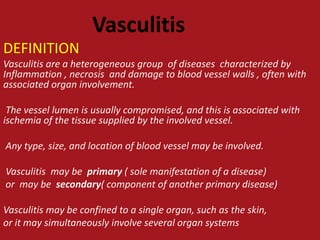
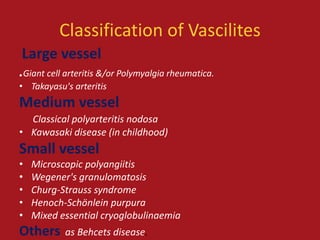
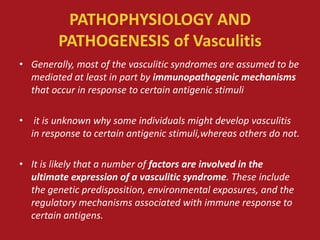
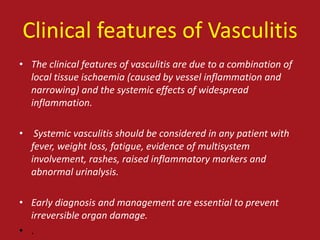
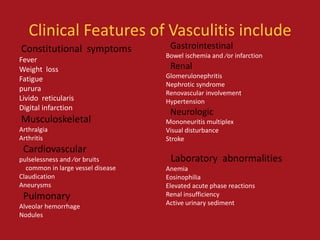
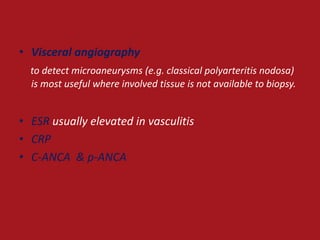
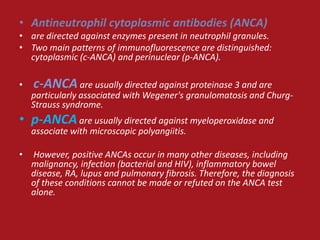
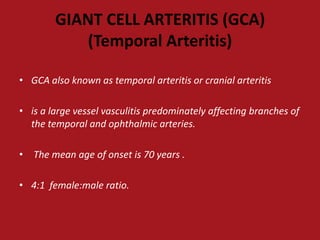
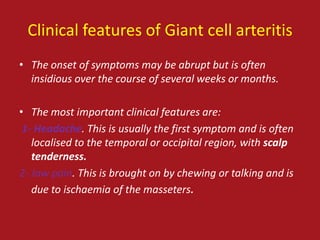
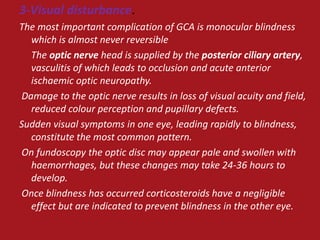
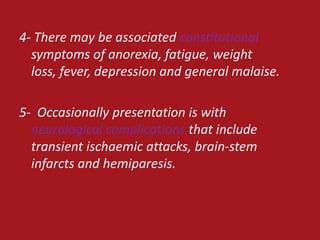
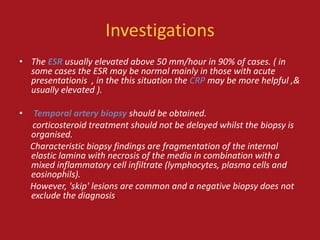
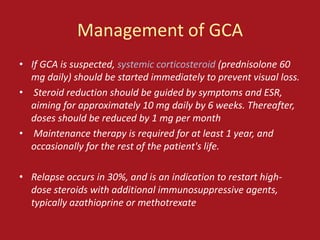
Vasculitis refers to a group of diseases characterized by inflammation of blood vessels. The document defines and classifies different types of vasculitis based on vessel size. It discusses the pathophysiology, clinical features, investigations and management of vasculitis. Giant cell arteritis is provided as an example of large vessel vasculitis that predominantly affects branches of the temporal and ophthalmic arteries in older individuals, with headaches, jaw pain and risk of vision loss as key clinical features.