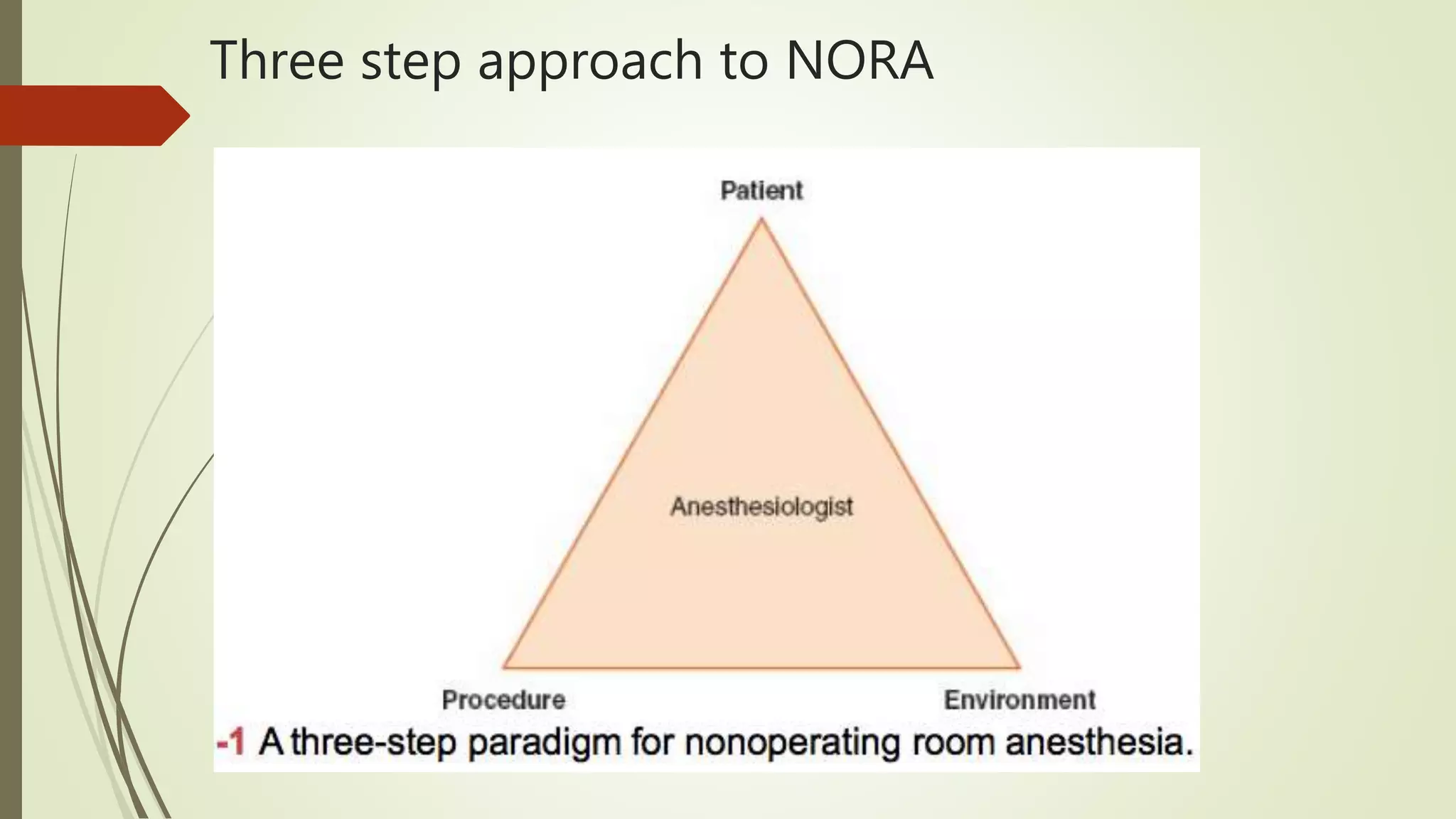
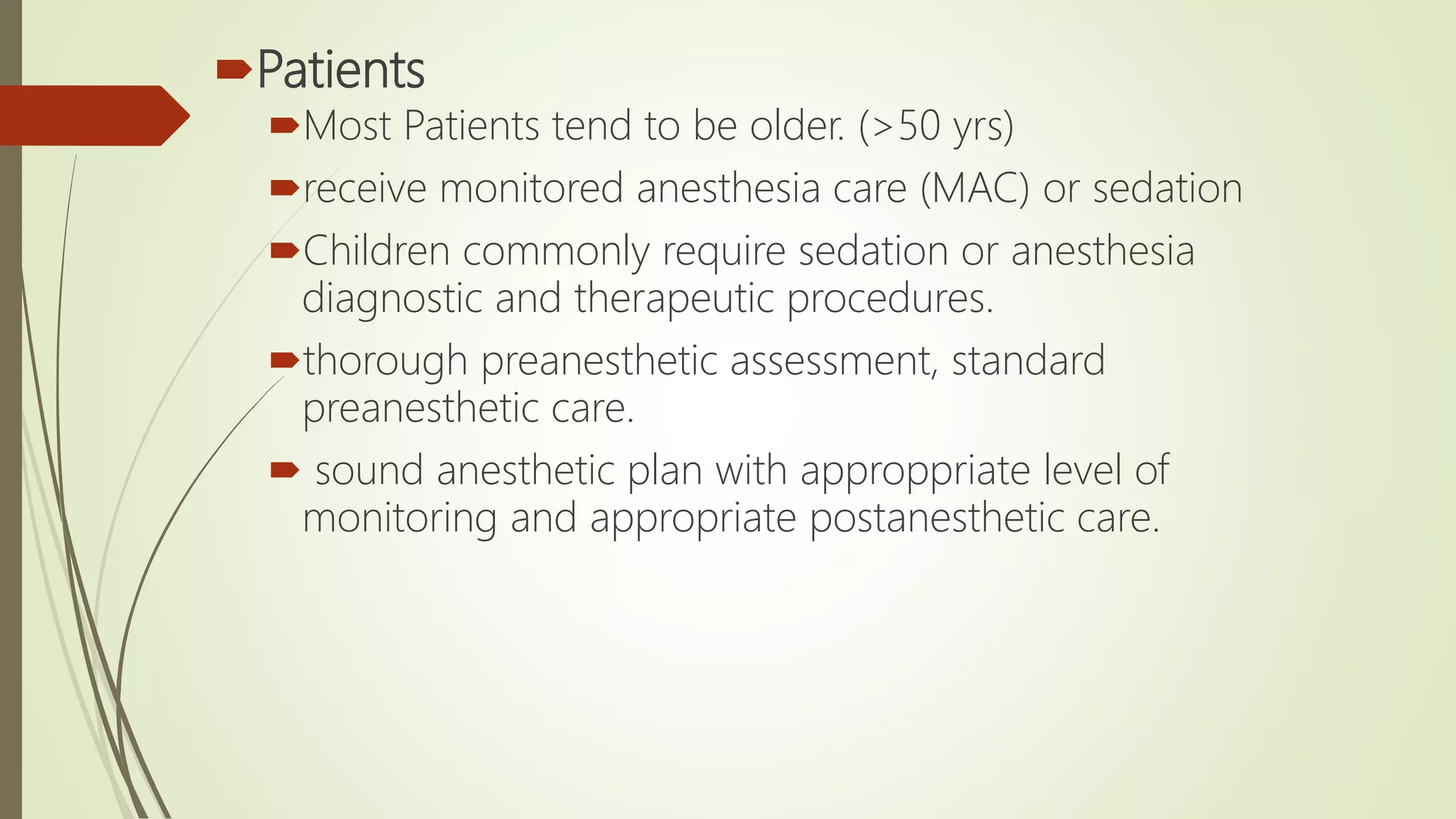
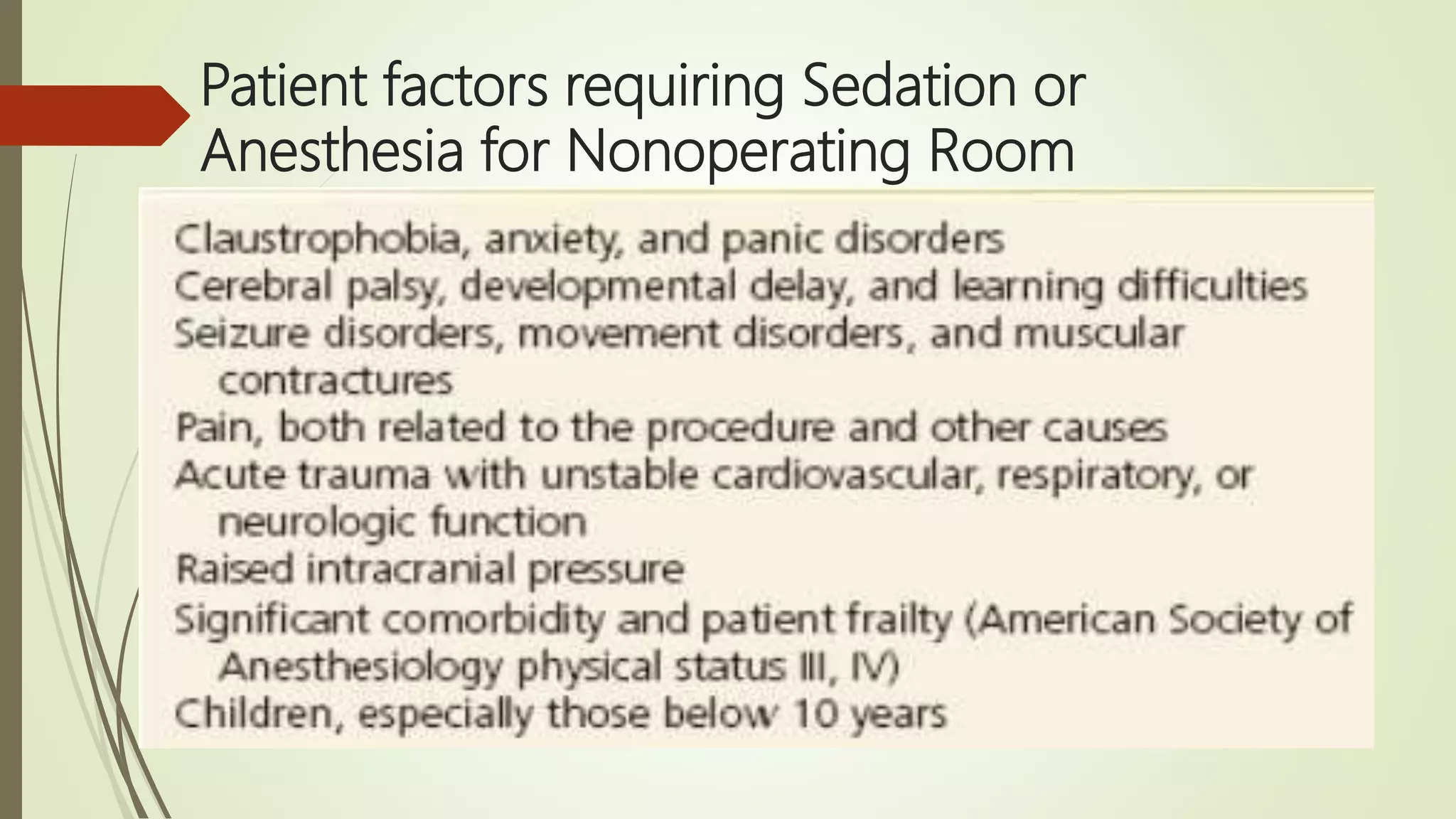
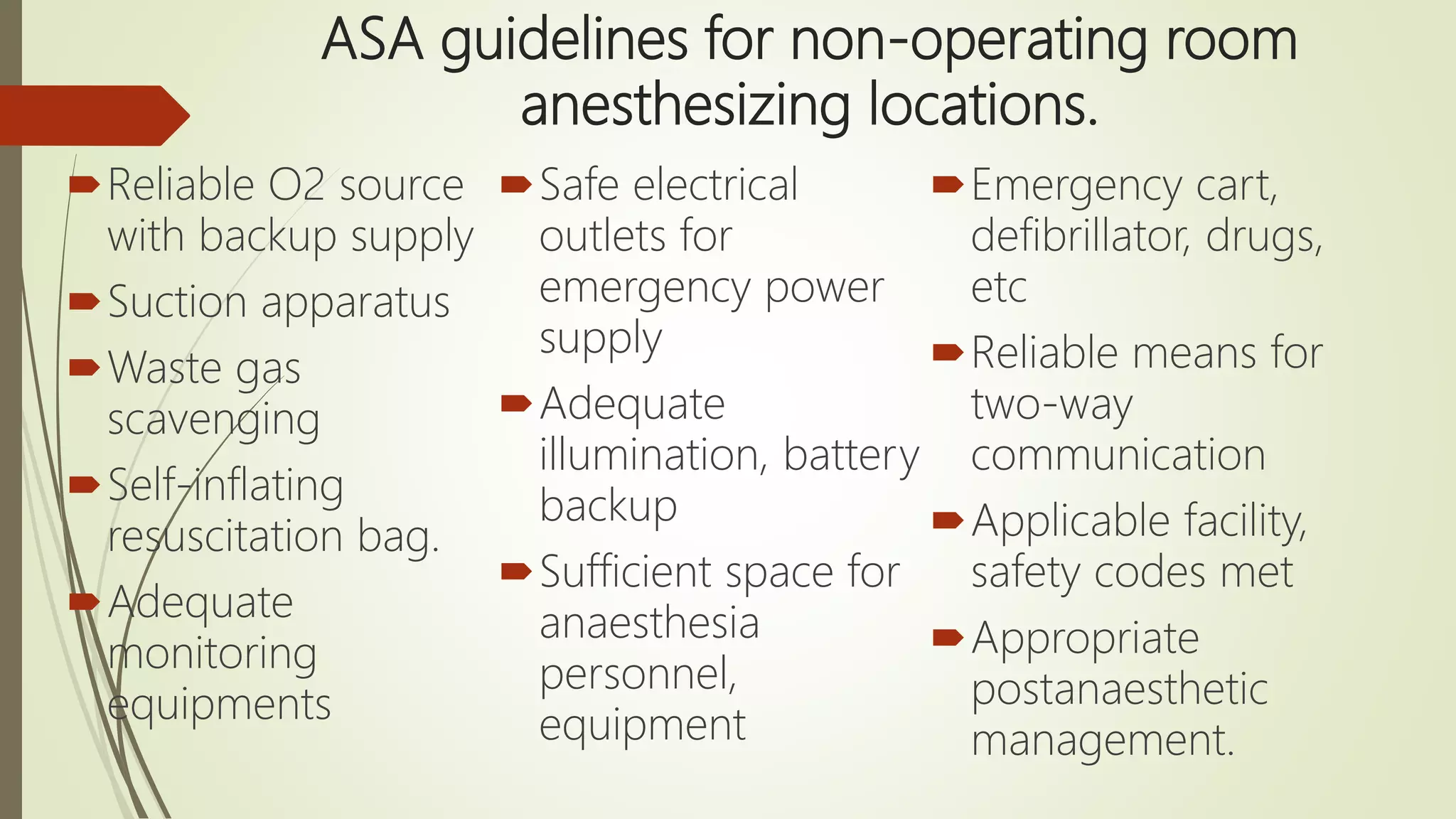
