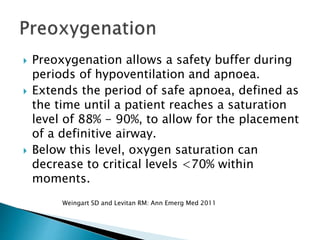
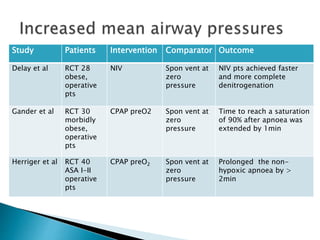
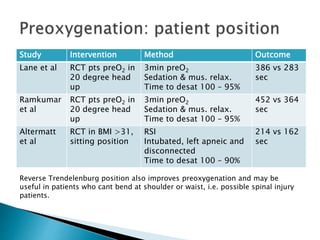
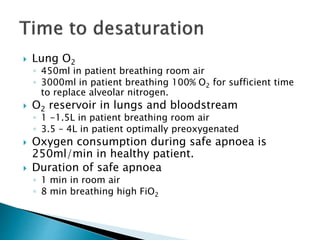
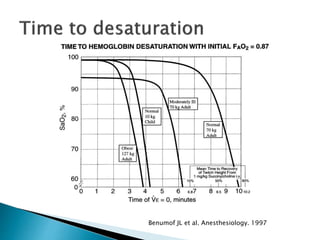
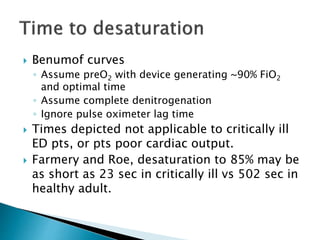
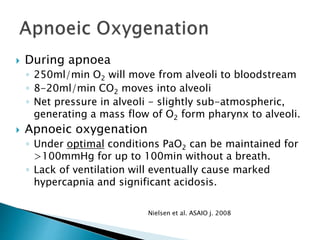
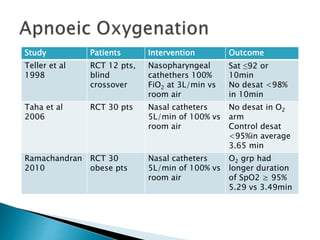
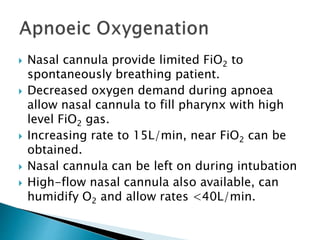
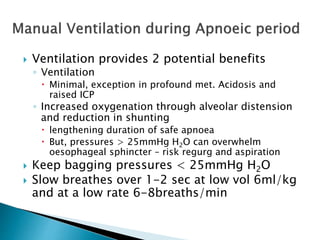
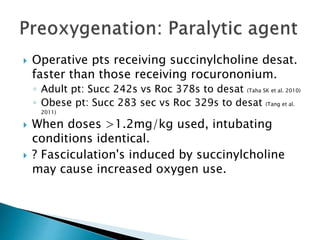
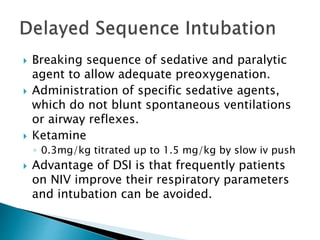
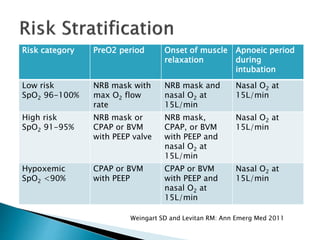
This document discusses strategies for optimizing preoxygenation prior to endotracheal intubation. It notes that conventional preoxygenation techniques provide safe intubation for most ED patients but that a subset may still desaturate. To safely intubate this higher risk group, the document recommends optimizing preoxygenation through techniques like non-invasive ventilation, apneic oxygenation through nasal cannula, positioning patients in a head-up position, and breaking the sequence of rapid sequence intubation administration. The goal is to prevent deoxygenation and extend the safe apneic period for patients undergoing endotracheal intubation.