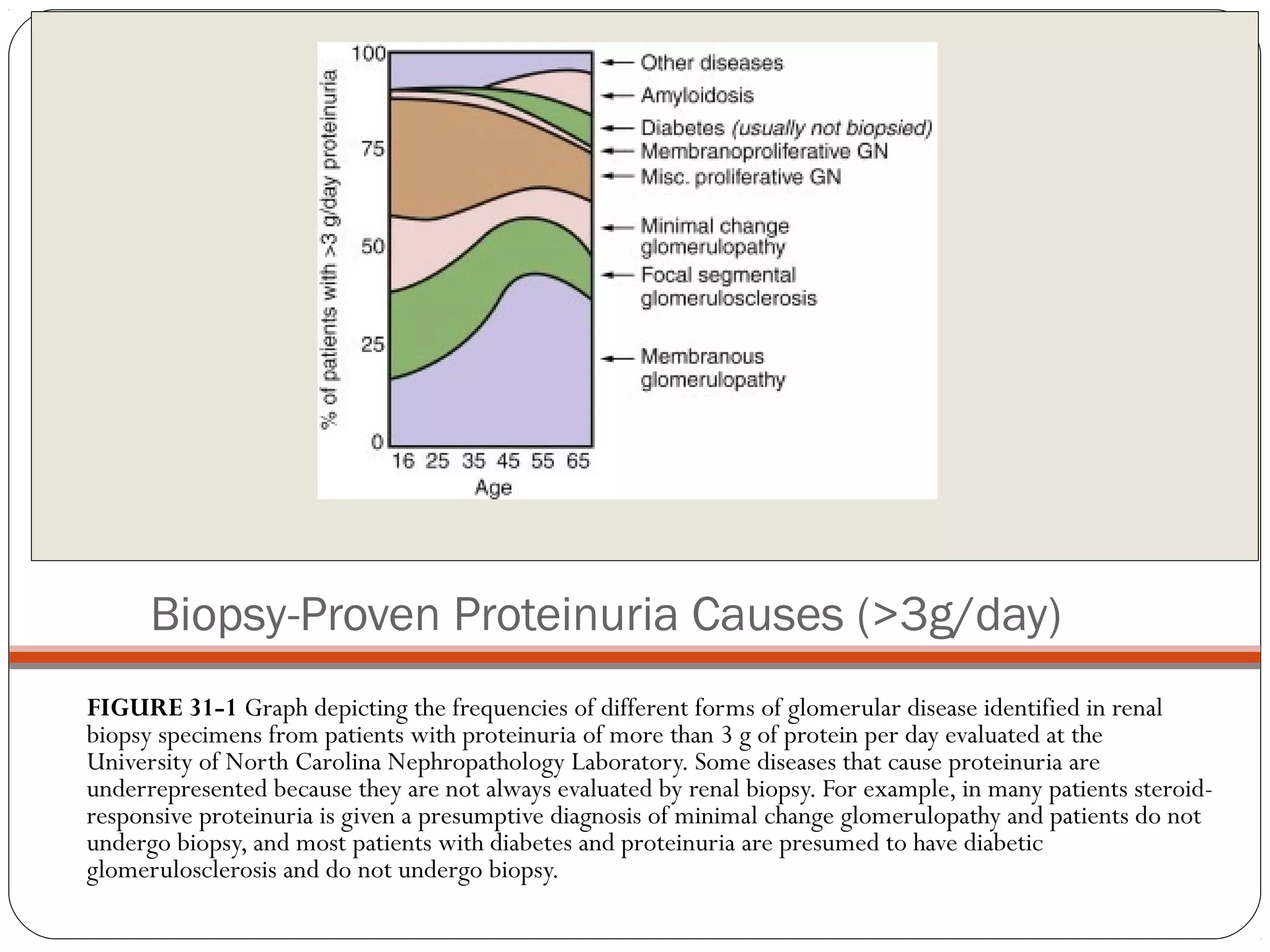
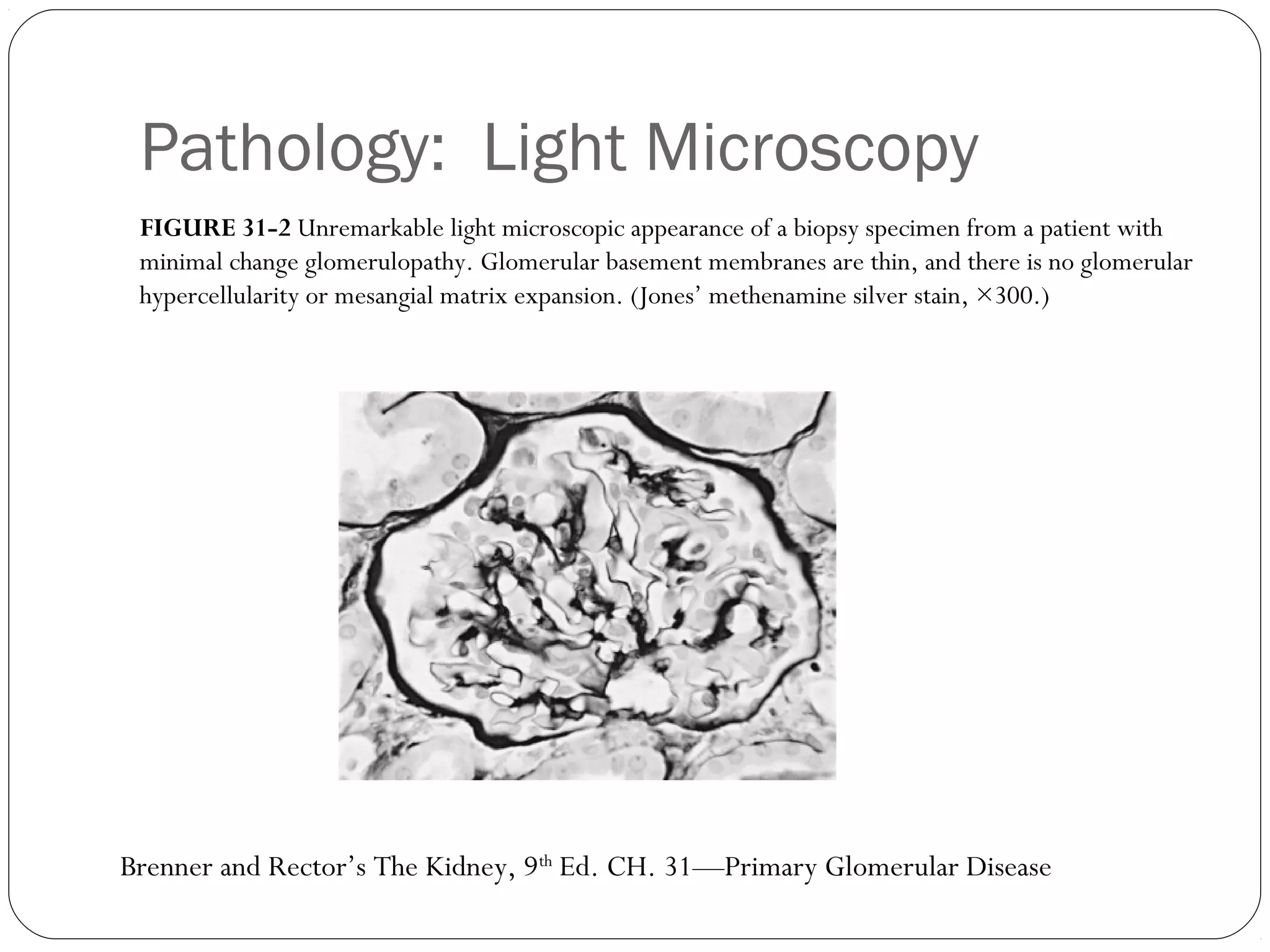
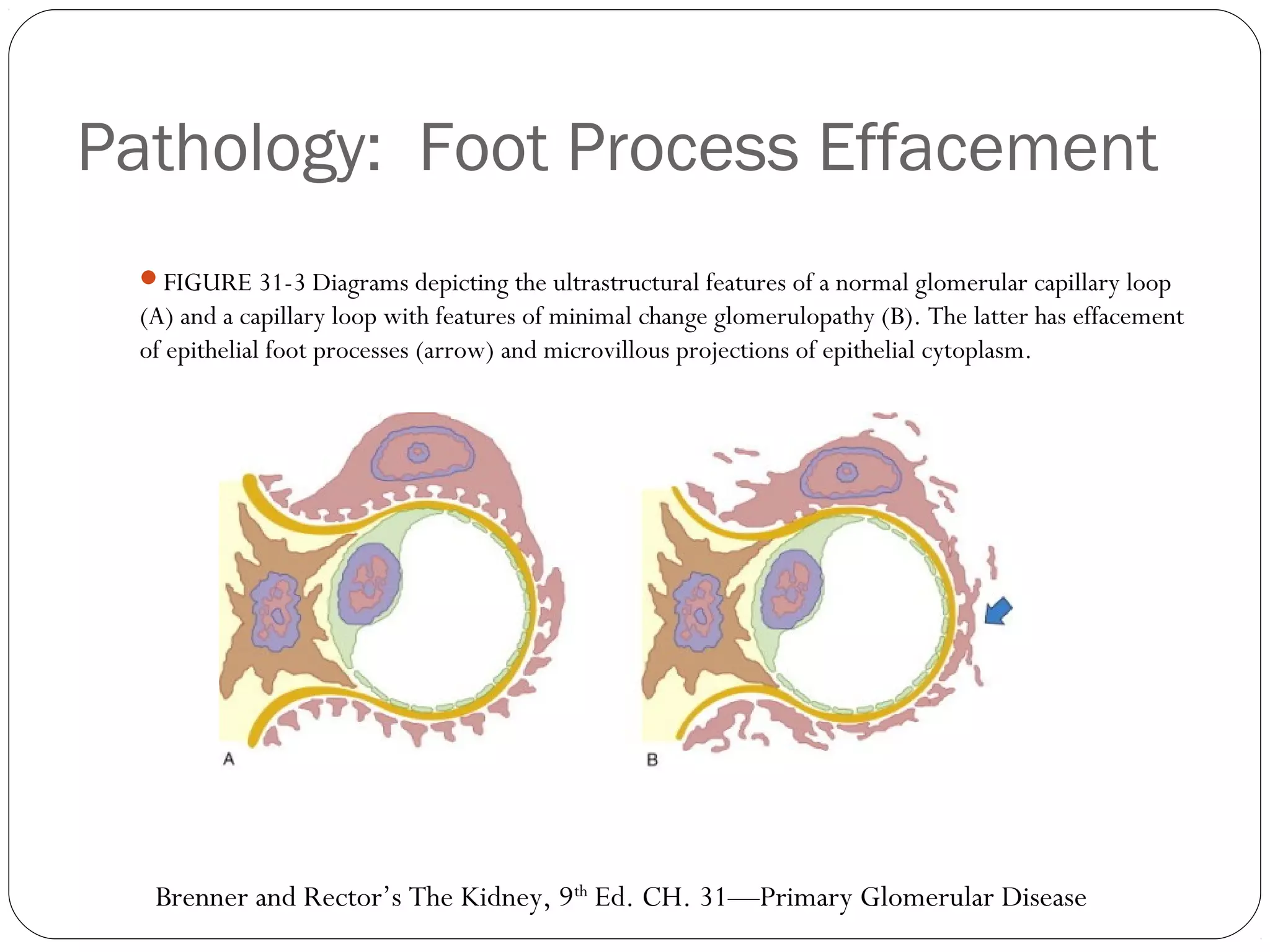
