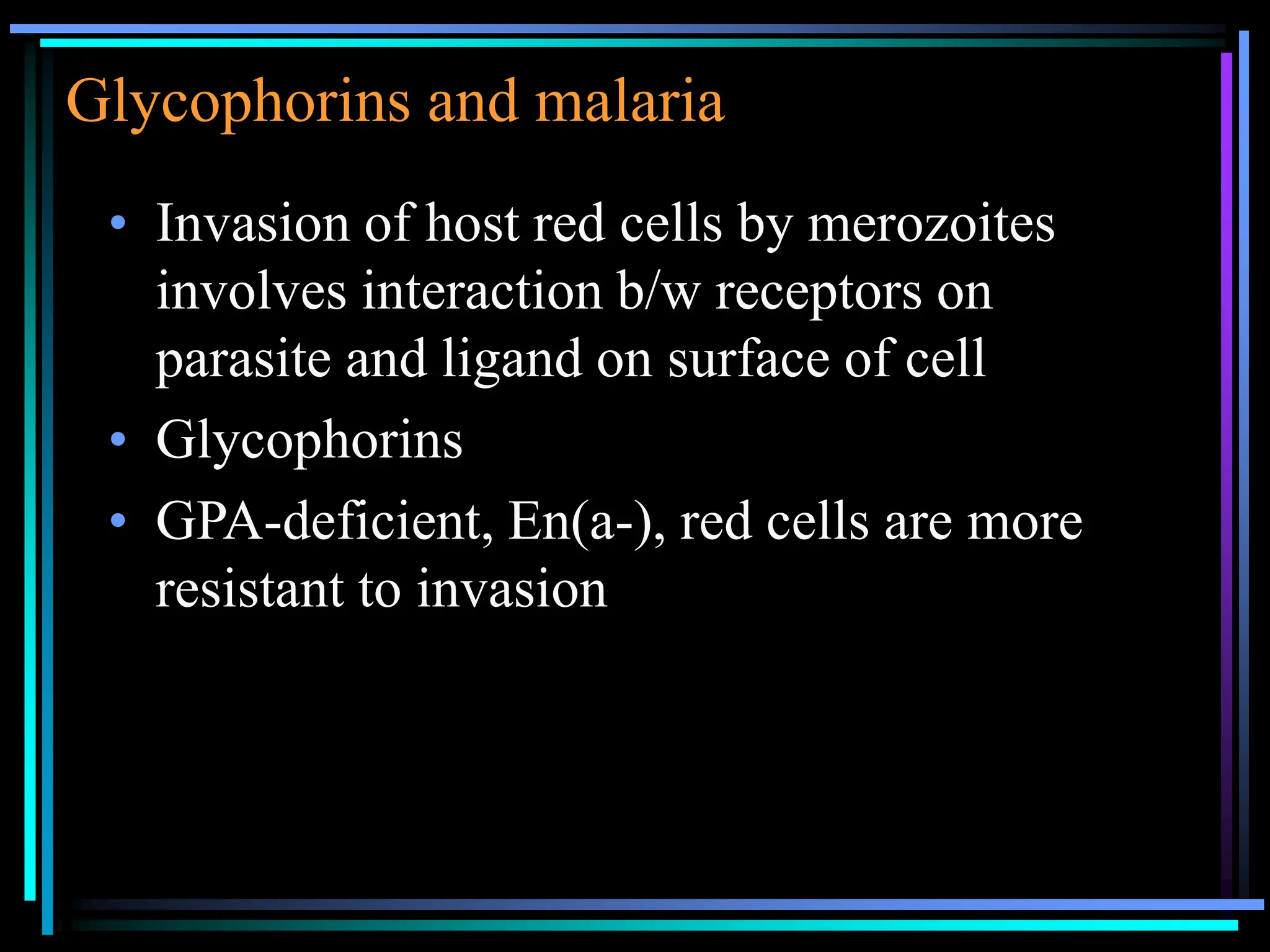
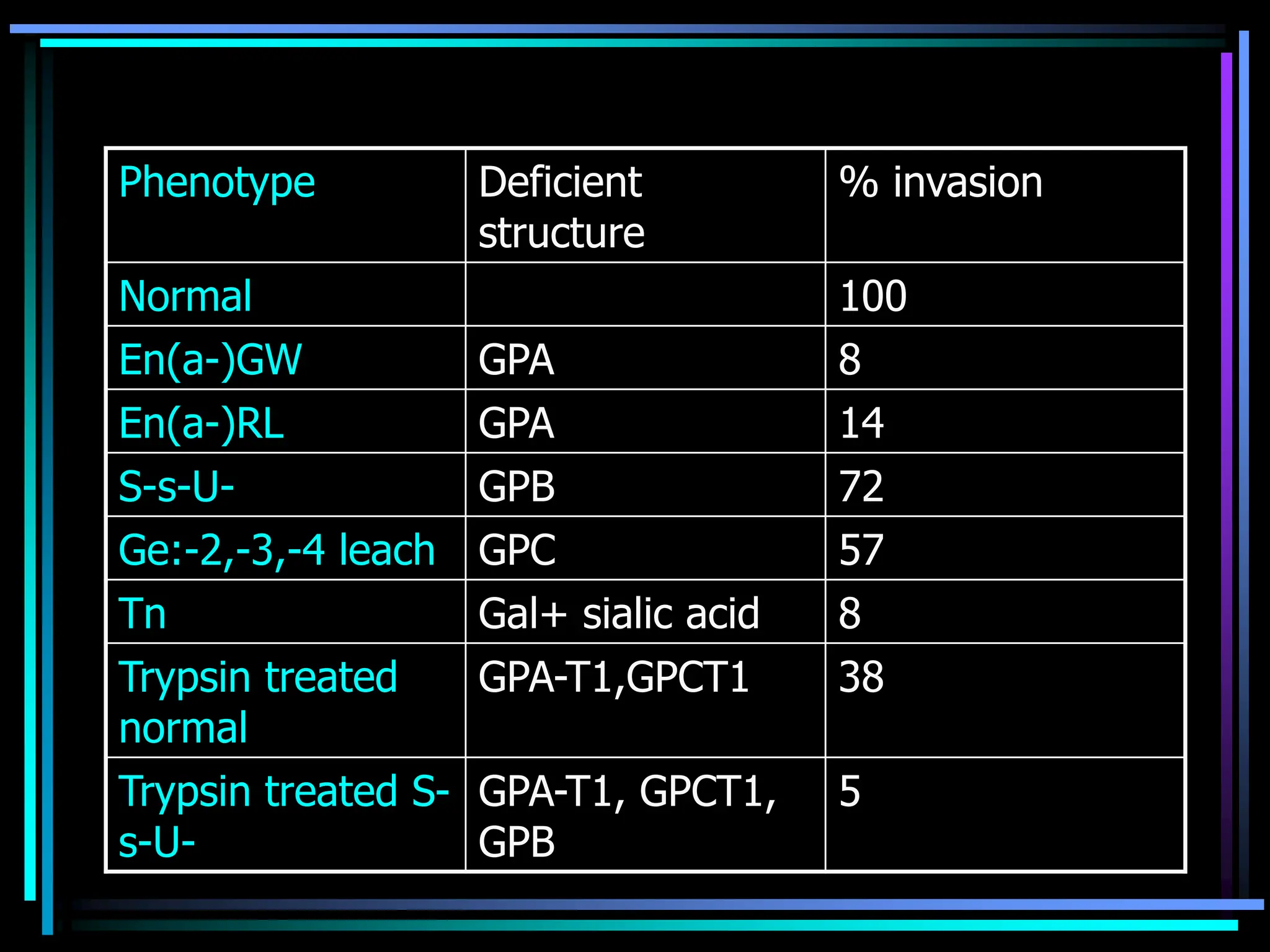
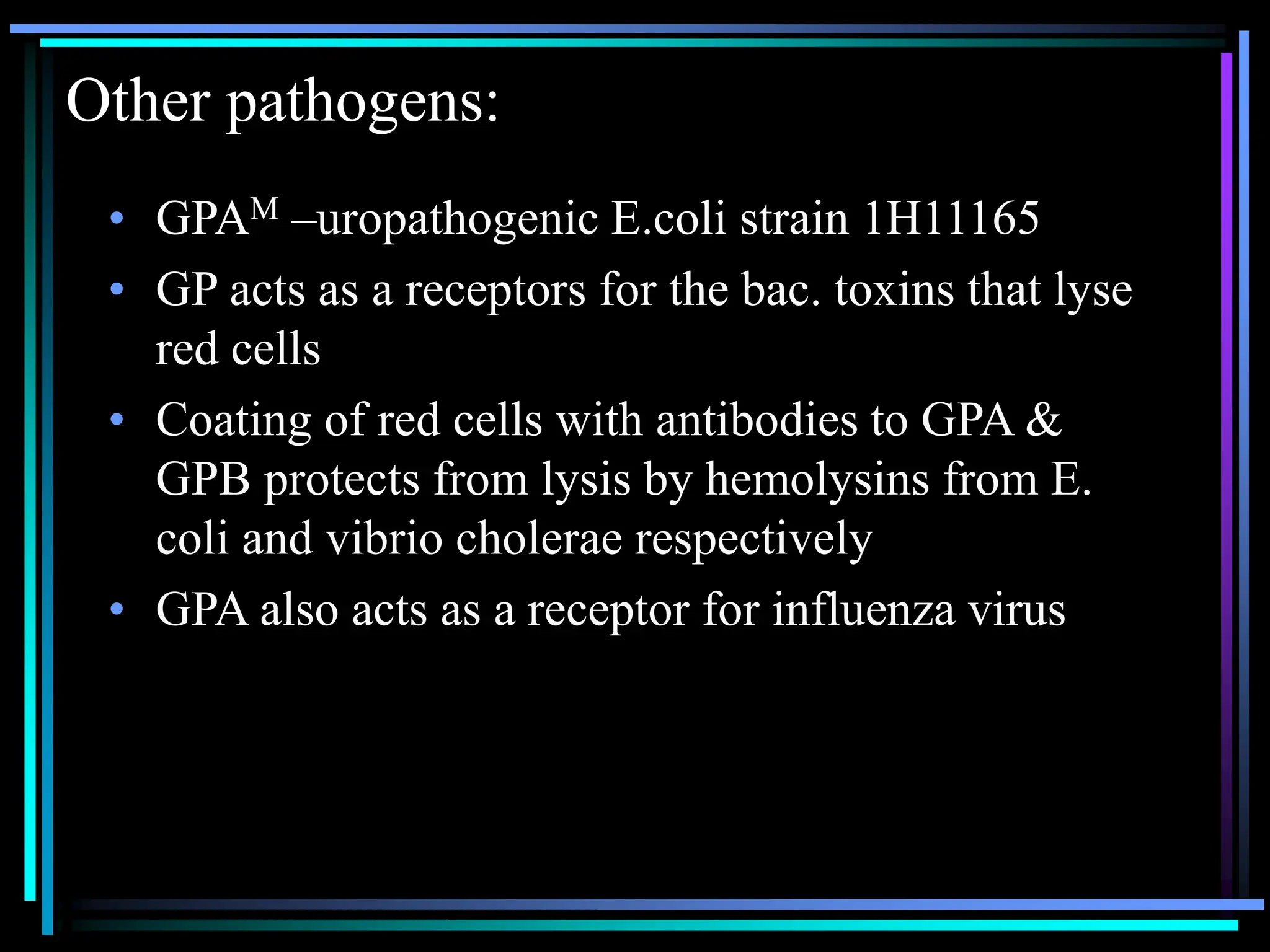
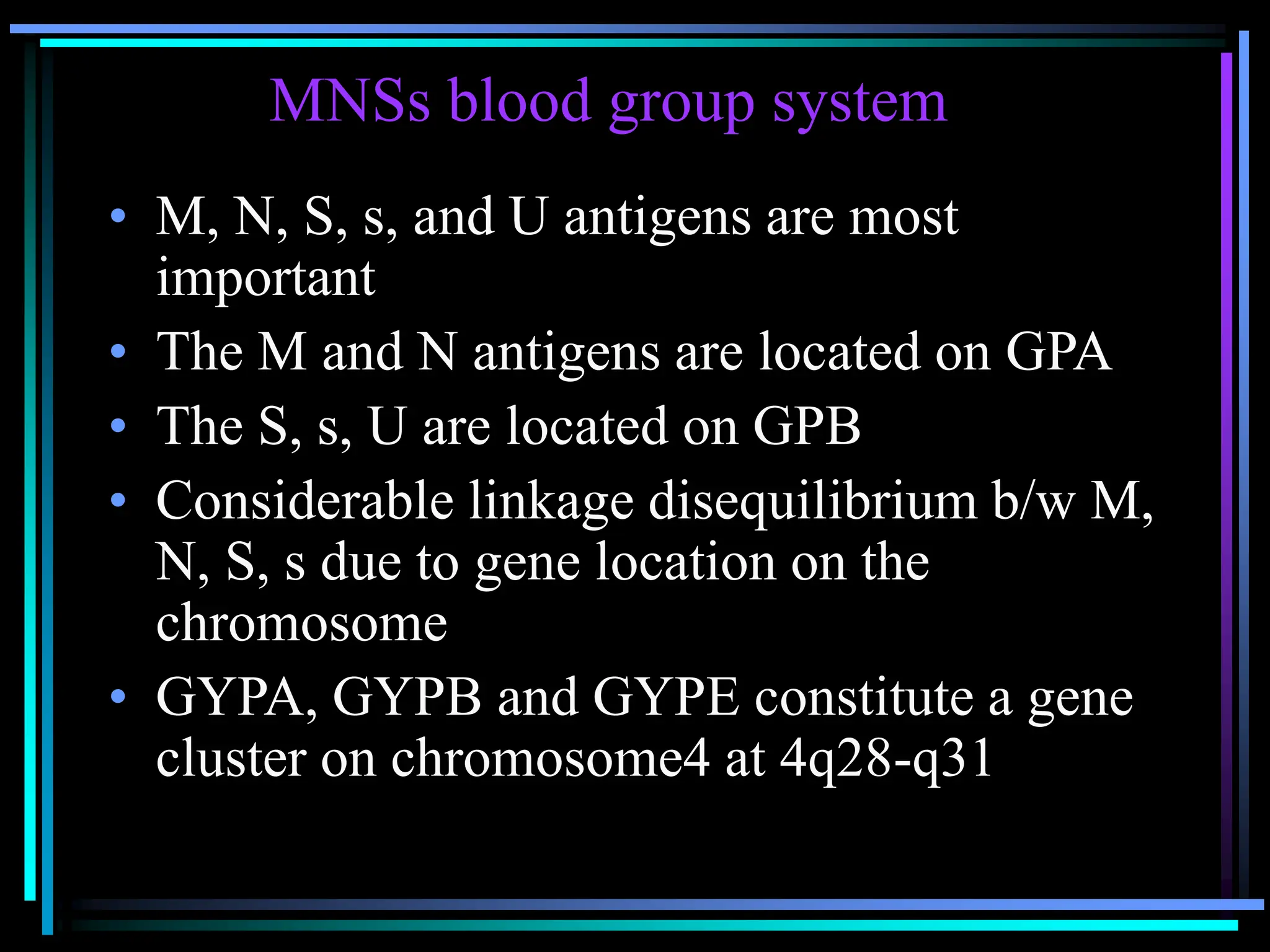
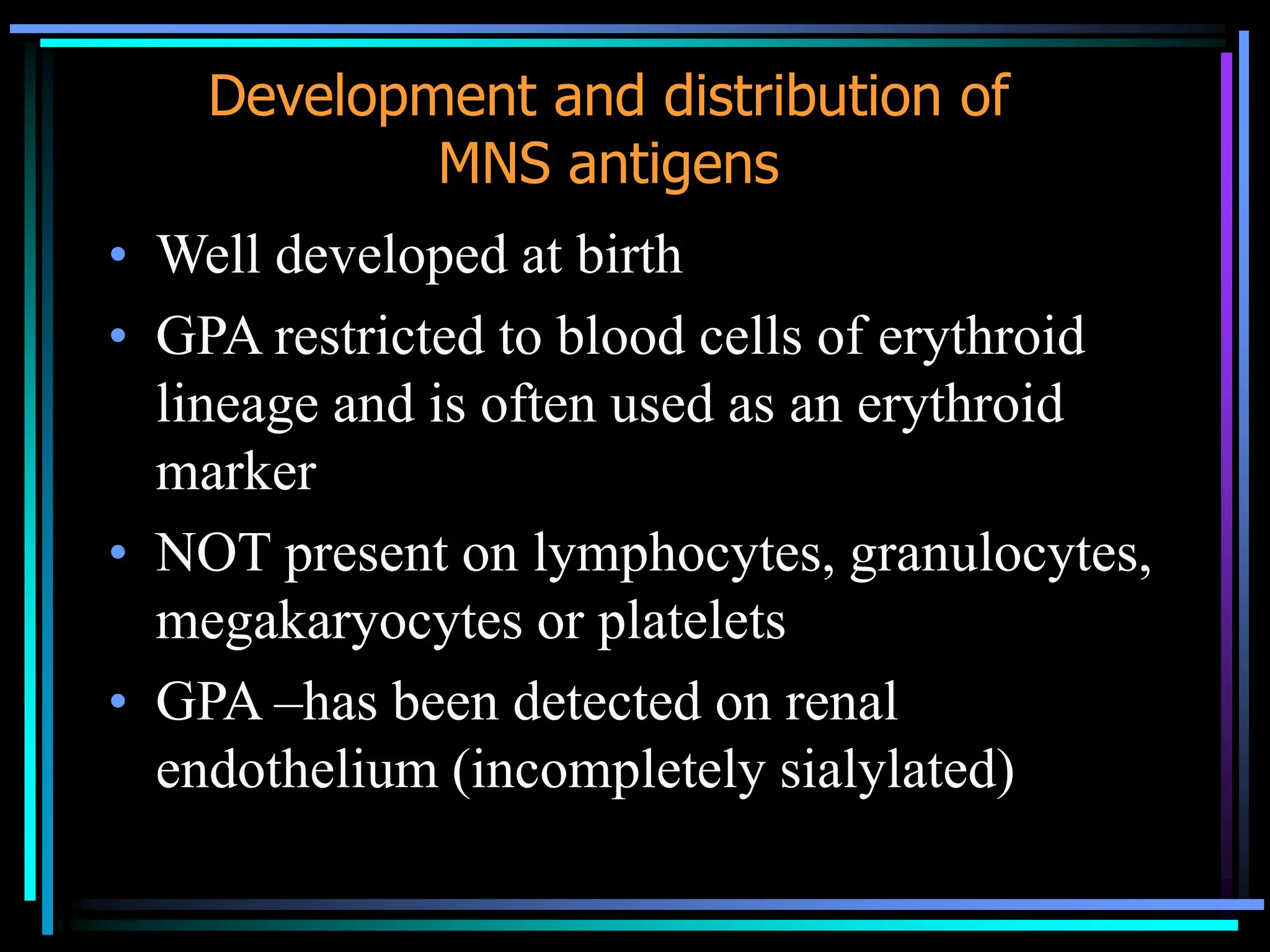
