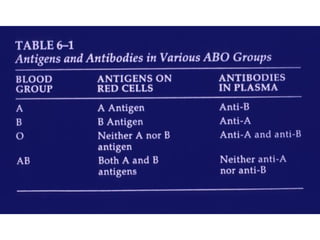
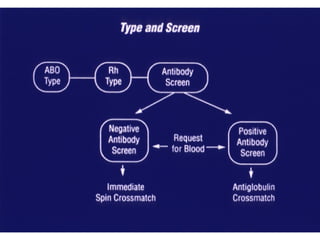
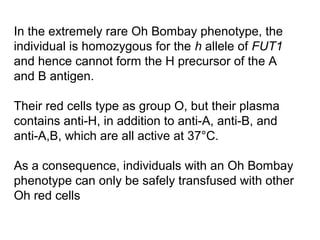
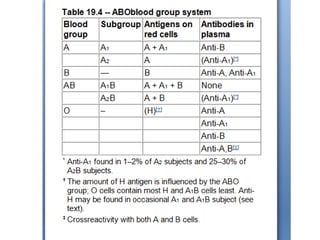
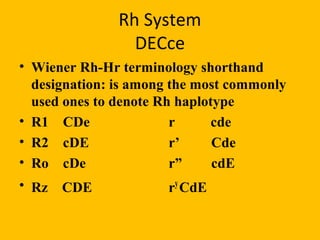
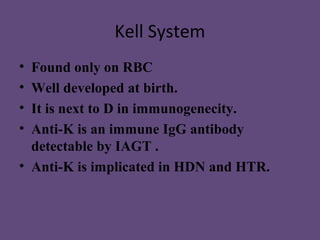
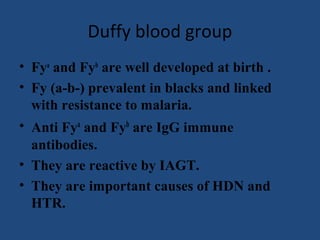
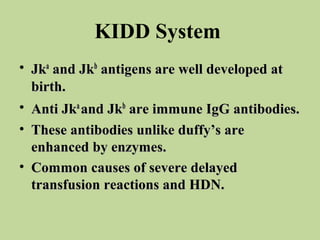
The document summarizes key information about major blood group systems including ABO, Rh, Lewis, Kell, Duffy, and Kidd. It describes the antigens and genes involved in determining blood group types, frequencies in different populations, clinically significant antibodies, and associations with diseases.
![ABO SYSTEM
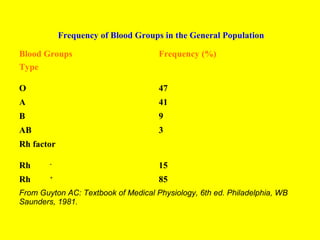
• There are four main blood groups: A, B, AB
and O.
• In the British Caucasian population, the
frequency of group A is 42%, B 9%, AB 3%, and
O 46%
• there is racial variation in these frequencies.[6]
The epitopes of ABO antigens are determined
by carbohydrates (sugars), which are linked
either to polypeptides (forming glycoproteins)
or to lipids (glycolipids).](https://image.slidesharecdn.com/bloodgroup-130129161045-phpapp02/85/Blood-group-2-320.jpg)