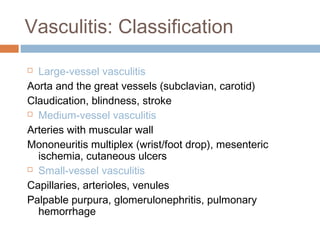
This document discusses vasculitis, which is inflammation of blood vessels. It defines vasculitis and describes the different types including large vessel, medium vessel, and small vessel vasculitis. Specific conditions are discussed such as giant cell arteritis, granulomatosis with polyangiitis, Churg-Strauss syndrome, Behcet's disease, thromboangiitis obliterans, and infectious vasculitis. The pathology, clinical features, morphology, and treatment of some of these conditions are summarized. Images are also included showing histological features.