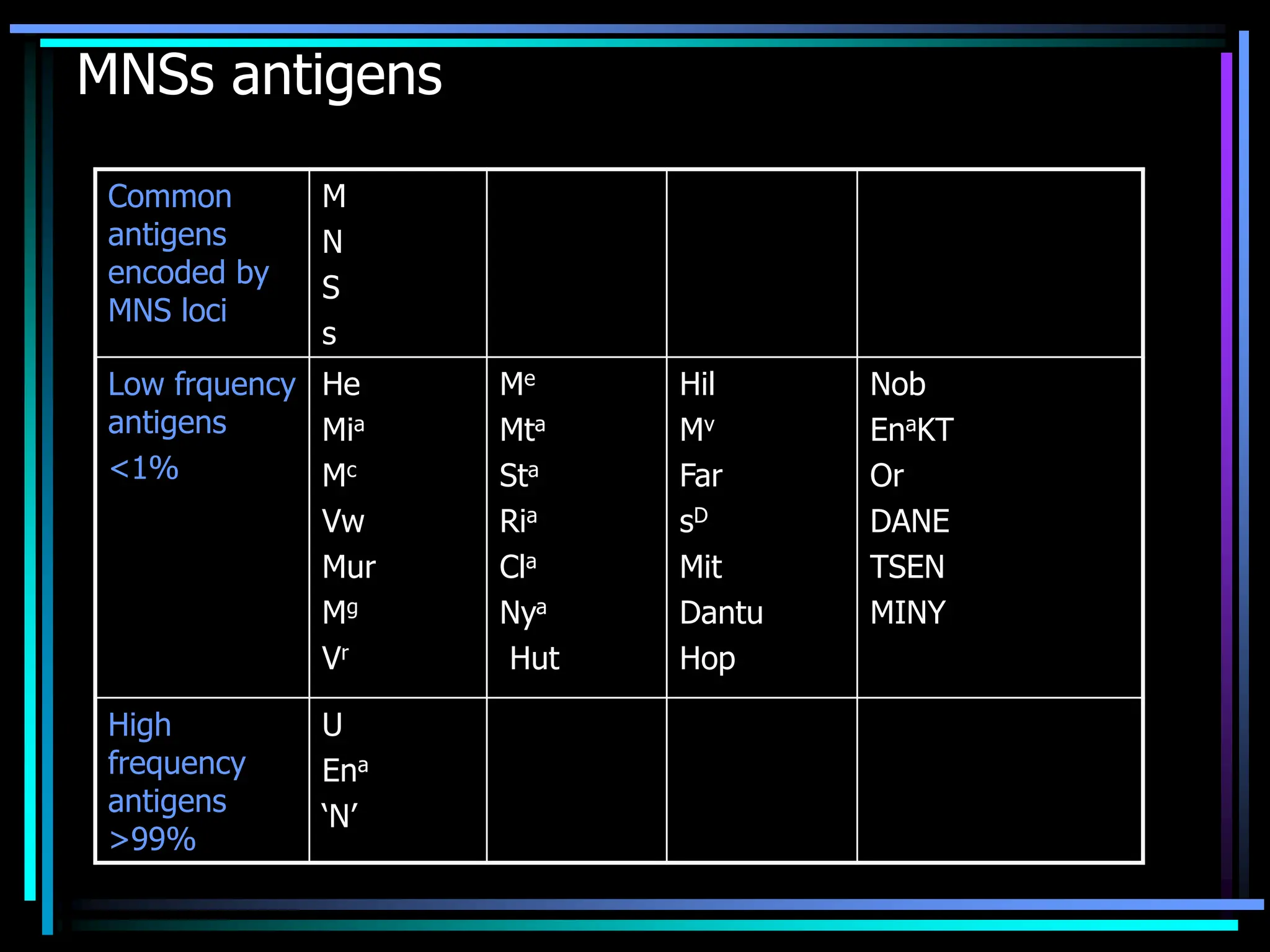
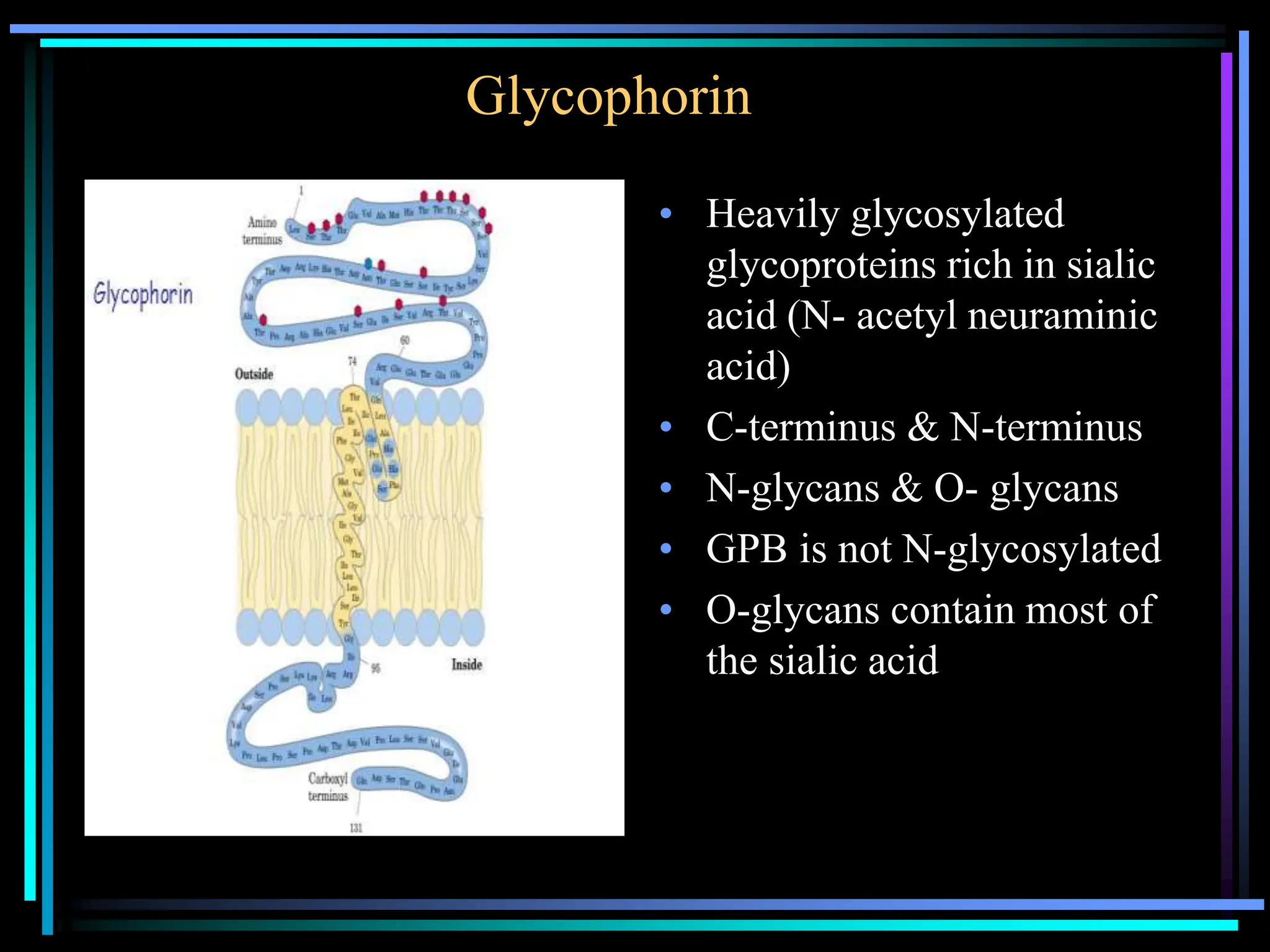
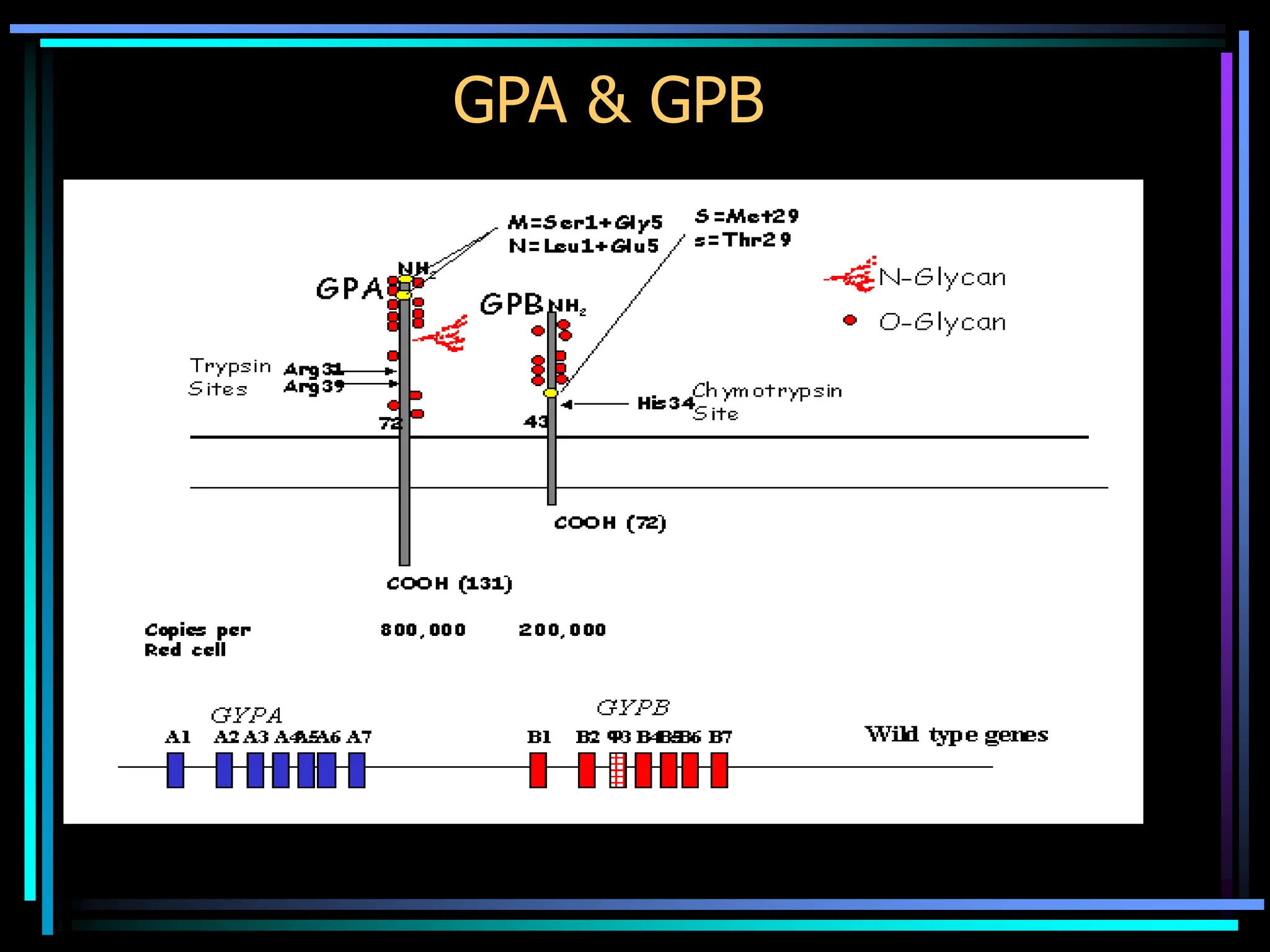
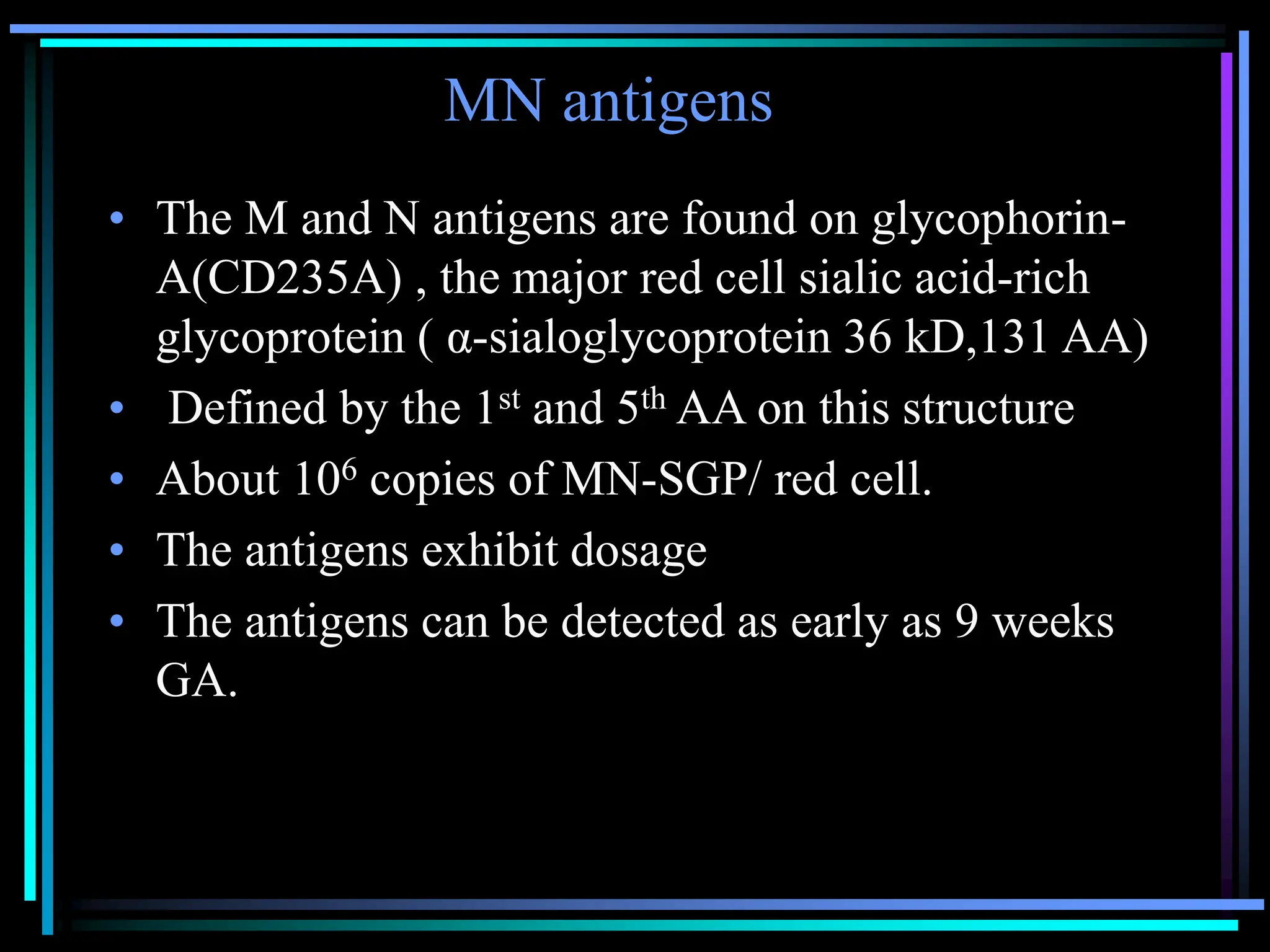