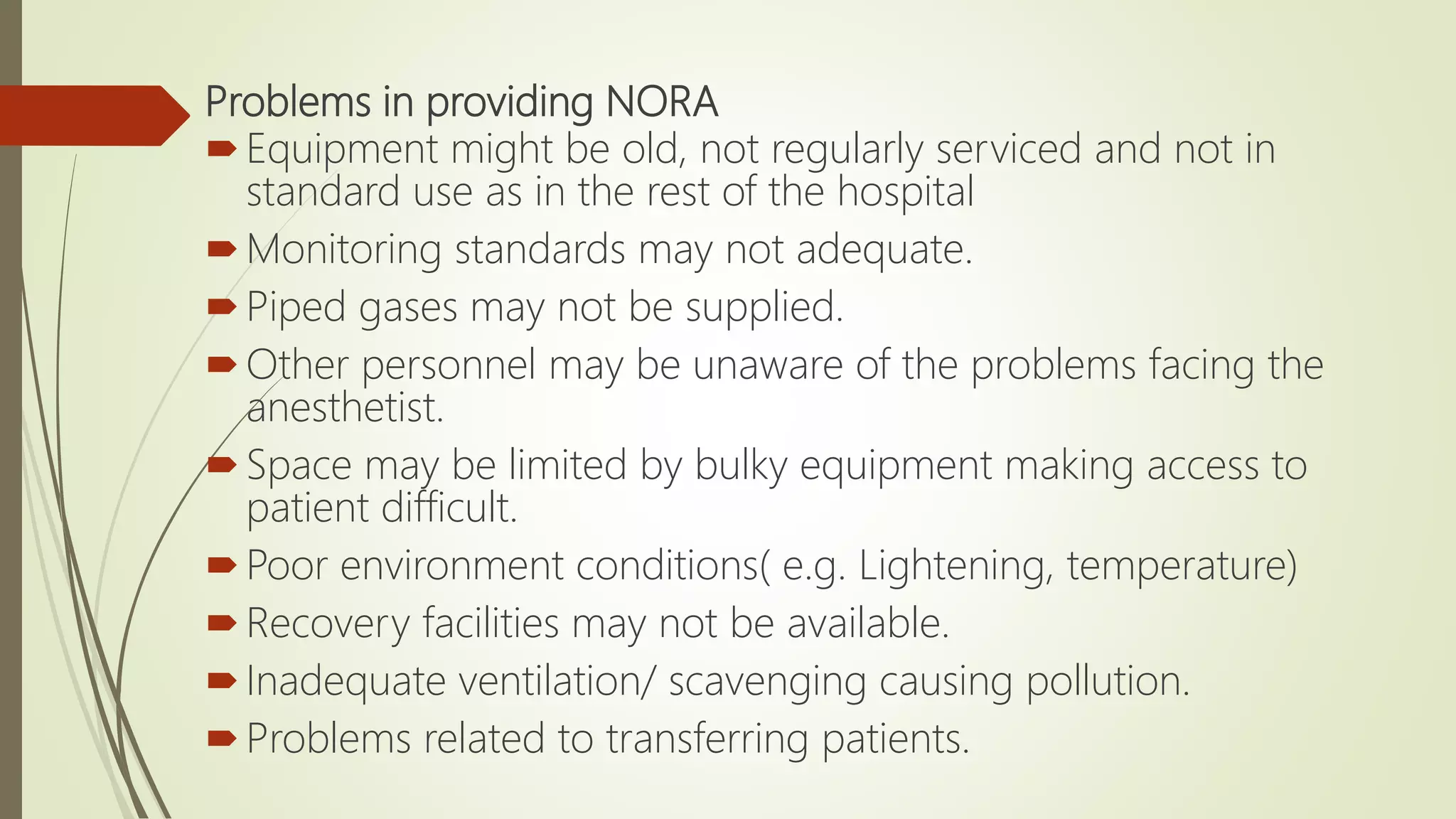
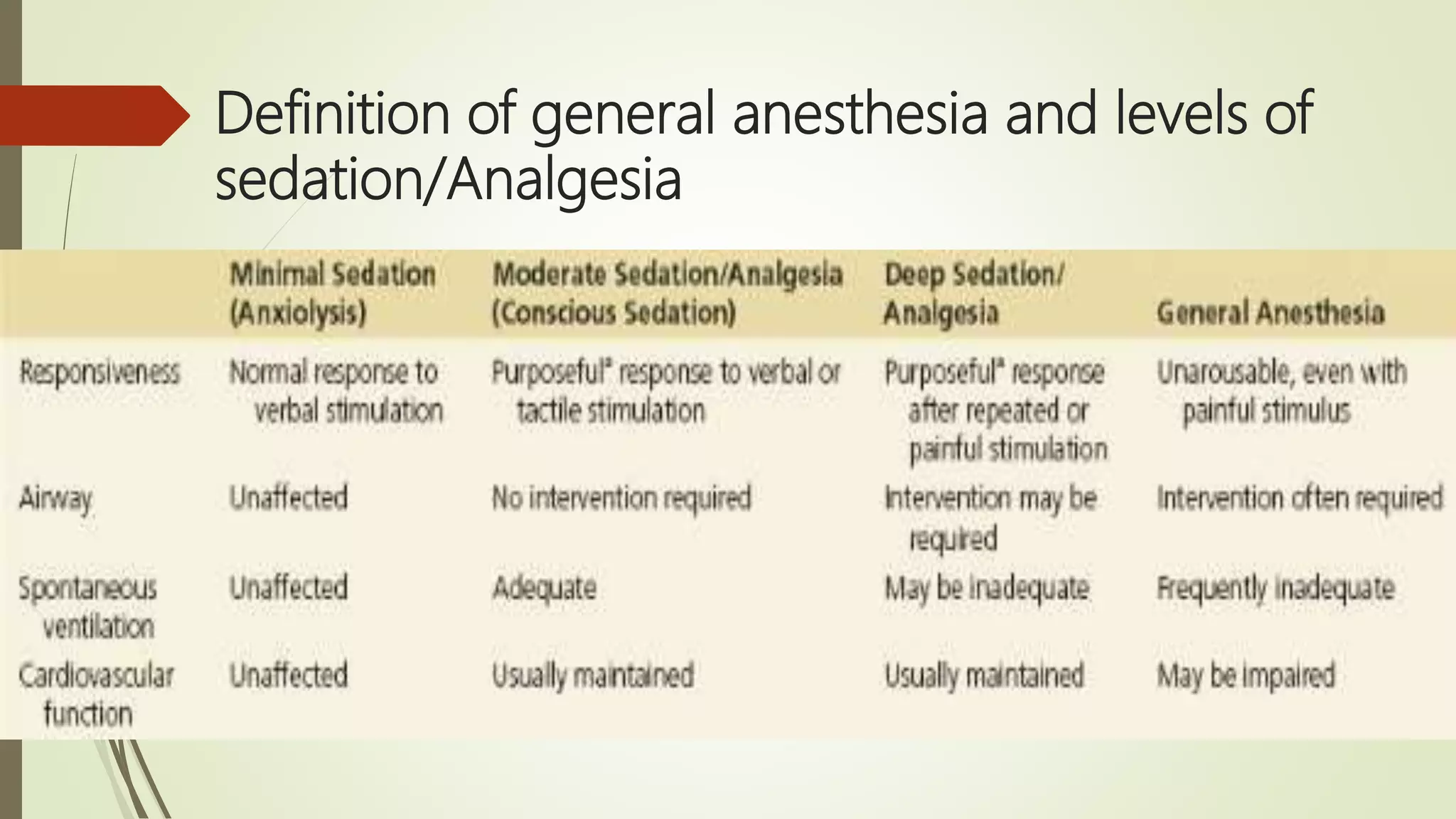
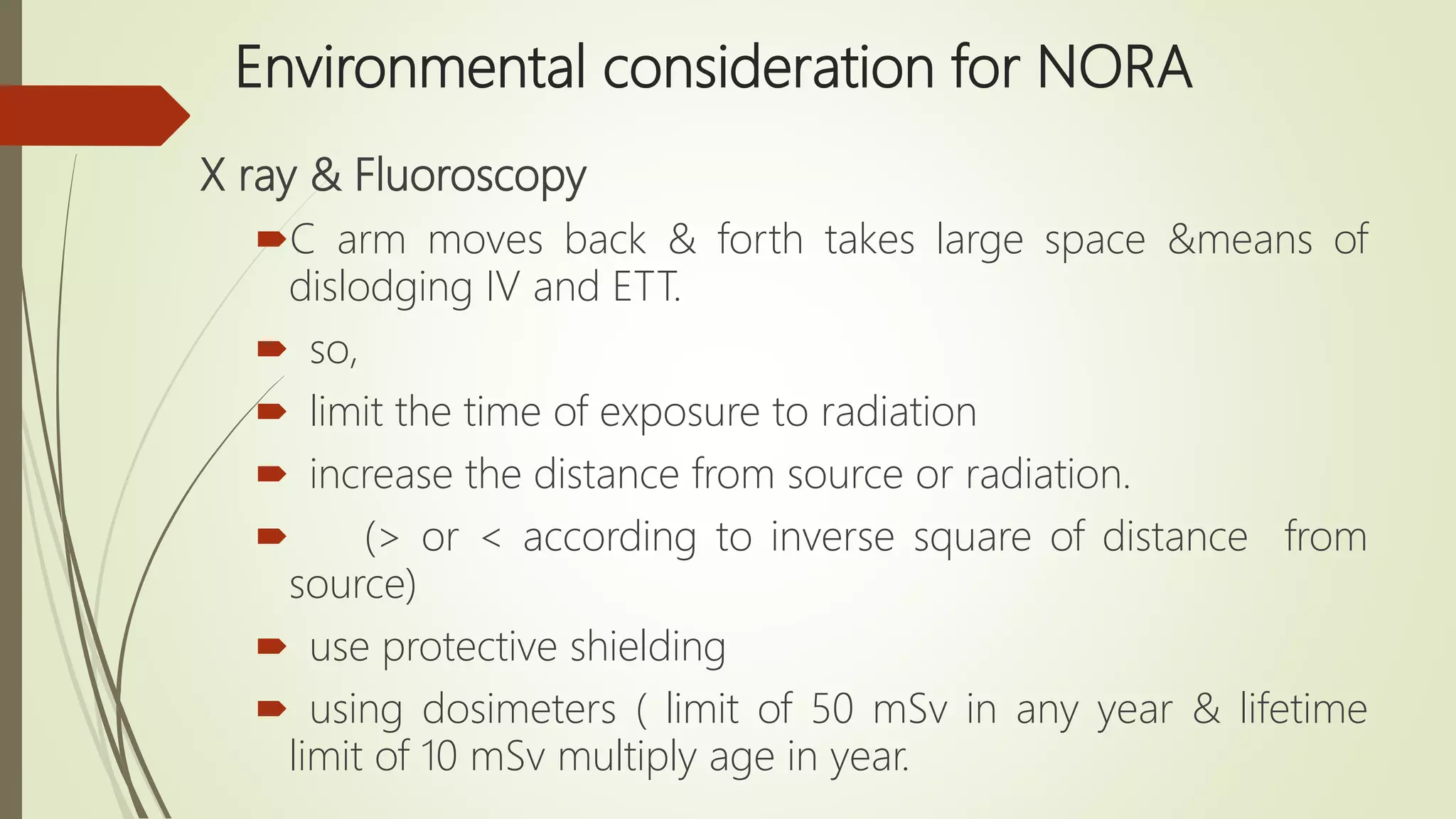
