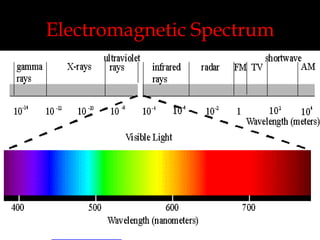
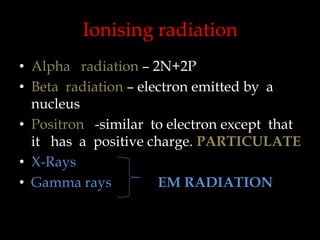
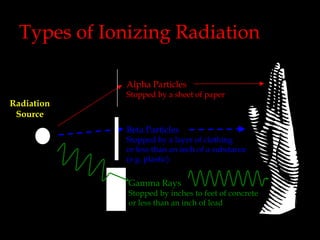
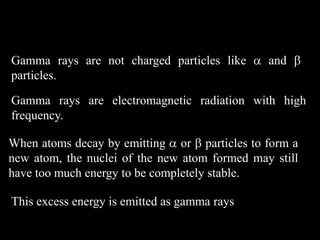
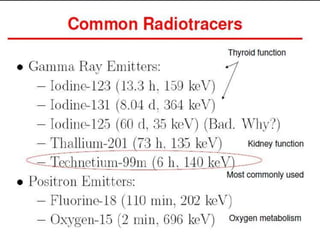
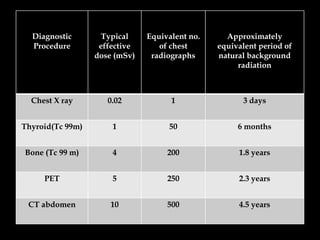
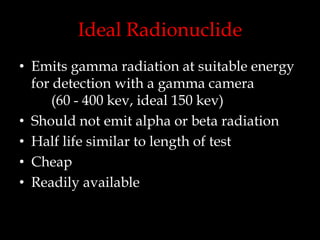
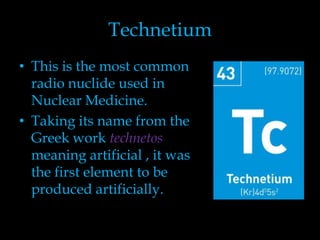
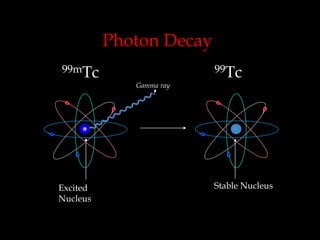
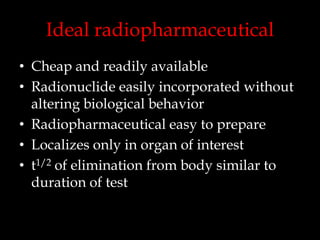
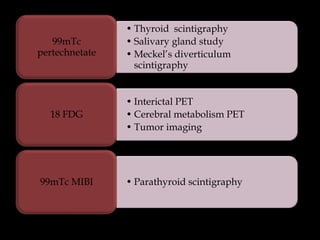
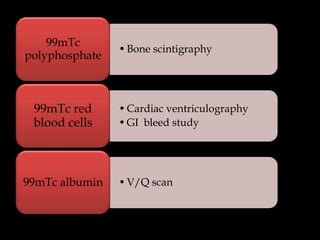
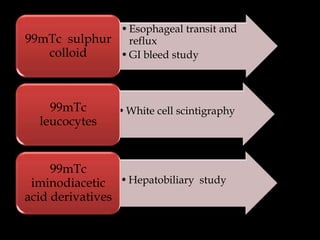
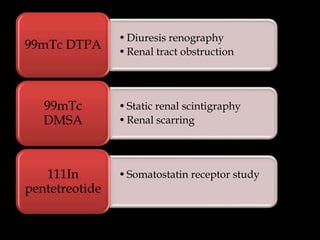
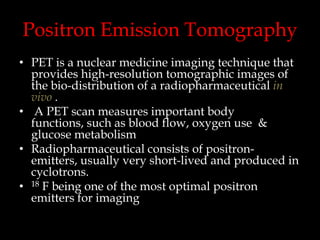
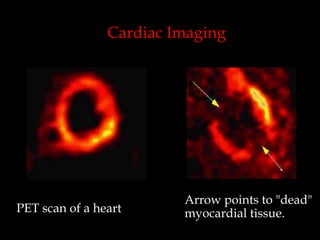
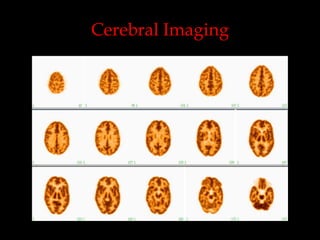
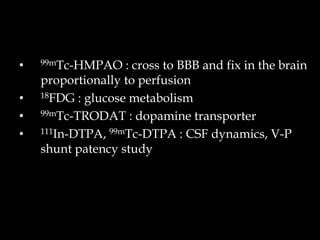