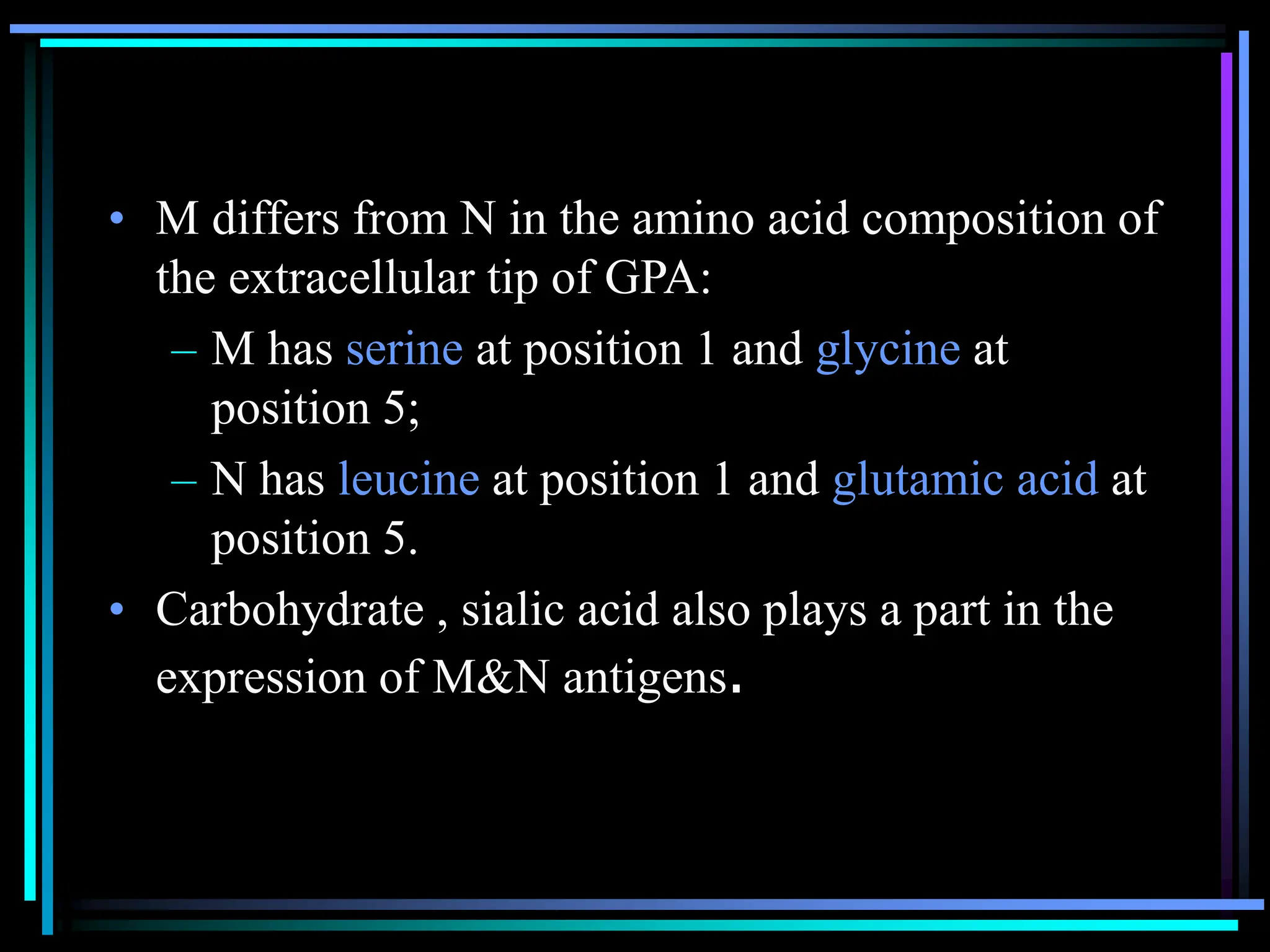
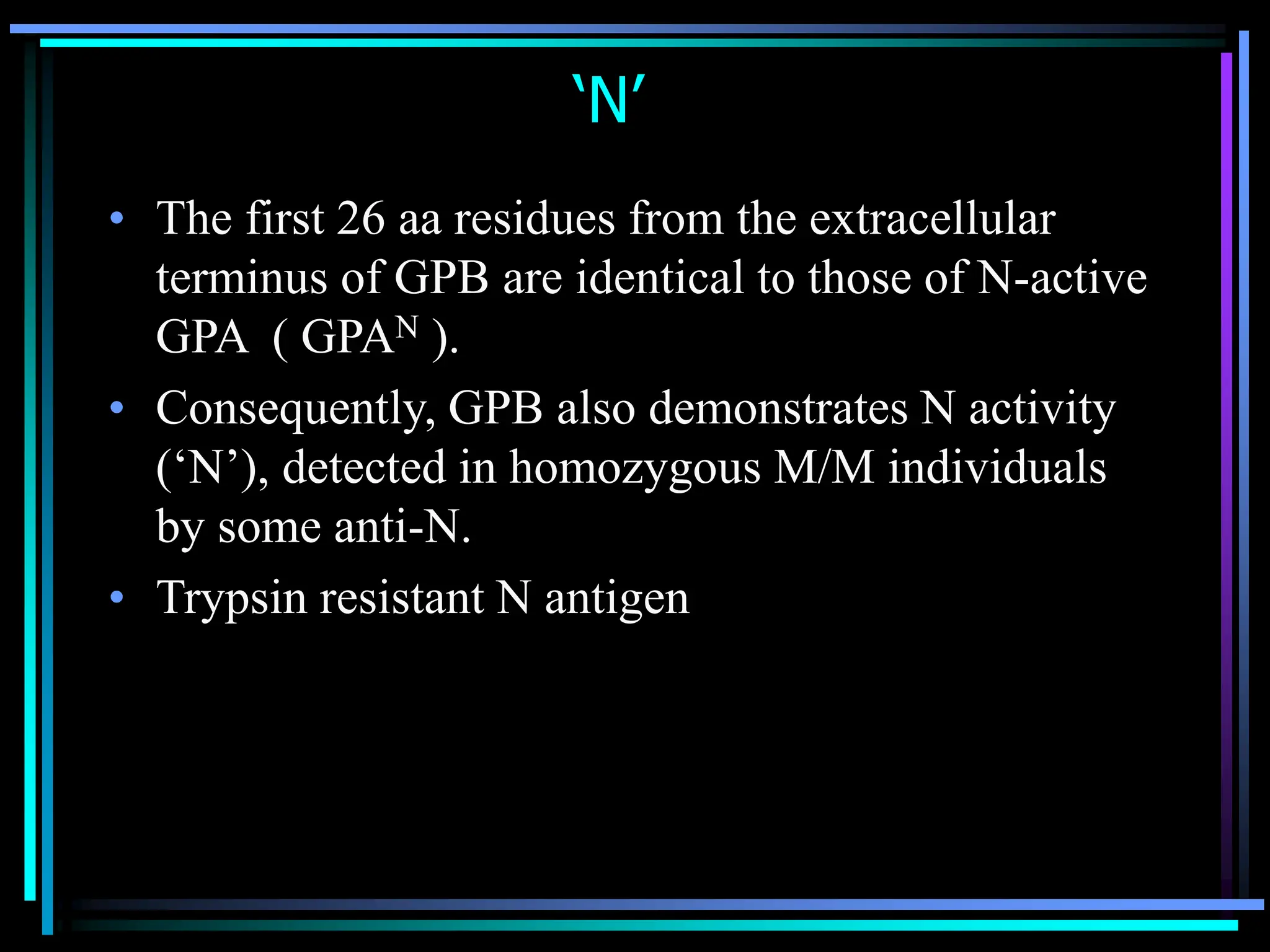
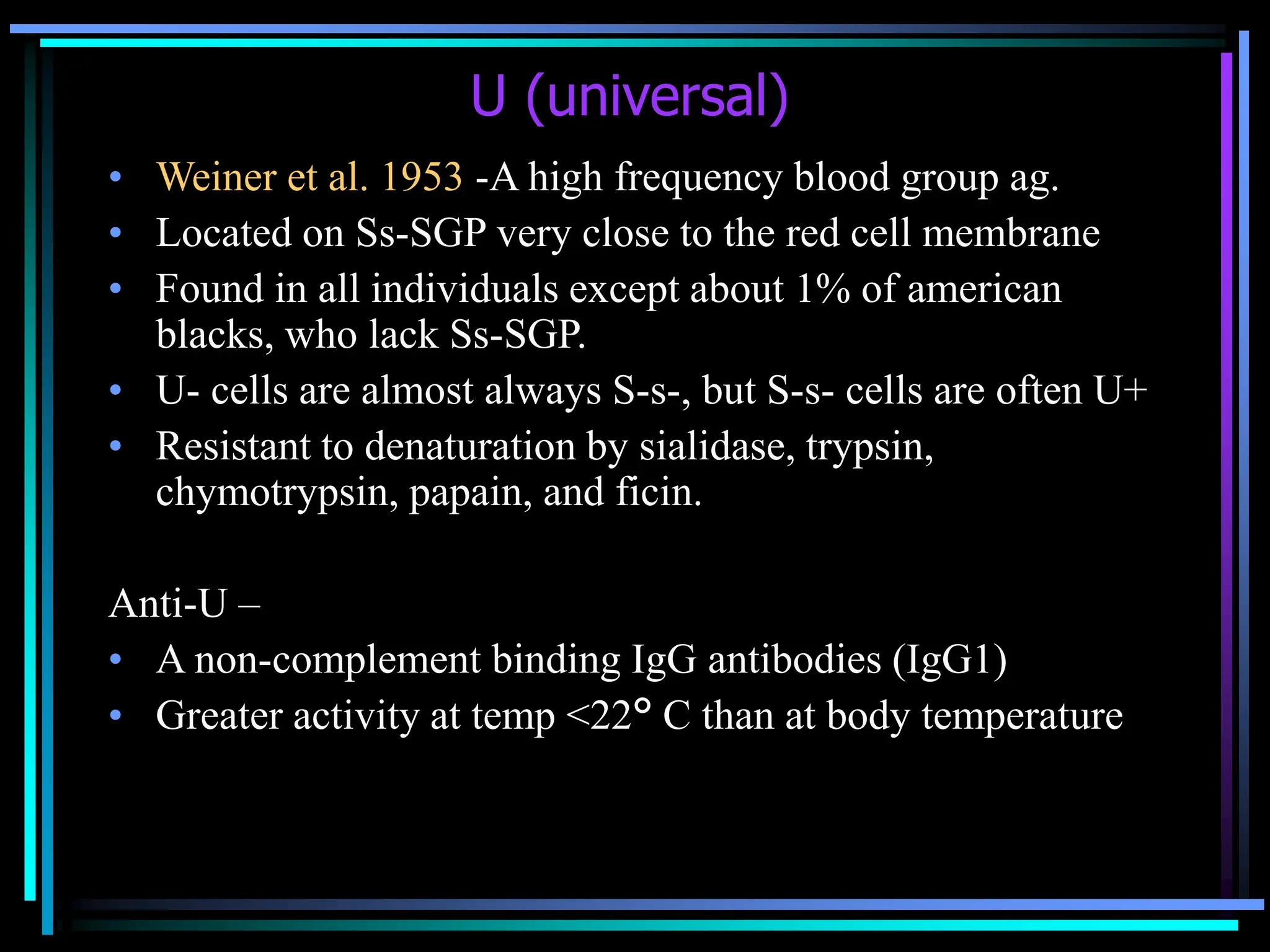
The MNS blood group system is complex, with 43 known antigens located on glycophorin A