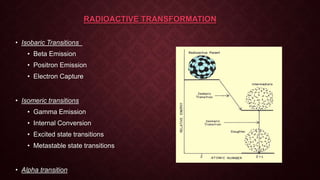
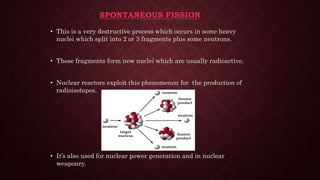
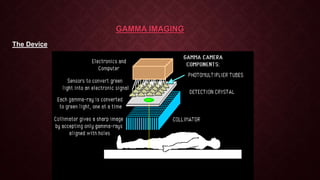
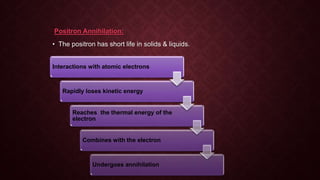
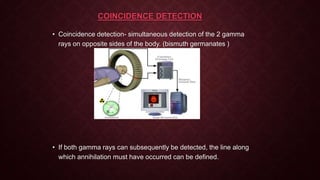
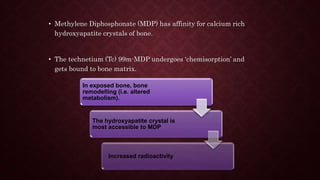
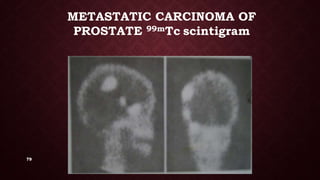
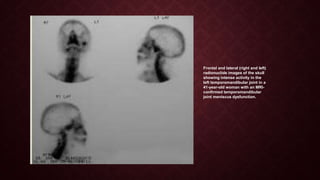
This document provides an overview of nuclear imaging and nuclear medicine. It discusses the basics of nuclear physics including radioactive decay modes like beta emission, positron emission, and gamma emission. It describes common medical isotopes used like technetium-99m, their ideal properties, production, and administration. The principles of nuclear medicine imaging are covered along with instrumentation and clinical applications for diagnosing diseases. Advantages include examining organ function while disadvantages include radiation exposure and limited anatomical detail.