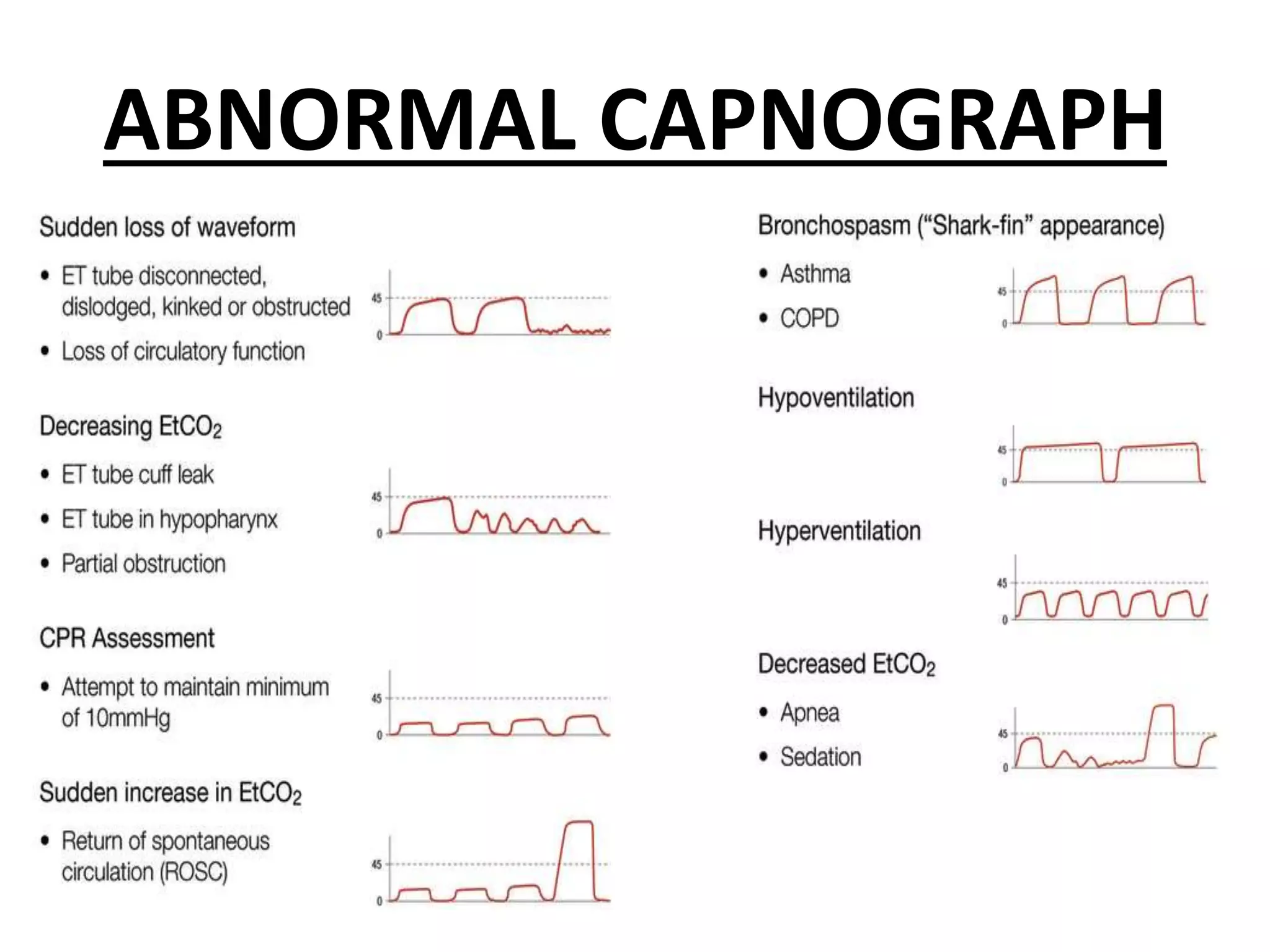
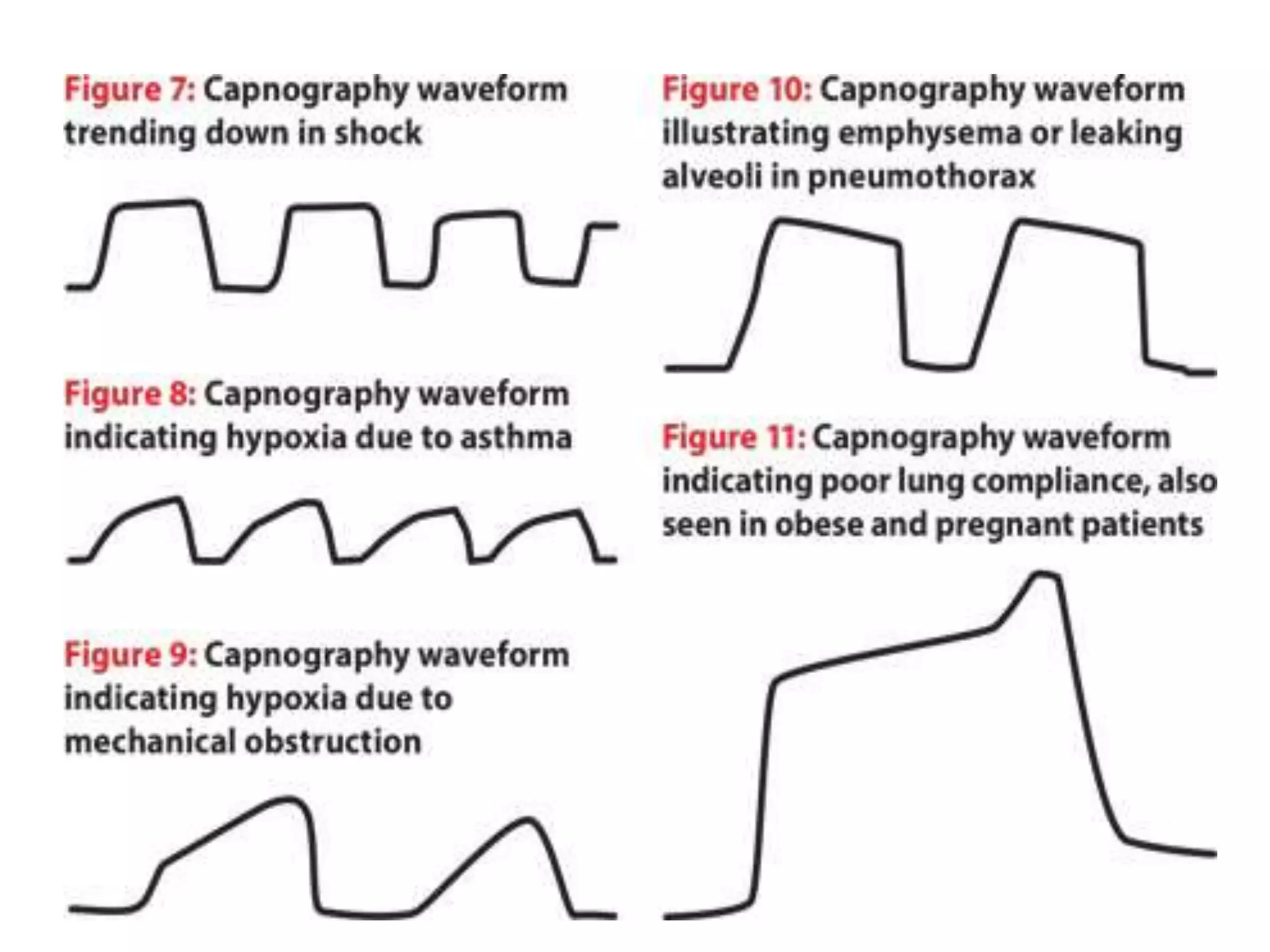
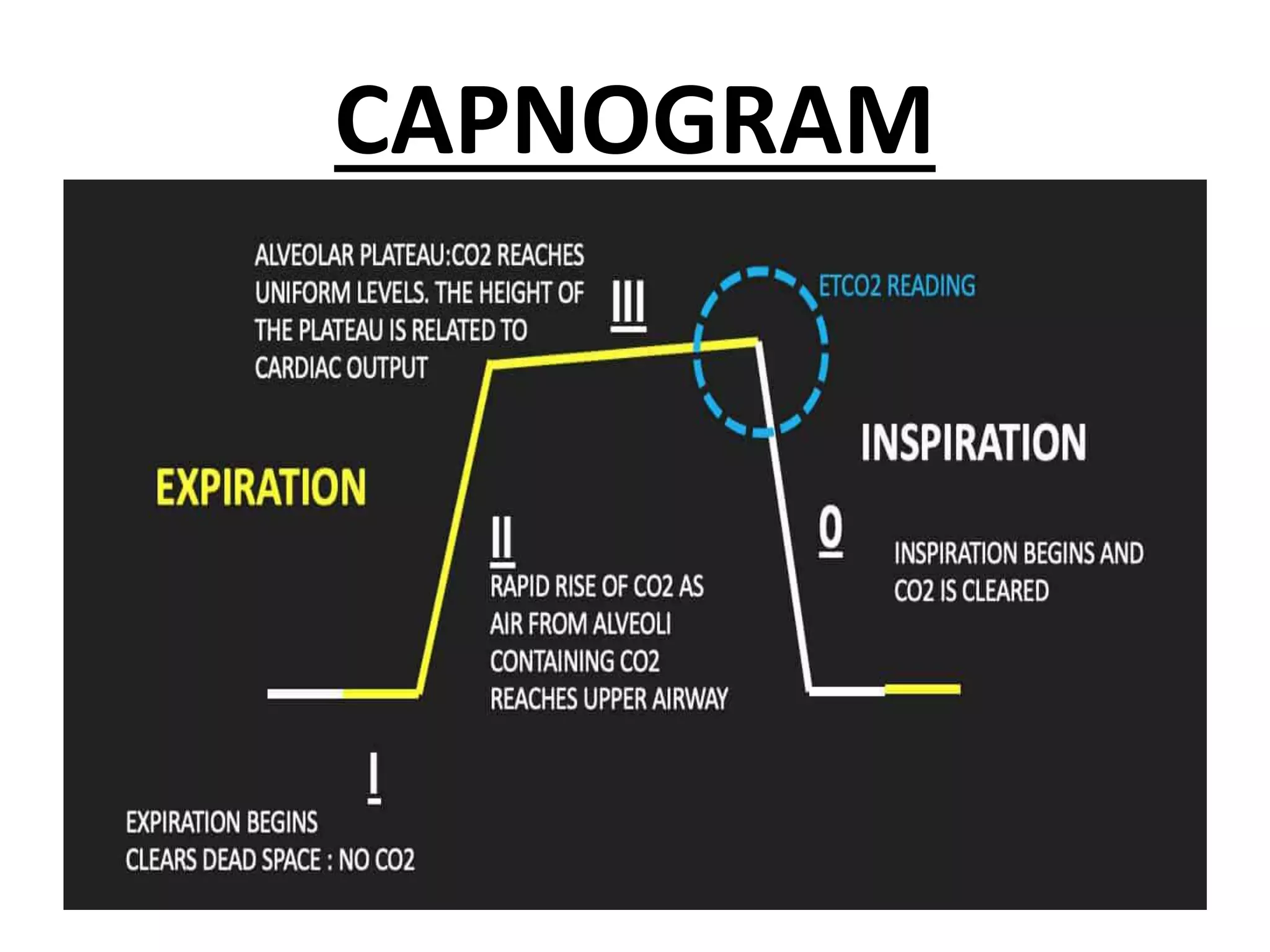
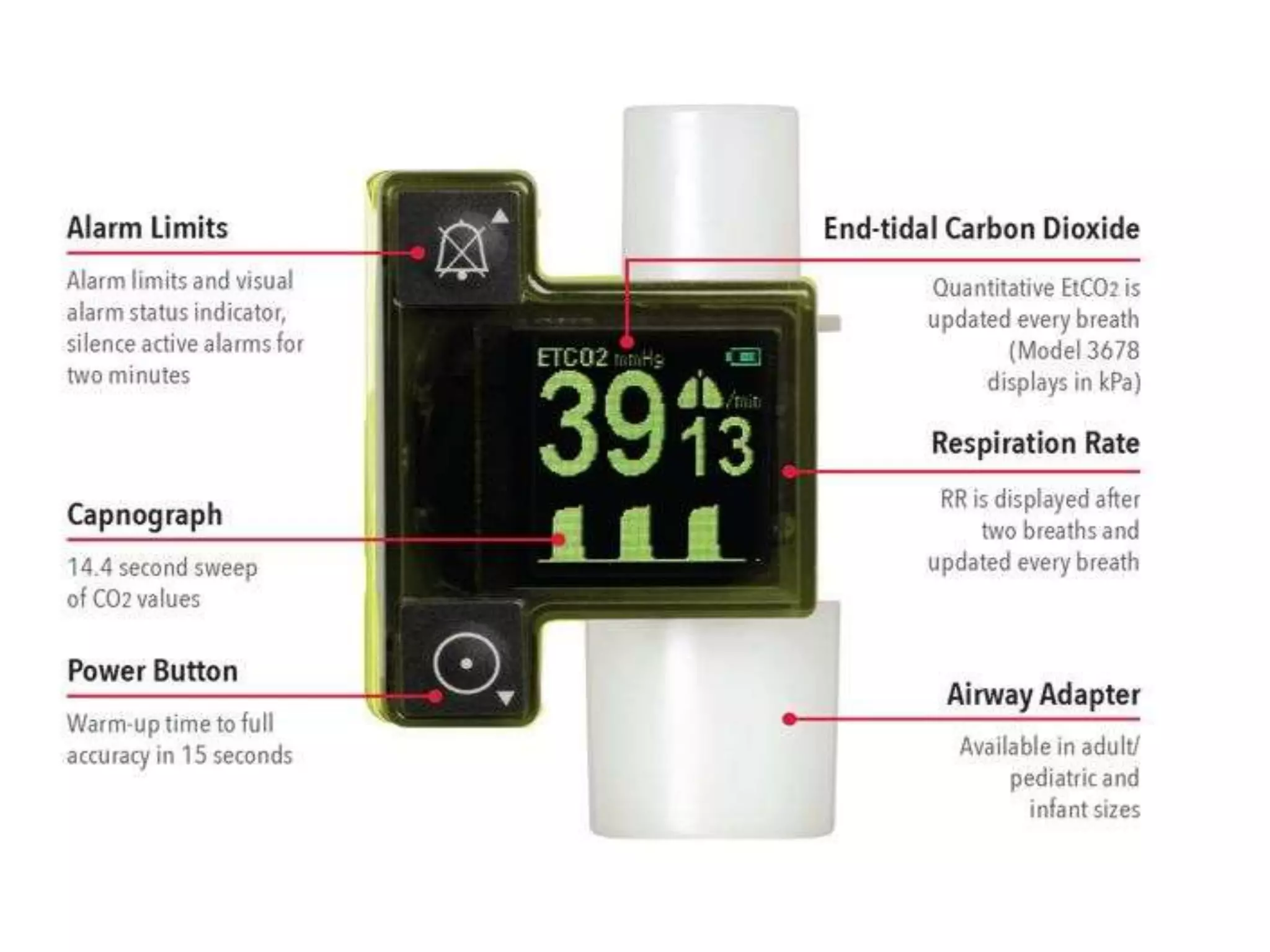
This document discusses capnography, which is the monitoring of carbon dioxide levels in exhaled breath. It can be used to assess ventilation, circulation, and metabolism during anesthesia and intensive care. The document defines capnography and describes the capnogram waveform and how it reflects respiratory parameters. Abnormal waveforms can indicate various lung diseases. Capnography is useful for confirming endotracheal tube placement and detecting malpositions. It provides advantages over pulse oximetry during procedures done under sedation. The principles of mainstream and sidestream capnography devices are outlined, as well as clinical applications in emergency medical services and indications for diagnostic usage.