and glycophorin B proteins. The M and N antigens are located on glycophorin A and defined by amino acid variations at positions 1 and 5. The S and s antigens are located on glycophorin B and defined by amino acid variations at position 29. Other important antigens include U, which is found in nearly all individuals, and En(a-), which lacks glycophorin A expression. Antibodies in this system like anti-M, anti-N, anti-S, and anti-s can cause hemolytic transfusion reactions or hemolytic disease of the newborn if incompatible blood

![Anti-Nf
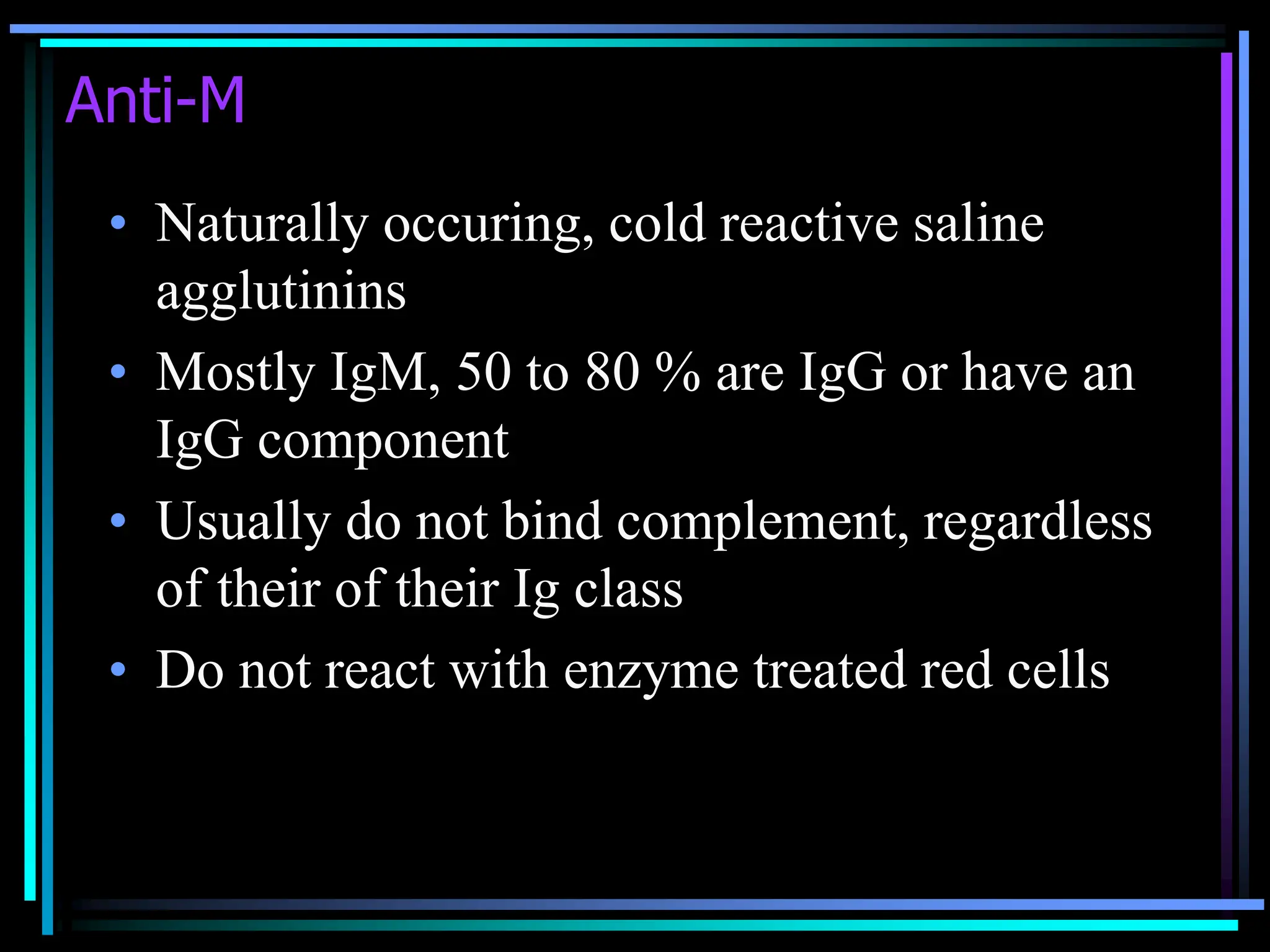
• Anti-N also seen in kidney transplant
patients maintained on chronic
hemodialysis , regardless of their MN type,
who are dialized on equipment sterilized
with formaldehyde
• Ab disappeared after transplantation
• 21 to 27 % of dialysis patients
[Am J Nephrol 1995]](https://image.slidesharecdn.com/mns-240220082418-1896cde2/75/MNS-Blood-group-system-powerpoint-in-ppt-26-2048.jpg)