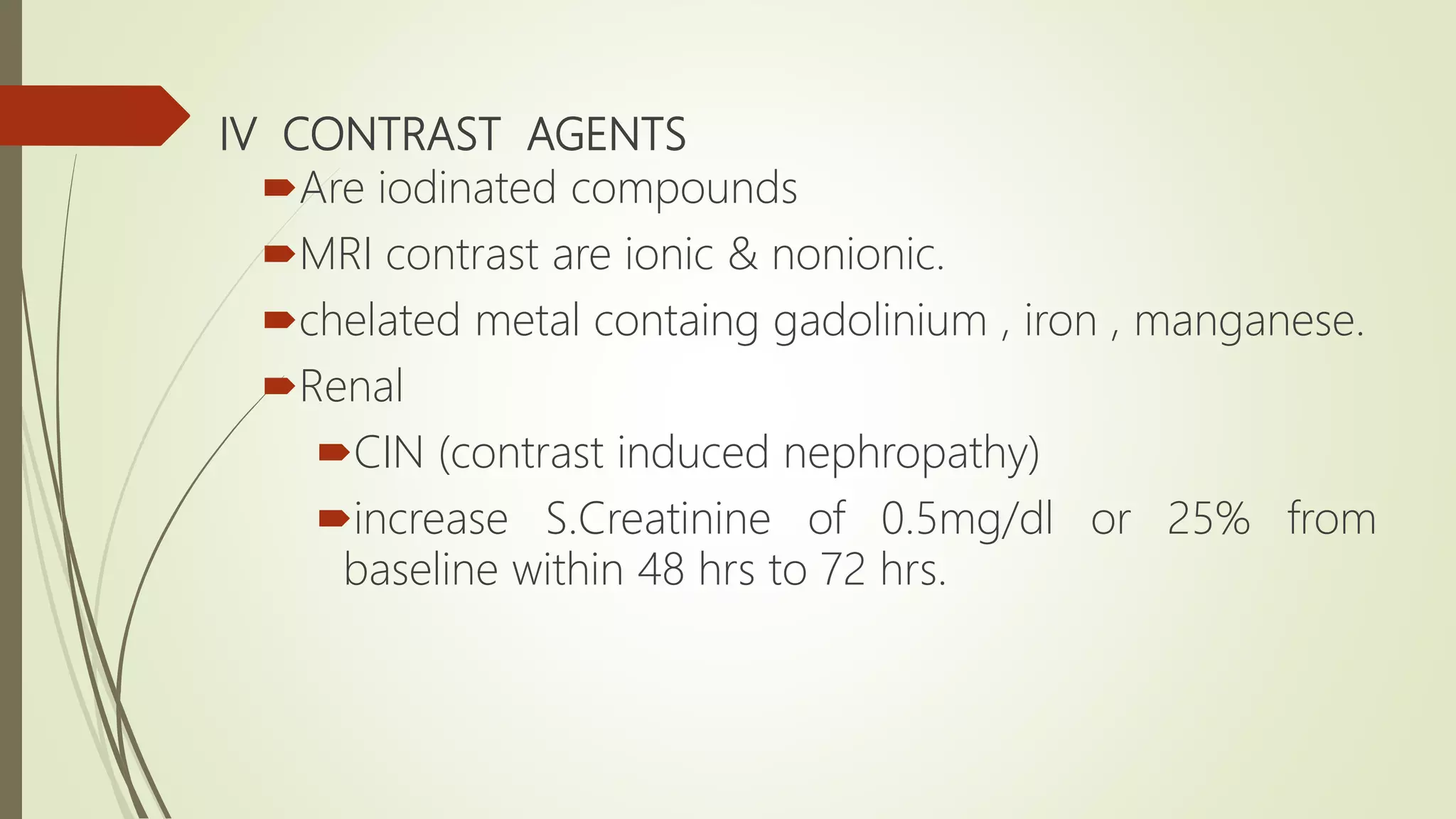
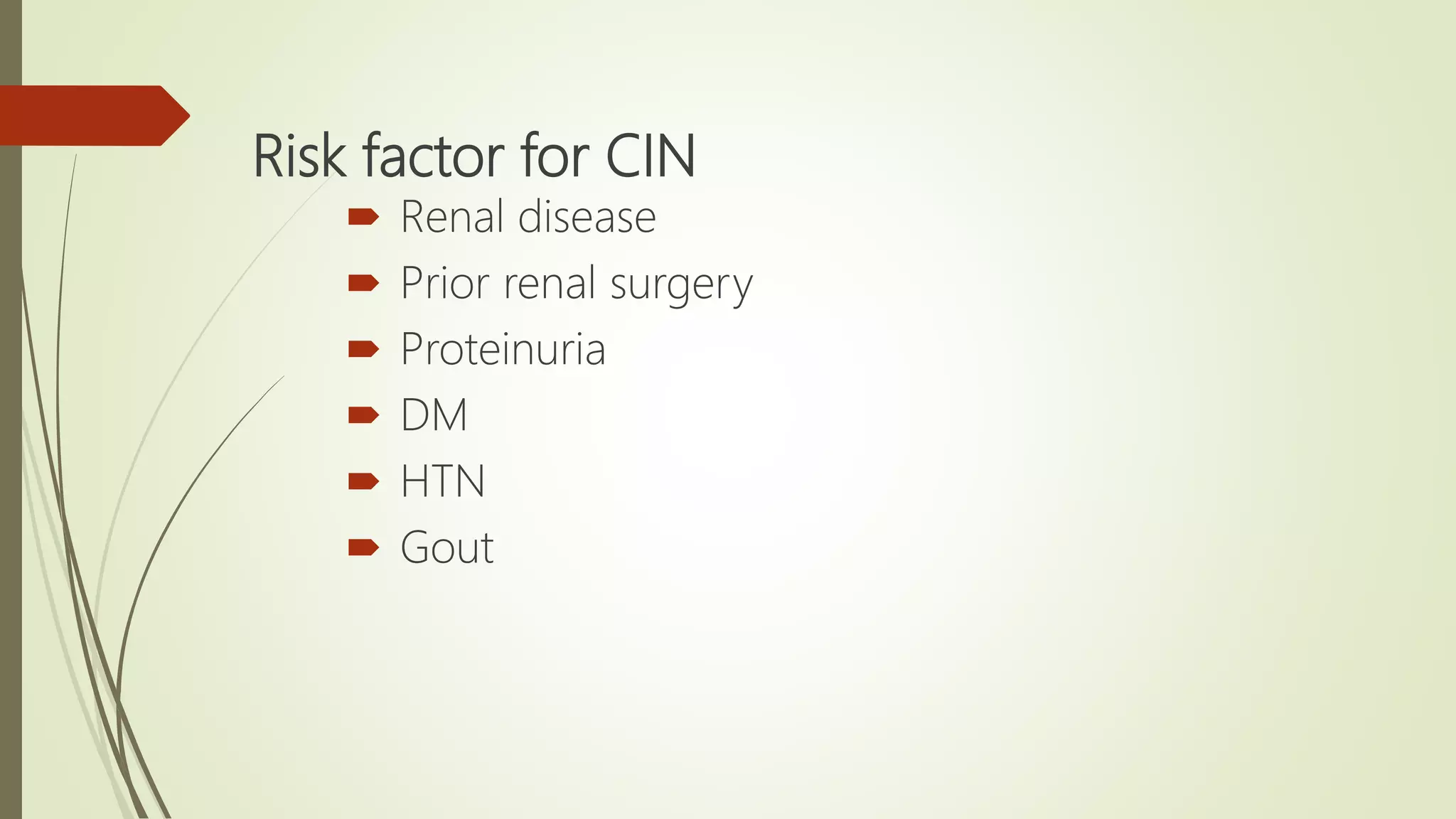
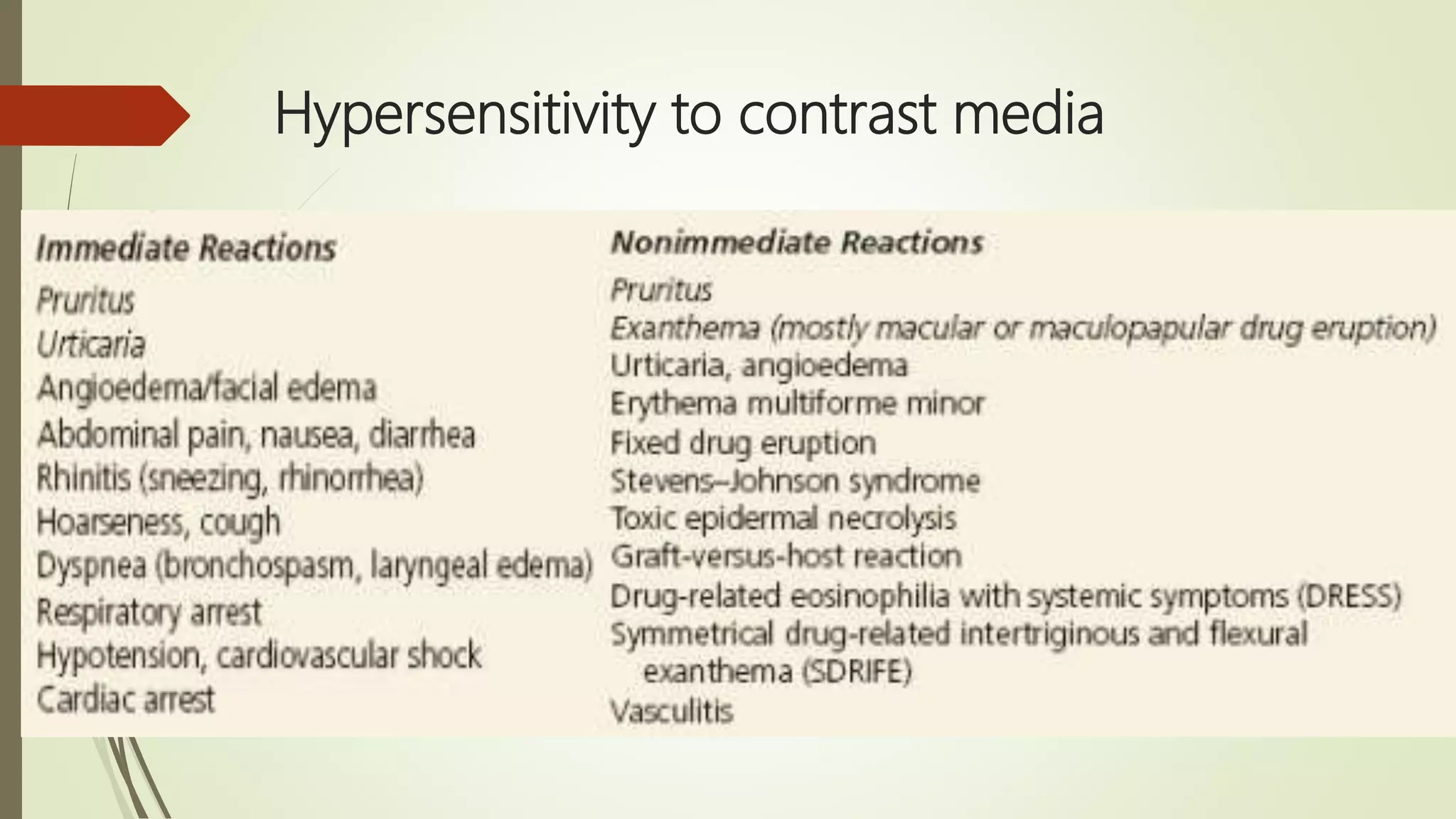
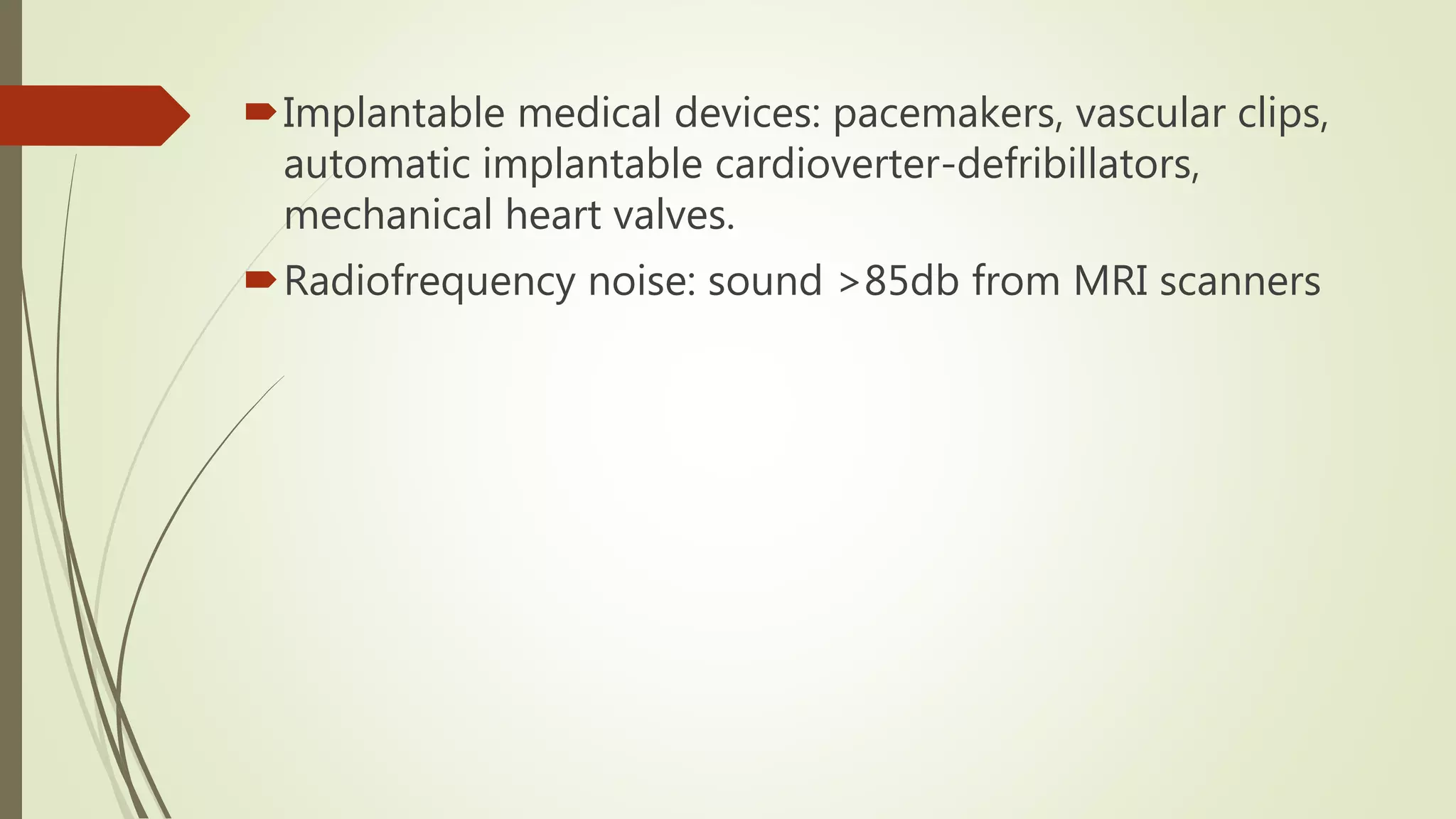
