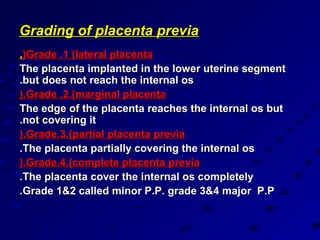
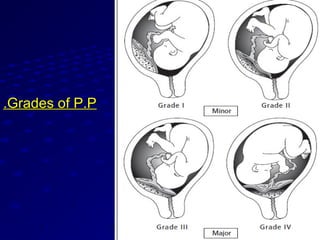
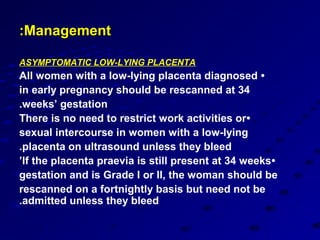
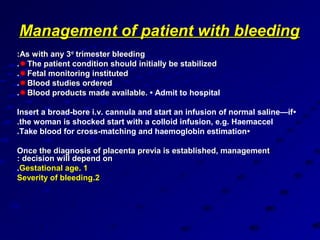
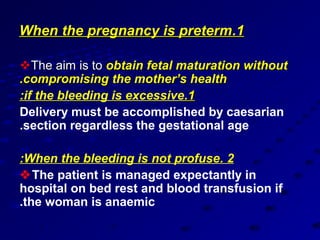
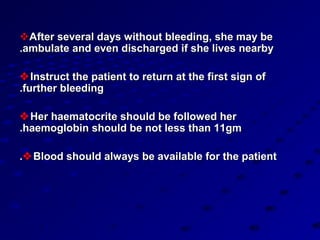
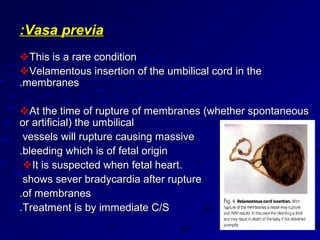
This document summarizes antepartum hemorrhage (APH), defined as bleeding in the third trimester between 24 weeks of pregnancy until delivery. Placenta previa, where the placenta covers all or part of the cervical os, is a major cause of APH, accounting for 30% of cases. Ultrasound is used to diagnose and grade placenta previa. Management depends on gestational age and bleeding severity, and may involve bed rest, blood transfusions, or caesarean section which is usually required for complete placenta previa. Complications of placenta previa include preterm birth, malpresentation, postpartum hemorrhage, and in rare cases