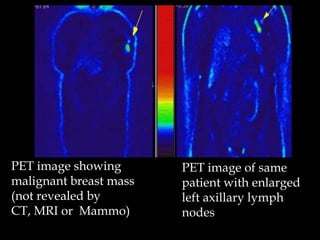
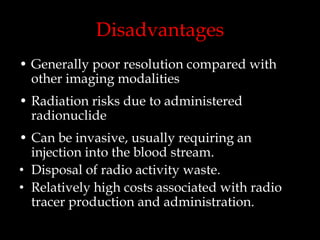
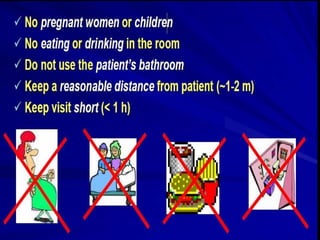
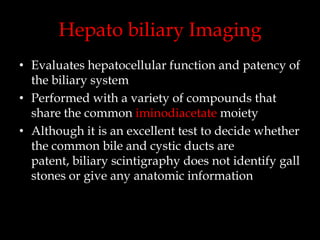
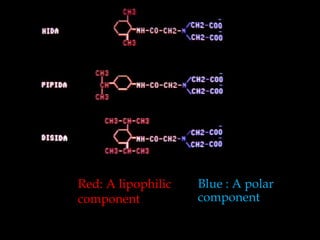
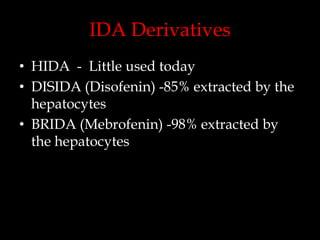
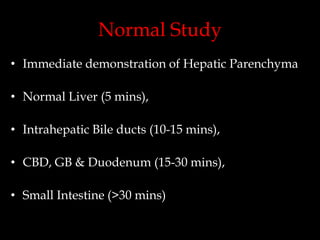
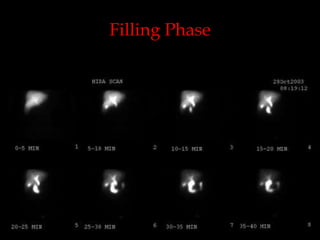
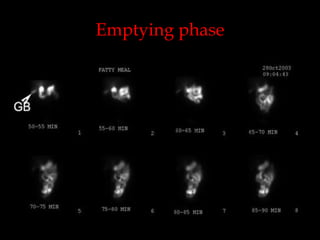
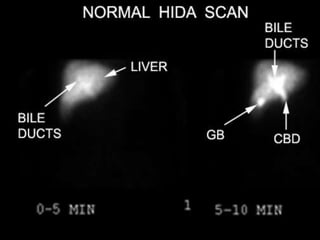
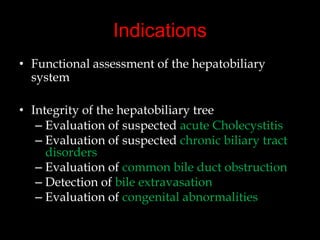
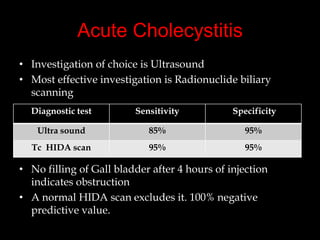
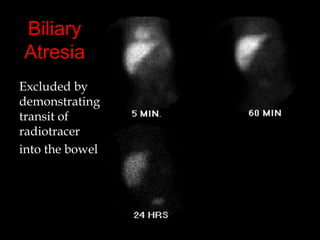
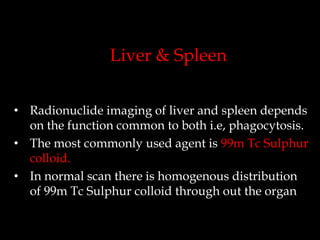
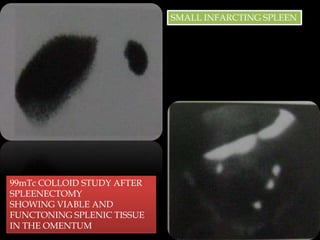
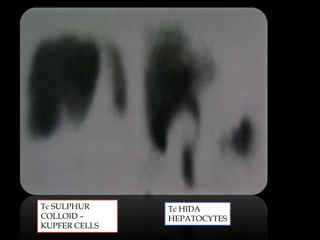
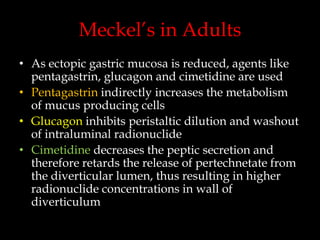
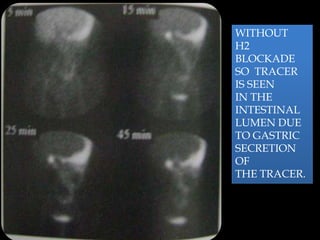
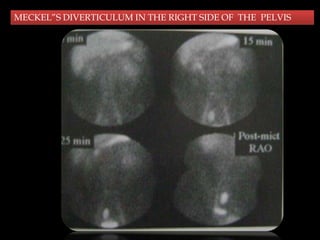
