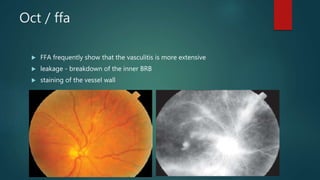
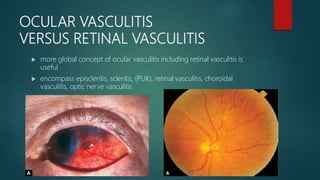
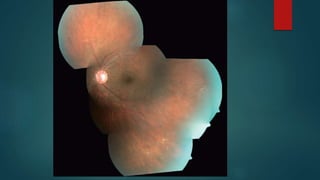
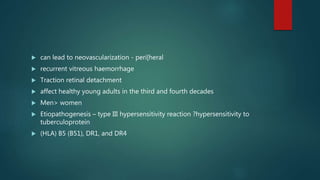
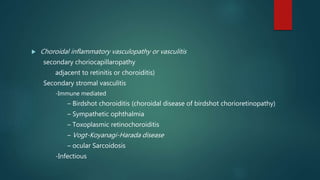
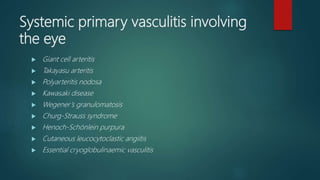
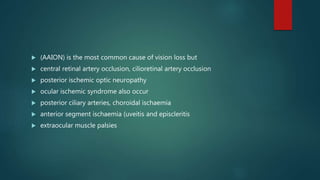
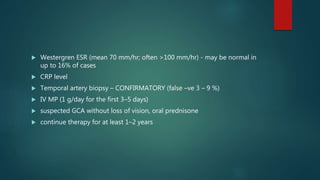
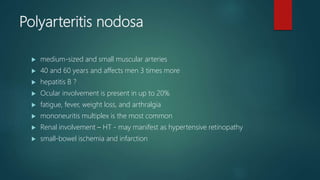
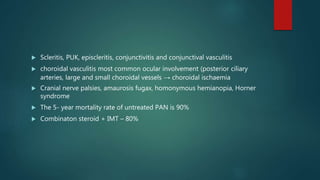
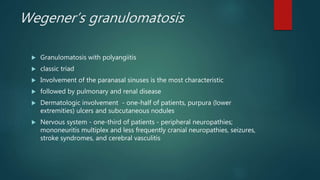
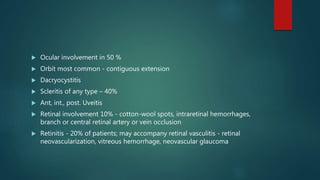
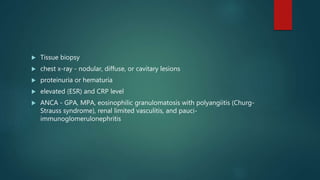
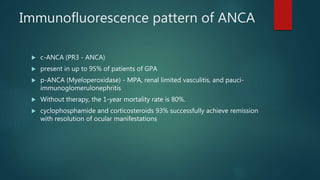
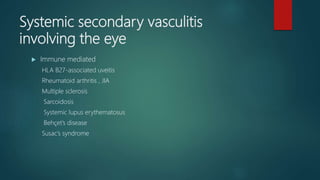
This document discusses various types of vasculitis and their ocular manifestations. It begins by describing the typical presentations of ocular vasculitis such as decreased vision, floaters, and scotomata. Imaging findings on fluorescein angiography and optical coherence tomography are also summarized. The document then differentiates between primary ocular vasculitis, secondary ocular vasculitis, and systemic vasculitis involving the eye. Specific conditions are outlined including Eale's disease, giant cell arteritis, Wegener's granulomatosis, and lupus retinopathy. Treatment options are briefly mentioned for some conditions.