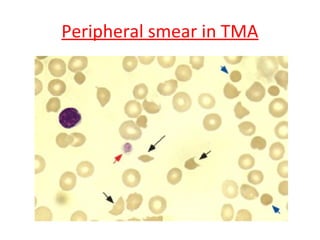
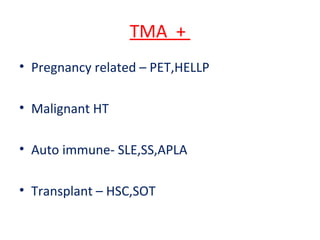
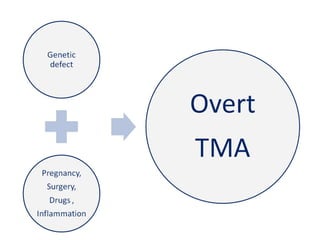
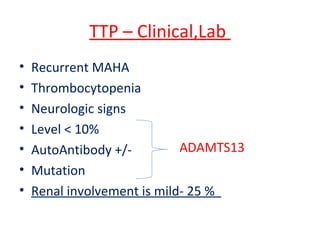
Thrombotic microangiopathy (TMA) is characterized by arteriolar and capillary lesions leading to microangiopathic hemolytic anemia, thrombocytopenia, and organ injury due to platelet-rich thrombi. The condition can be hereditary or acquired, affecting various age groups and organs, with multiple classifications evolving over time, including atypical HUS and TTP. Early diagnosis and prompt management, such as plasmapheresis and potential new treatments, are critical for patient survival and mitigating organ damage.
![Beginning of the story
• 1924
• Moschcowitz treats a 16 yr old girl
• Purpura, Pallor, hemiparesis
• Dies of cardiac failure
• Autopsy- Hyaline thrombi in microcirculation
incl. Kidneys
• ? TTP [ ADAMSTS13 Def.]
• More people studied it than suffered from it !](https://image.slidesharecdn.com/finalpune-150104113107-conversion-gate01/85/Thrombotic-Microangiopathy-3-320.jpg)

![TTP [ ADAMTS 13 defect ]
• ADAMTS13 is secreted from Liver
• Gene on chr.9q34
• Cleaves vWf multimers of vasc. Endoth
• If deficient – vWf are uncut and large
• Platelet thrombi in small vv. with high
shear states
Hereditary [Upshaw Schulman]
Homozy, compd het.of
ADAMTS 13
Acquired
Auto antibody inh.ADAMTS13
Females](https://image.slidesharecdn.com/finalpune-150104113107-conversion-gate01/85/Thrombotic-Microangiopathy-15-320.jpg)
![Management of Stx HUS
• Aggressive hydration with isotonic fluids
• Antibiotics – Warning ! [E.Coli. Infection]
• May increase Stx release
• Quinolones,TMP- Induce of Stx gene transcr.
• However , In Shigellosis – Early antibiotics
indicated
• Stx binder SYNSORB was not effective
• PEX or P.Infusion – Effective along with
Dialysis](https://image.slidesharecdn.com/finalpune-150104113107-conversion-gate01/85/Thrombotic-Microangiopathy-23-320.jpg)
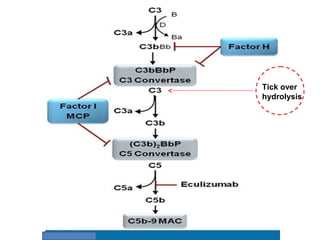
![Complement factors and TMA
[C-TMA]](https://image.slidesharecdn.com/finalpune-150104113107-conversion-gate01/85/Thrombotic-Microangiopathy-26-320.jpg)
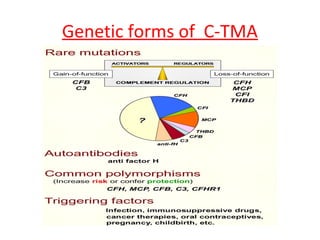
![Genetics of C-TMA
Missing Links
• Family members carrying same heterozygous
mutations are normal [ ? Modifier genes]
• SNP in CFH,CD46
• Copy No. variations in CFH1,3 Genes
• Fusion genes of CFHR and CFH due to
homologous recombination
• Normal plasma C3,C4,CFH,CFB,CFI does not
exclude C-HUS](https://image.slidesharecdn.com/finalpune-150104113107-conversion-gate01/85/Thrombotic-Microangiopathy-30-320.jpg)