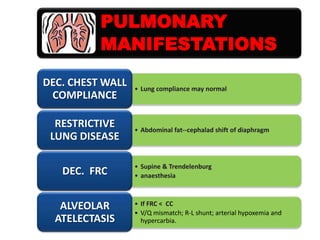
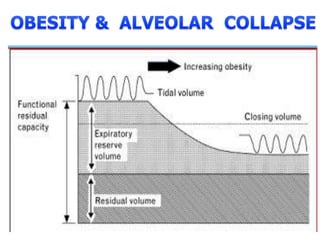
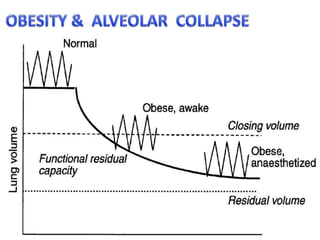
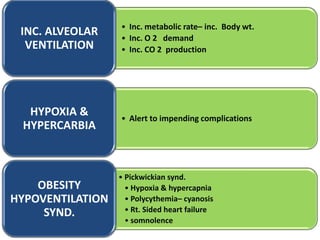
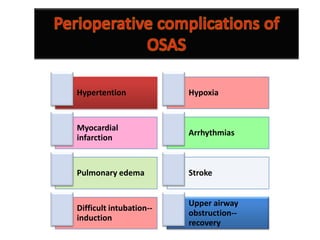
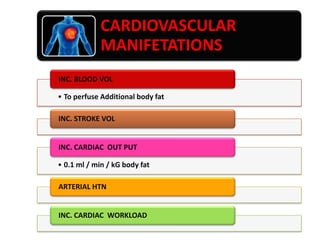
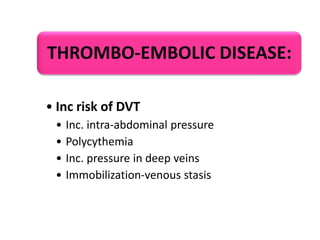
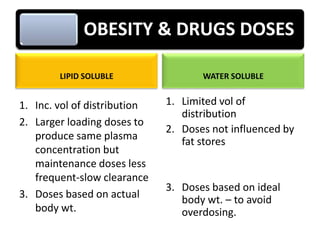
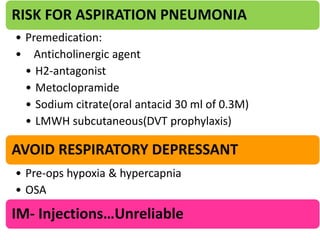
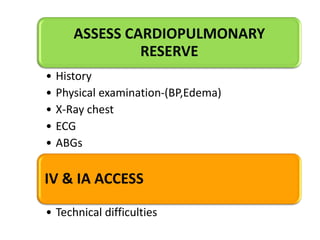
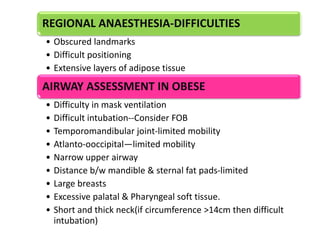
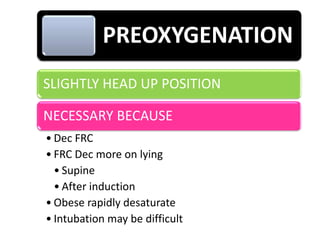
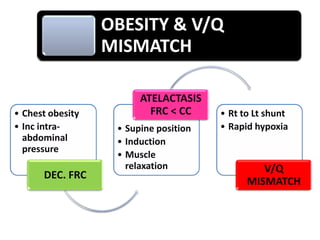
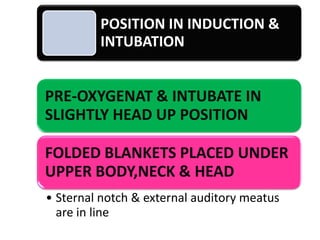
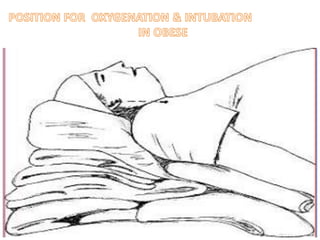
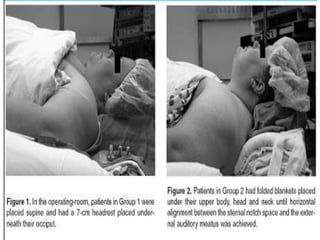
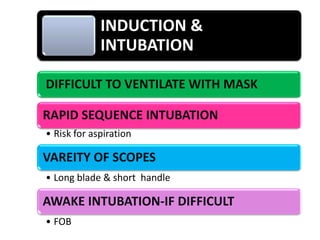
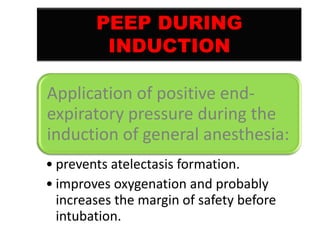
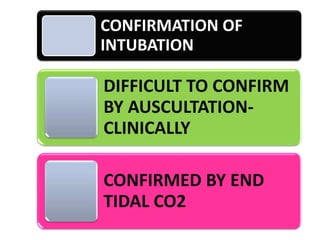
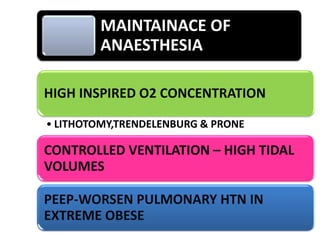
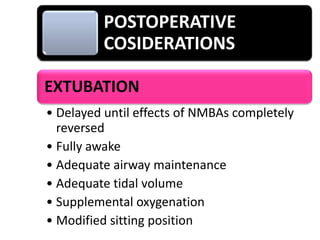
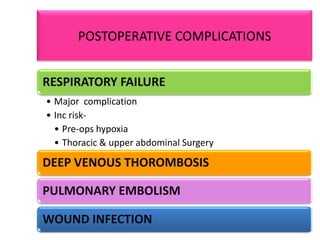
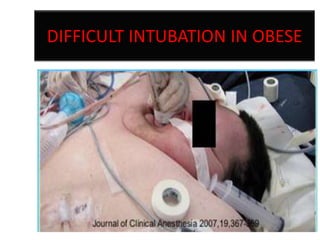
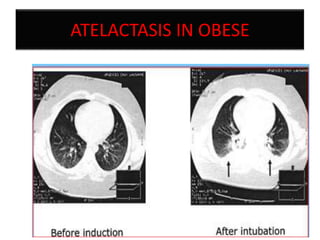
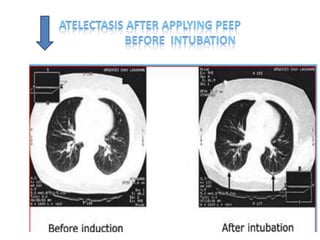
Obesity presents unique challenges for anaesthesia. Obese patients have decreased lung volumes which increases the risk of hypoxemia during induction and intubation. Preoxygenation in a slightly head-up position can help reduce this risk. Intubation may be difficult due to obesity related anatomical changes. Regional anaesthesia can also be challenging due to obscured landmarks and extensive adipose tissue. Postoperatively, obese patients are at higher risk of respiratory failure, DVT, and wound infections requiring close monitoring. Careful consideration of dosing, positioning, and postoperative monitoring is needed to safely manage anaesthesia for obese patients.