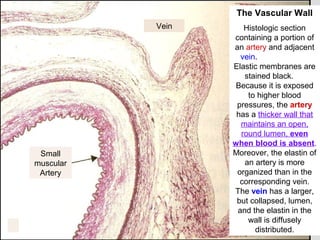
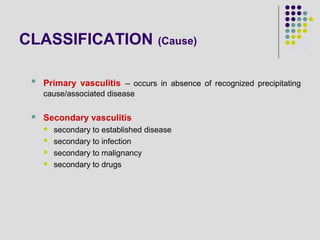
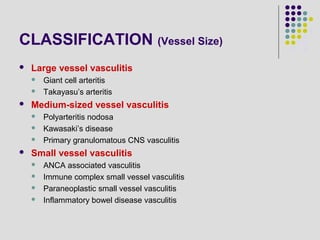
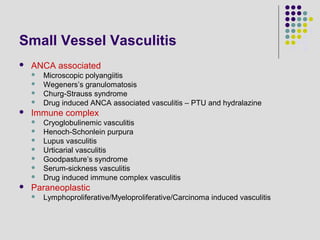
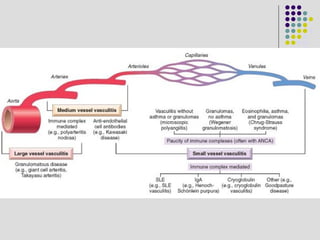
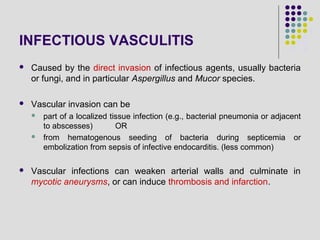
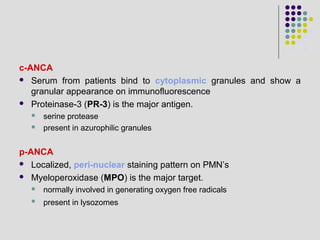
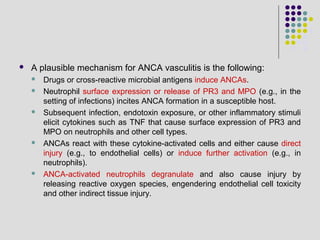
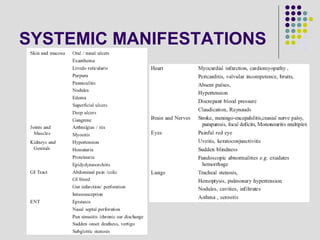
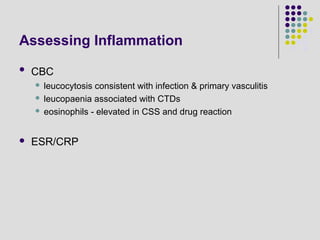
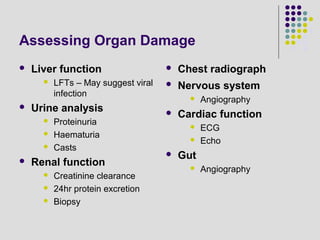
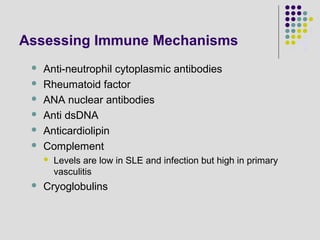
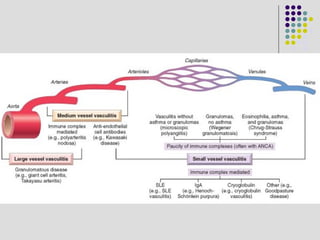
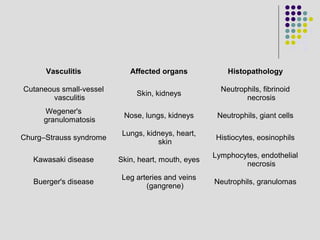
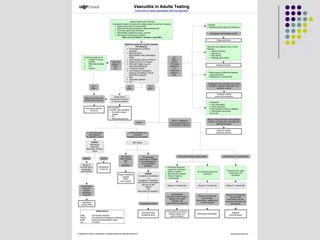
Vasculitis refers to inflammation of blood vessels. The document discusses the classification, pathogenesis, clinical manifestations, investigations, and histopathology of various types of vasculitis. It classifies vasculitis based on vessel size (large, medium, small vessel) and cause (primary, secondary to infection, drugs, etc). Pathogenesis may involve infectious or non-infectious mechanisms like immune complex deposition, ANCA, or anti-endothelial cell antibodies. Investigations assess organ damage, immune mechanisms, and provide tissue diagnosis. Clinical features and histopathology vary depending on the type and organs involved in the vasculitis.