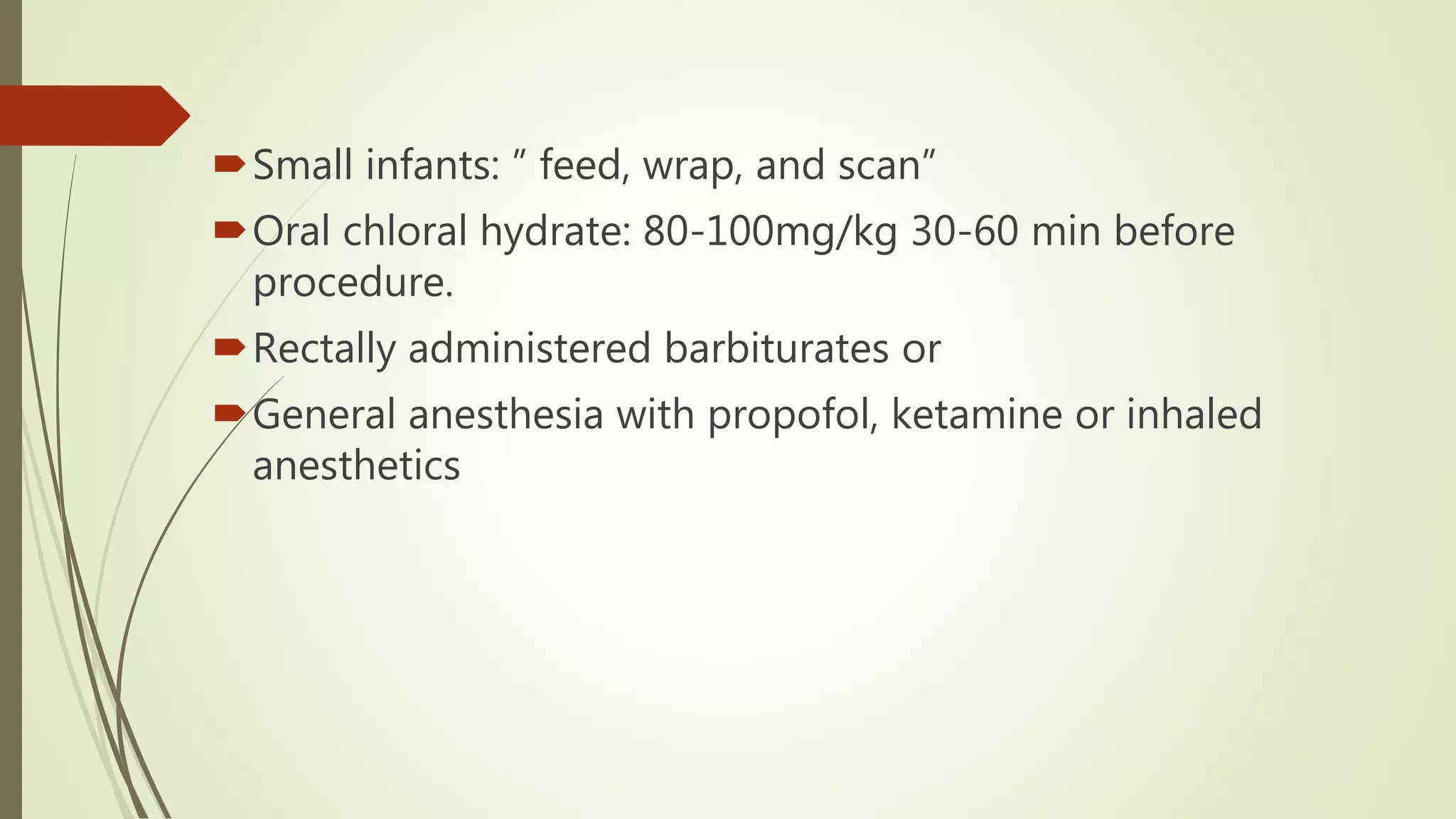
This document discusses non-operating room anesthesia (NORA). It begins by defining NORA as anesthesia provided outside the operating room, such as in radiology, endoscopy suites, MRI, and dental clinics. It then outlines a three step approach to NORA involving thorough patient assessment, appropriate monitoring and anesthesia care, and post-procedure management. Several ASA guidelines for equipment and facilities in NORA locations are also reviewed. Complications associated with NORA and special considerations for procedures like X-rays, MRIs, and IV contrast administration are discussed. The document emphasizes choosing anesthesia techniques based on patient factors and needs for each specific non-operating room procedure.