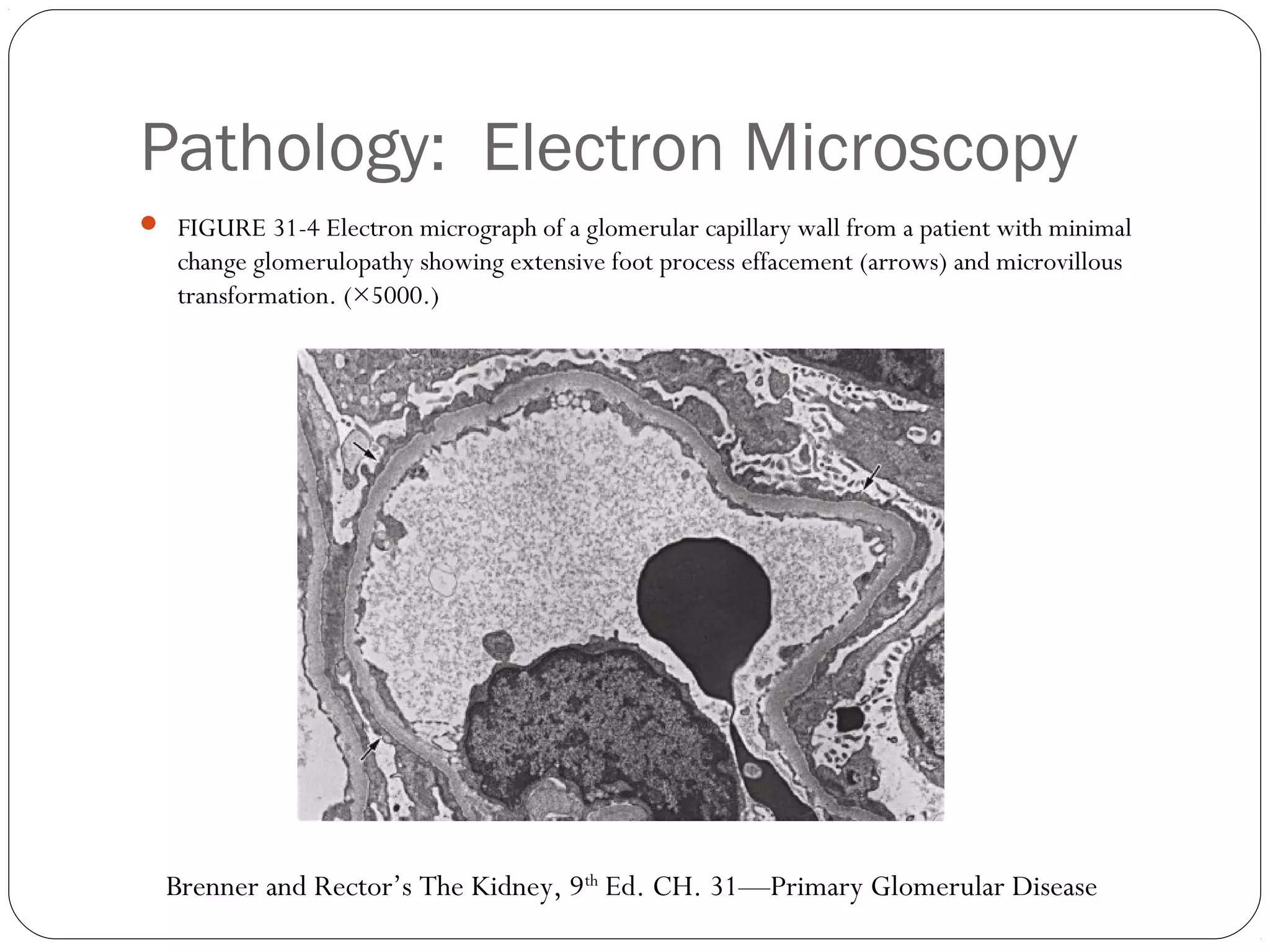
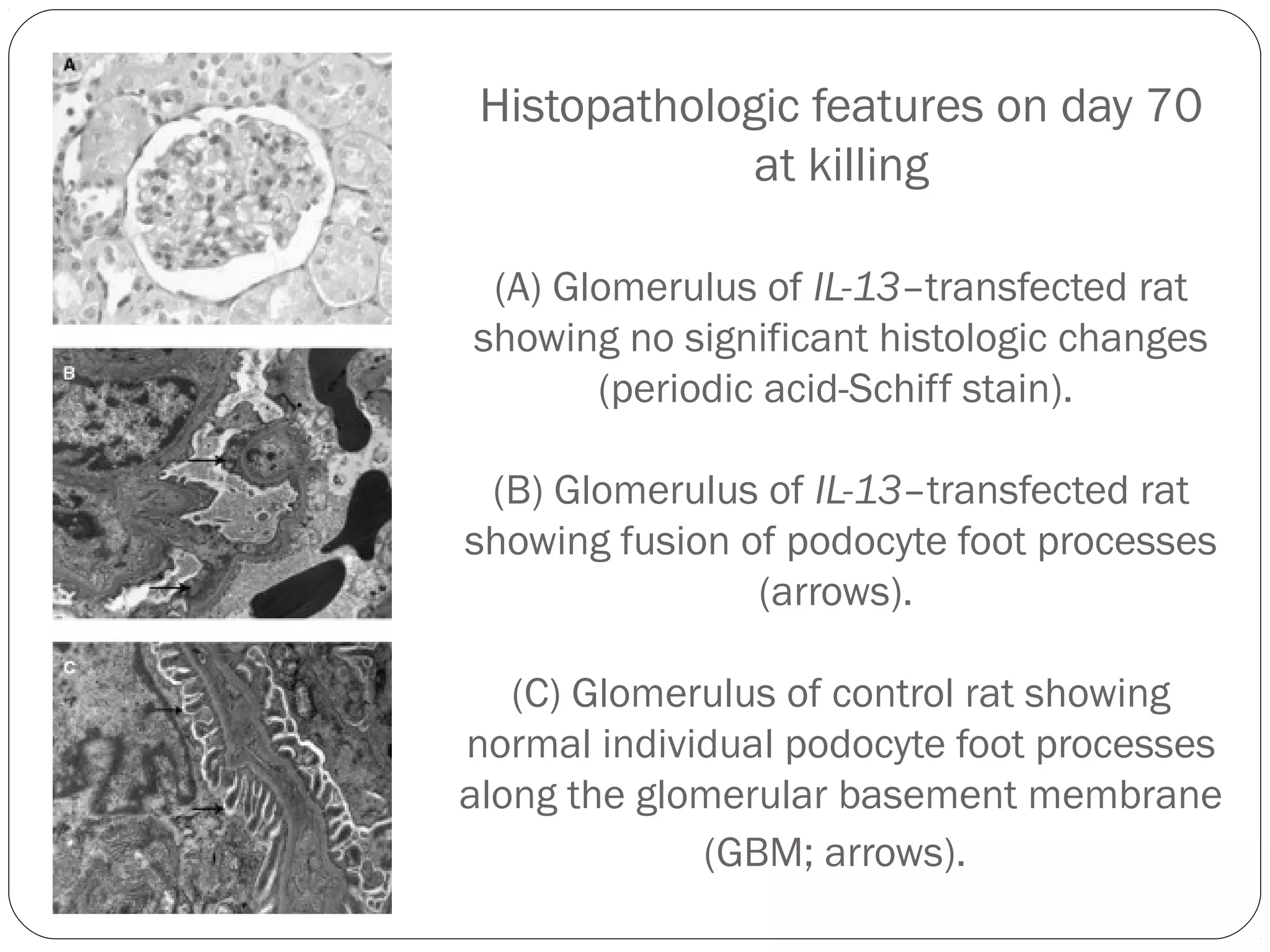
