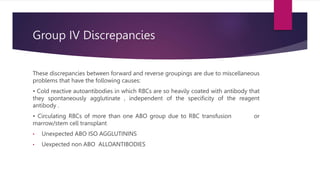
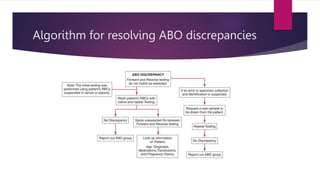
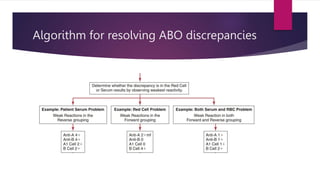
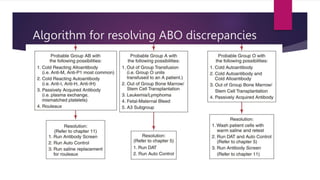
Group I discrepancies involve weak or missing antibodies in reverse grouping due to conditions like newborn status, immunosuppression, or subgroups. Group II discrepancies involve weak or missing antigens in forward grouping, which can be caused by subgroups or diseases weakening antigens. Group III discrepancies are due to rouleaux formation or pseudoagglutination from elevated proteins. Group IV involves miscellaneous issues like cold antibodies, mixed field RBCs, or unexpected antibodies. Resolving discrepancies involves investigating patient history, enhancing weak reactions, addressing rouleaux or cold antibodies, determining if multiple RBC populations exist, and following an algorithmic approach.