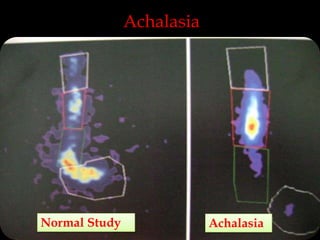
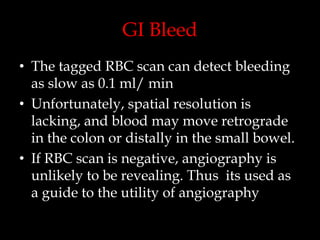
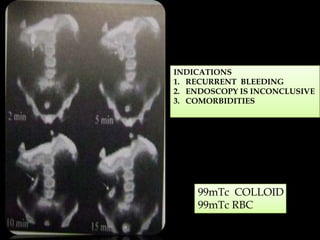
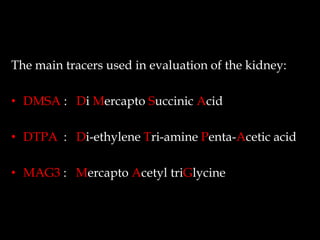
This document discusses various applications of radionuclide imaging. It begins with an overview of types of ionizing radiation and how different radionuclides are used in nuclear medicine. Examples are given of specific radiotracers used in cardiac, cerebral, and oncologic imaging. The document then focuses on applications of nuclear medicine in evaluating the gastrointestinal system and hepatobiliary system, including imaging of the liver, spleen, and detection of Meckel's diverticulum and gastrointestinal bleeding. Safety considerations of radiotracer administration are also reviewed.