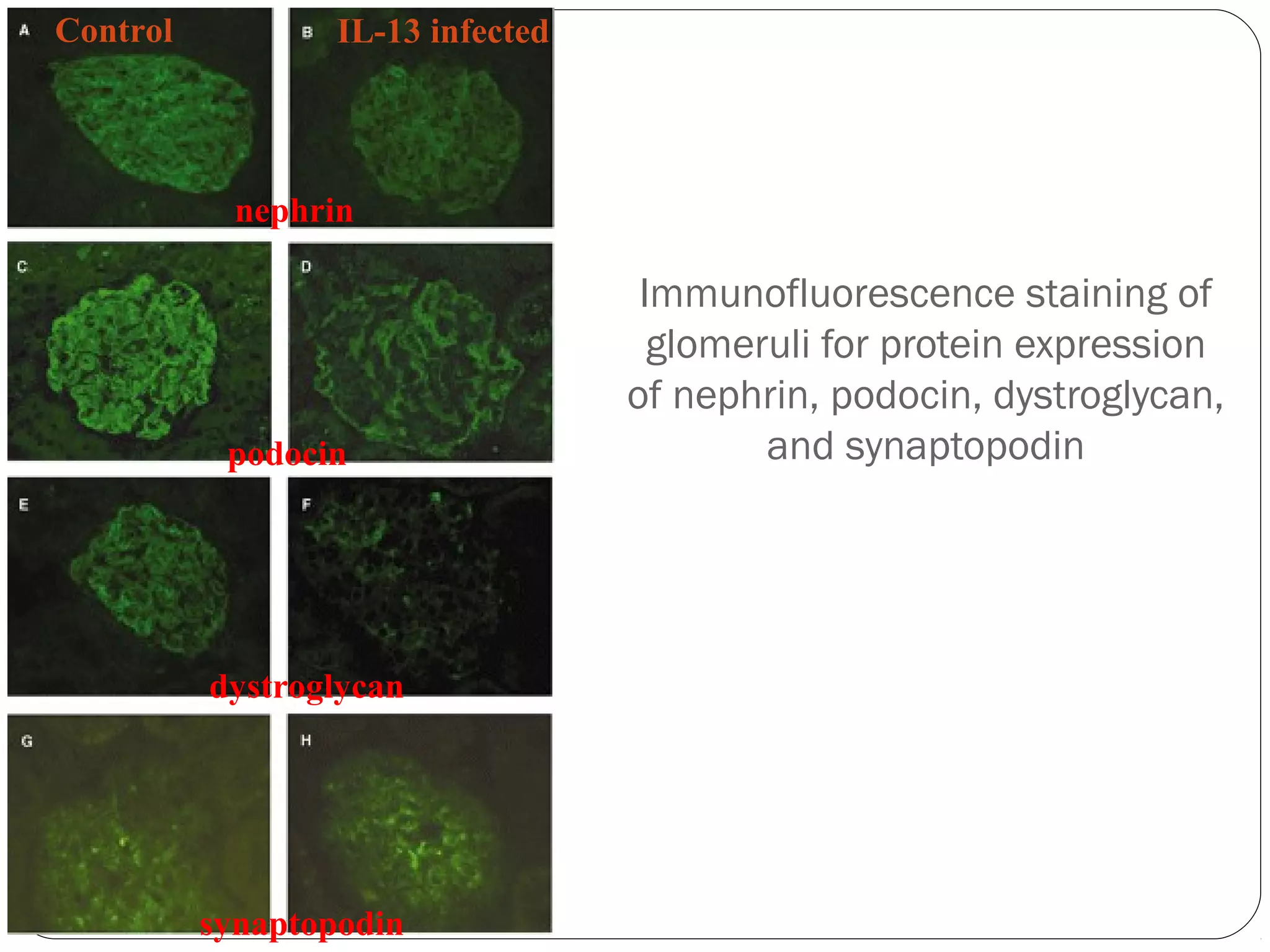
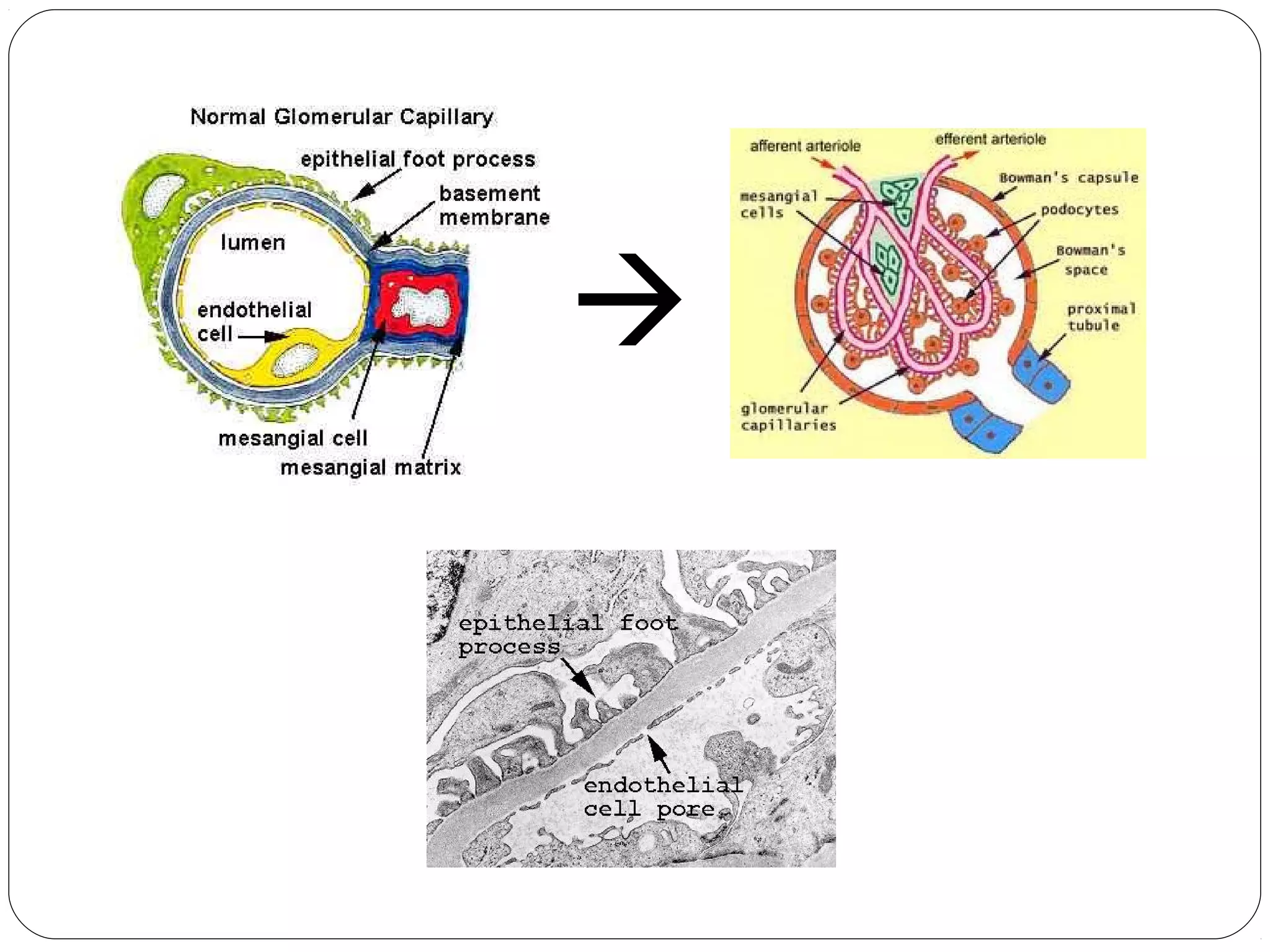
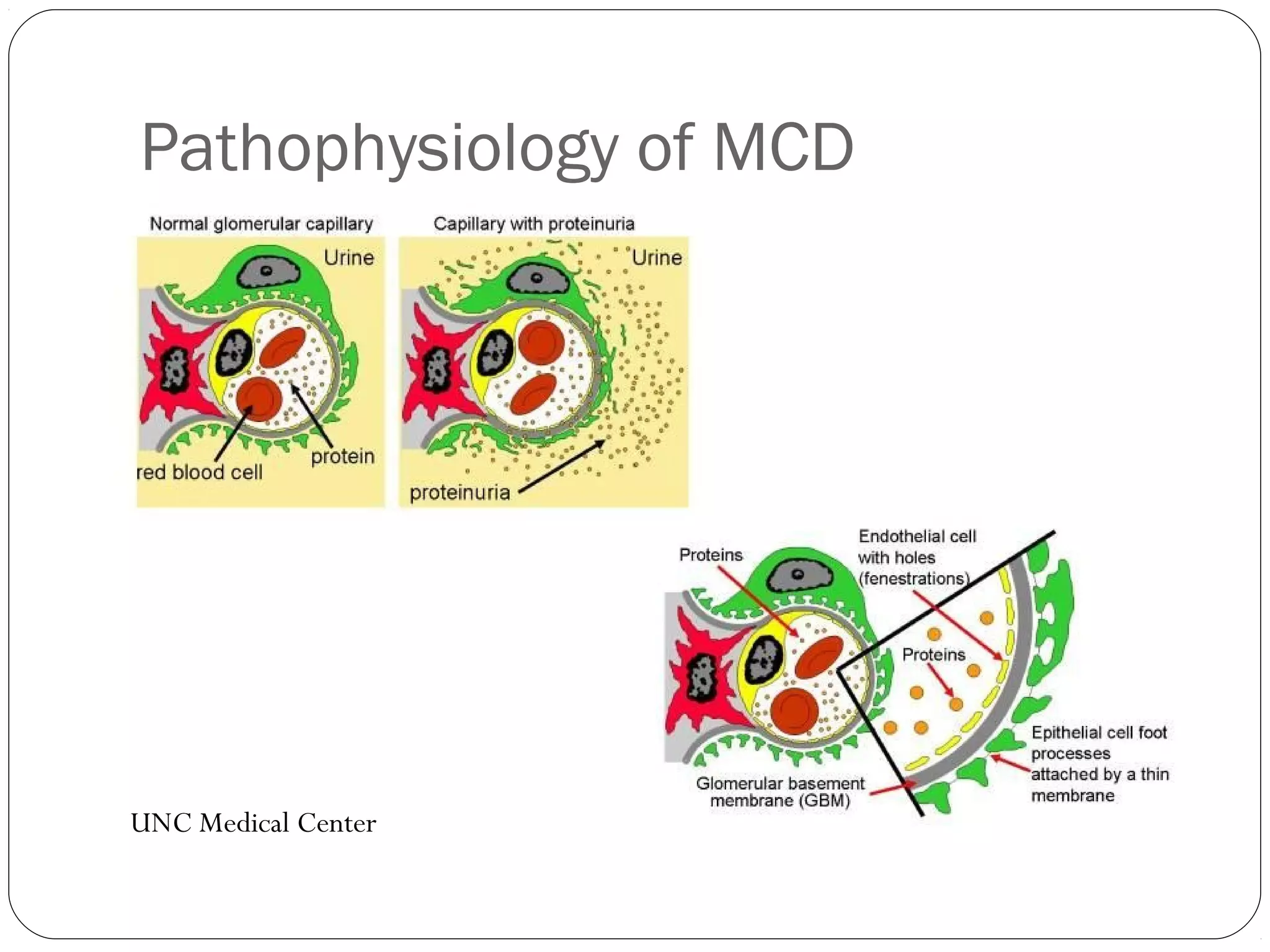
