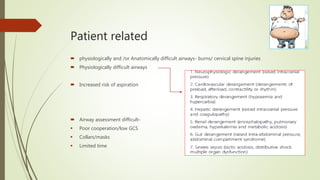
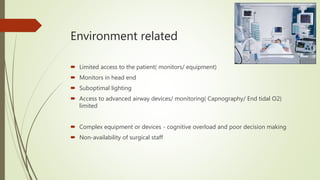
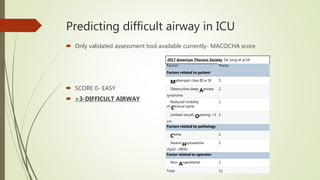
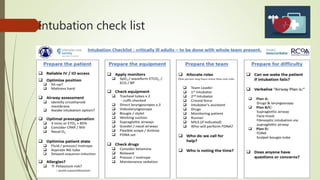
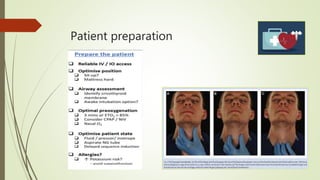
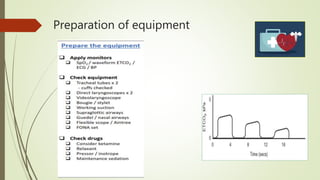
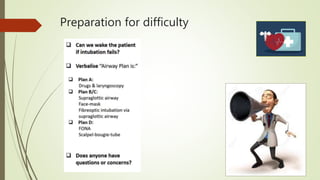
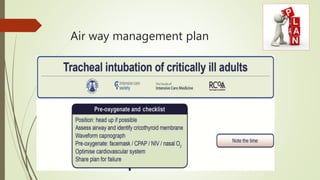
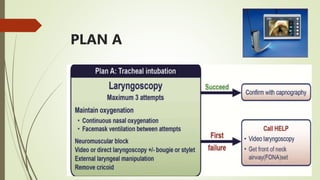
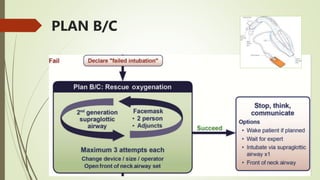
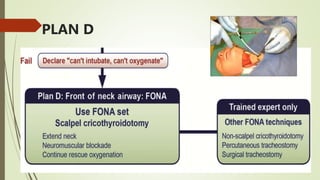
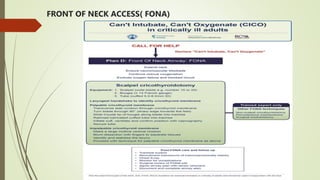
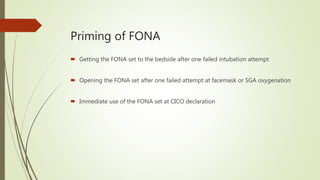
This document discusses intubation in critical care settings. It notes that ICU intubations carry high risks, with 25% of patients experiencing severe hypoxemia and 60% of airway incidents resulting in death or neurological injury. Difficulties arise from factors relating to the patient, staff, and environment. The MACOCHA score can help predict difficult airways. The Difficult Airway Society guidelines recommend preparation, checklists, backup plans including front-of-neck access, and continuous monitoring after intubation to reduce risks from these high-stakes procedures in critically ill patients.