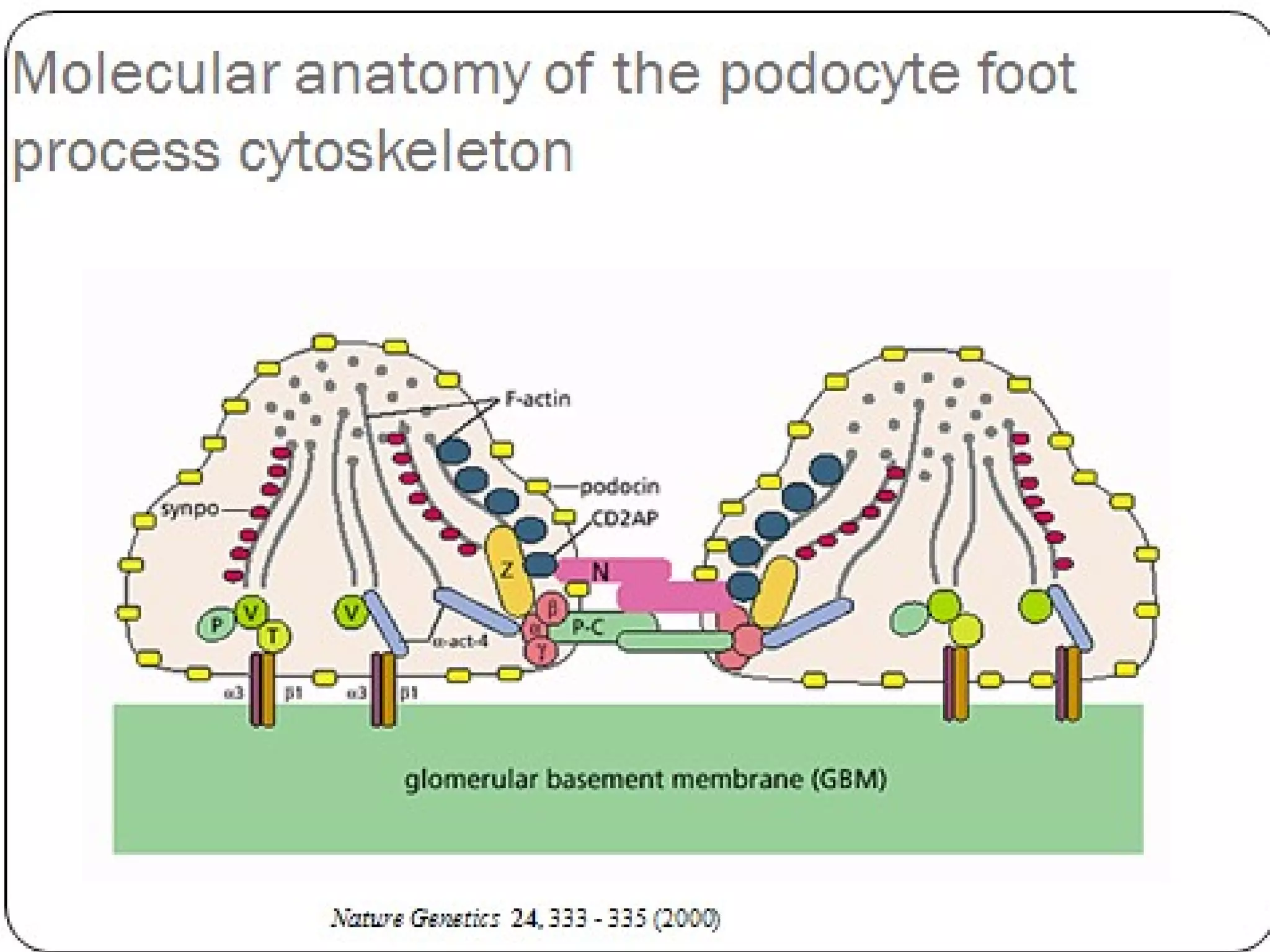
Minimal Change Disease (MCD) is a type of nephrotic syndrome characterized by proteinuria and swelling without significant findings on light microscopy. It is caused by a circulating permeability factor that leads to foot process effacement on electron microscopy. MCD is most common in children and responds well to steroid treatment, though relapses are common. Second line treatments include cyclophosphamide or rituximab if relapses are frequent or the patient is steroid dependent.